Effects of Docosahexaenoic Acid in Preventing Experimental Choroidal Neovascularization in Rodents
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Fatty Acid Diets: Regulation of Gut Microbiota Composition and Obesity and Its Related Metabolic Dysbiosis
International Journal of Molecular Sciences Review Fatty Acid Diets: Regulation of Gut Microbiota Composition and Obesity and Its Related Metabolic Dysbiosis David Johane Machate 1, Priscila Silva Figueiredo 2 , Gabriela Marcelino 2 , Rita de Cássia Avellaneda Guimarães 2,*, Priscila Aiko Hiane 2 , Danielle Bogo 2, Verônica Assalin Zorgetto Pinheiro 2, Lincoln Carlos Silva de Oliveira 3 and Arnildo Pott 1 1 Graduate Program in Biotechnology and Biodiversity in the Central-West Region of Brazil, Federal University of Mato Grosso do Sul, Campo Grande 79079-900, Brazil; [email protected] (D.J.M.); [email protected] (A.P.) 2 Graduate Program in Health and Development in the Central-West Region of Brazil, Federal University of Mato Grosso do Sul, Campo Grande 79079-900, Brazil; pri.fi[email protected] (P.S.F.); [email protected] (G.M.); [email protected] (P.A.H.); [email protected] (D.B.); [email protected] (V.A.Z.P.) 3 Chemistry Institute, Federal University of Mato Grosso do Sul, Campo Grande 79079-900, Brazil; [email protected] * Correspondence: [email protected]; Tel.: +55-67-3345-7416 Received: 9 March 2020; Accepted: 27 March 2020; Published: 8 June 2020 Abstract: Long-term high-fat dietary intake plays a crucial role in the composition of gut microbiota in animal models and human subjects, which affect directly short-chain fatty acid (SCFA) production and host health. This review aims to highlight the interplay of fatty acid (FA) intake and gut microbiota composition and its interaction with hosts in health promotion and obesity prevention and its related metabolic dysbiosis. -

Omega-3 Eicosapentaenoic Acid (EPA)
nutrients Article Omega-3 Eicosapentaenoic Acid (EPA) Rich Extract from the Microalga Nannochloropsis Decreases Cholesterol in Healthy Individuals: A Double-Blind, Randomized, Placebo-Controlled, Three-Month Supplementation Study Amanda Rao 1,2 , David Briskey 1,3, Jakob O Nalley 4 and Eneko Ganuza 4,* 1 RDC Clinical, Brisbane 4006, Australia; [email protected] (A.R.); [email protected] (D.B.) 2 School of Medicine, University of Sydney, Sydney, NSW 2006, Australia 3 School of Human Movement and Nutrition Sciences, The University of Queensland, Brisbane, QLD 4067, Australia 4 Qualitas Health, Houston, TX 77056, USA; [email protected] * Correspondence: [email protected] Received: 26 May 2020; Accepted: 20 June 2020; Published: 23 June 2020 Abstract: The aim of this trial is to assess the effect of Almega®PL on improving the Omega-3 Index, cardio-metabolic parameters, and other biomarkers in generally healthy individuals. The benefits of long-chain omega-3 fatty acids for cardiovascular health are primarily built upon mixtures of docosahexaenoic (DHA) and eicosapentaenoic acids (EPA). Highly purified EPA therapy has proven to be particularly effective in the treatment of cardiovascular disease, but less is known about the benefits of EPA-only supplementation for the general healthy population. Almega®PL is a polar rich oil (>15%) derived from the microalga Nannochloropsis that contains EPA (>25%) with no DHA. Participants (n = 120) were given a capsule of 1 g/day of either Almega®PL or placebo for 12 weeks. Differences in the Omega-3 Index, cardiometabolic markers, and other general health indicators were measured at the baseline, six, and 12 weeks. -

Compounds with Anti-Aging Activities
(19) TZZ ZZ_T (11) EP 2 862 600 A1 (12) EUROPEAN PATENT APPLICATION (43) Date of publication: (51) Int Cl.: 22.04.2015 Bulletin 2015/17 A61Q 19/08 (2006.01) A61K 8/49 (2006.01) A61K 8/36 (2006.01) A61K 8/44 (2006.01) (2006.01) (2006.01) (21) Application number: 14196664.8 A61K 8/63 A61K 8/64 A61K 8/33 (2006.01) A61K 8/60 (2006.01) (2006.01) (2006.01) (22) Date of filing: 20.12.2011 A61Q 17/04 A61K 8/42 A61Q 1/02 (2006.01) A61Q 19/00 (2006.01) A61Q 19/02 (2006.01) A61Q 19/04 (2006.01) A61Q 19/10 (2006.01) A61K 31/11 (2006.01) A61K 31/197 (2006.01) A61K 31/202 (2006.01) A61K 31/343 (2006.01) A61K 31/353 (2006.01) A61K 31/704 (2006.01) (84) Designated Contracting States: • Mavon, Alain Robert Pierre AL AT BE BG CH CY CZ DE DK EE ES FI FR GB 11264 Stockholm (SE) GR HR HU IE IS IT LI LT LU LV MC MK MT NL NO • Duracher, Lucie PL PT RO RS SE SI SK SM TR 11761 Stockholm (SE) Designated Extension States: • Klack, Anke BA ME 11244 Stockholm (SE) • Cattley, Kevin (62) Document number(s) of the earlier application(s) in Wexford (IE) accordance with Art. 76 EPC: 11797020.2 / 2 729 220 (74) Representative: Moore, Michael Richard et al Keltie LLP (71) Applicant: Oriflame Research and Development No.1 London Bridge Ltd. London SE1 9BA (GB) Bray, Co. Wicklow (IE) Remarks: (72) Inventors: This application was filed on 05-12-2014 as a • Gillbro, Johanna Maria divisional application to the application mentioned 11736 Stockholm (SE) under INID code 62. -
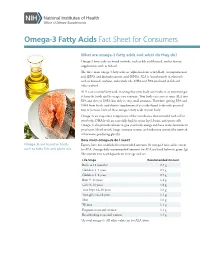
Omega-3 Fatty Acids Fact Sheet for Consumers
Omega-3 Fatty Acids Fact Sheet for Consumers What are omega-3 fatty acids and what do they do? Omega-3 fatty acids are found in foods, such as fish and flaxseed, and in dietary supplements, such as fish oil. The three main omega-3 fatty acids are alpha-linolenic acid (ALA), eicosapentaenoic acid (EPA), and docosahexaenoic acid (DHA). ALA is found mainly in plant oils such as flaxseed, soybean, and canola oils. DHA and EPA are found in fish and other seafood. ALA is an essential fatty acid, meaning that your body can’t make it, so you must get it from the foods and beverages you consume. Your body can convert some ALA into EPA and then to DHA, but only in very small amounts. Therefore, getting EPA and DHA from foods (and dietary supplements if you take them) is the only practical way to increase levels of these omega-3 fatty acids in your body. Omega-3s are important components of the membranes that surround each cell in your body. DHA levels are especially high in retina (eye), brain, and sperm cells. Omega-3s also provide calories to give your body energy and have many functions in your heart, blood vessels, lungs, immune system, and endocrine system (the network of hormone-producing glands). How much omega-3s do I need? Omega-3s are found in foods Experts have not established recommended amounts for omega-3 fatty acids, except such as fatty fish and plant oils. for ALA. Average daily recommended amounts for ALA are listed below in grams (g). -

Revealing the Role of Short Chain and Polyunsaturated Fatty Acids As
Southern Illinois University Carbondale OpenSIUC Honors Theses University Honors Program 2019 Revealing the Role of Short Chain and Polyunsaturated Fatty Acids as Regulators of Metabolic Activity and Gene Expression in Ovarian Cancer Abigayle Ochs [email protected] Follow this and additional works at: https://opensiuc.lib.siu.edu/uhp_theses Recommended Citation Ochs, Abigayle, "Revealing the Role of Short Chain and Polyunsaturated Fatty Acids as Regulators of Metabolic Activity and Gene Expression in Ovarian Cancer" (2019). Honors Theses. 461. https://opensiuc.lib.siu.edu/uhp_theses/461 This Dissertation/Thesis is brought to you for free and open access by the University Honors Program at OpenSIUC. It has been accepted for inclusion in Honors Theses by an authorized administrator of OpenSIUC. For more information, please contact [email protected]. REVEALING THE ROLE OF SHORT CHAIN AND POLYUNSATURATED FATTY ACIDS AS REGULATORS OF METABOLIC ACTIVITY AND GENE EXPRESSION IN OVARIAN CANCER Abigayle Ochs A thesis submitted to the University Honors Program in partial fulfillment of the requirements for the Honors Certificate with Thesis Southern Illinois University Carbondale May 2019 Ochs 2 I. Abstract Previous research using the chicken model has provided evidence that a flaxseed- supplemented diet decreases both the severity and the incidence of ovarian cancer. Flaxseed is a source of omega-3 (OM3) polyunsaturated fatty acids (PUFA), particularly α-linolenic acid (ALA). ALA is converted into longer chain OM3s, eicosapentaenoic acid (EPA) and docosahexaenoic acid (DHA), which inhibit prostaglandins, thereby inhibiting oxidative stress, inflammation, angiogenesis, and proliferation. The dietary fiber component of flaxseed can be fermented in the gut to produce short chain fatty acids (SCFA). -

Omega-3, Omega-6 and Omega-9 Fatty Acids
Johnson and Bradford, J Glycomics Lipidomics 2014, 4:4 DOI: 0.4172/2153-0637.1000123 Journal of Glycomics & Lipidomics Review Article Open Access Omega-3, Omega-6 and Omega-9 Fatty Acids: Implications for Cardiovascular and Other Diseases Melissa Johnson1* and Chastity Bradford2 1College of Agriculture, Environment and Nutrition Sciences, Tuskegee University, Tuskegee, Alabama, USA 2Department of Biology, Tuskegee University, Tuskegee, Alabama, USA Abstract The relationship between diet and disease has long been established, with epidemiological and clinical evidence affirming the role of certain dietary fatty acid classes in disease pathogenesis. Within the same class, different fatty acids may exhibit beneficial or deleterious effects, with implications on disease progression or prevention. In conjunction with other fatty acids and lipids, the omega-3, -6 and -9 fatty acids make up the lipidome, and with the conversion and storage of excess carbohydrates into fats, transcendence of the glycome into the lipidome occurs. The essential omega-3 fatty acids are typically associated with initiating anti-inflammatory responses, while omega-6 fatty acids are associated with pro-inflammatory responses. Non-essential, omega-9 fatty acids serve as necessary components for other metabolic pathways, which may affect disease risk. These fatty acids which act as independent, yet synergistic lipid moieties that interact with other biomolecules within the cellular ecosystem epitomize the critical role of these fatty acids in homeostasis and overall health. This review focuses on the functional roles and potential mechanisms of omega-3, omega-6 and omega-9 fatty acids in regard to inflammation and disease pathogenesis. A particular emphasis is placed on cardiovascular disease, the leading cause of morbidity and mortality in the United States. -

Breast Milk Docosahexaenoic Acid (DHA) Correlates with DHA Status Of
Arch Dis Child 2000;82:493–494 493 Breast milk docosahexaenoic acid (DHA) correlates Arch Dis Child: first published as 10.1136/adc.82.6.493 on 1 June 2000. Downloaded from with DHA status of malnourished infants Ella N Smit, Esther A Oelen, Ejaz Seerat, Frits A J Muskiet, E Rudy Boersma Abstract ished, mostly breast fed, 4–56 month old chil- Aim—To investigate whether low docosa- dren, living in and around Islamabad, North hexaenoic acid (22:6ù3; DHA) status of Pakistan.3 malnourished, mostly breast fed infants is We hypothesised that the low RBC DHA a result of low ù3 fatty acid intake via content in these infants was a result of low breast milk. ù3-LCPUFA intake via breast milk. In an Methods—Fatty acid composition of attempt to test this hypothesis we studied the breast milk of eight Pakistani mothers, FA composition of both the breast milk of eight and of the erythrocytes of their malnour- Pakistani mothers and that of the RBC of their ished children was analysed. malnourished children. Results—The milk of the Pakistani moth- ers contained low percentages of all ù3 Subjects and methods and most ù6 fatty acids, compared with The study population consisted of eight milk of Dutch mothers. Breast milk DHA mother–child pairs from a low socioeconomic was positively correlated with infant class. They were recruited from the Nutrition erythrocyte DHA and arachidonic acid Rehabilitation Center of the Pediatric Depart- (20:4ù6). ment, Federal Government Services Hospital, Conclusion—DHA status of these mal- Islamabad. The children were classified as nourished children is strongly dependent malnourished, defined as weight for age below on the ù3 fatty acid intake from breast the mean minus 2SD, according to WHO milk. -

Vitamins and Healthy Skin Zoe Diana Draelos, MD
COSMETIC CONSULTATION Vitamins and Healthy Skin Zoe Diana Draelos, MD he term nutricosmetic combines the words nutri- to prevent vitamin D deficiency.1 Vitamin D deficiency, tion and cosmetic. Many of the new food intro- the cause of rickets in children, was virtually eliminated T ductions at the grocery store are nutricosmetics. when milk was enriched with 400 IU vitamin D per quart For example, milk is enriched with vitamin D whereas in the 1930s. One cup of milk supplies 25% of the recom- yogurt is not. However, a new line of yogurt contains mended daily allowance of vitamin D in adults; however, both vitamin D and inulin, a nonabsorbable fiber to aid it is probable that the current recommended daily allow- elimination. A competing yogurt brand contains probiotic ances are too low.2 Two hundred IU are recommended organisms, which are bacteria designed to recolonize the daily from birth to age 50 years; 400 IU from age 51 to gut, resulting in improved elimination and better overall 70 years; and 600 IU from age 71 years and older.3 health from the inside out. Adding nutrients is an impor- It is important to recognize that only milk is enriched tant marketing tactic because it allows existing foods to with vitamin D. Cheese, yogurt, and ice cream are not be made new with the addition of one ingredient. An required to include vitamin D; however, a new trend in existing food with decreasing sales can be reinvigorated some nutricosmetic yogurts, mentioned previously, is to in the marketplace with littleCOS upfront cost. -

The Effects of Omega-3 Fatty Acid Supplementation in Pregnancy on Maternal Eicosanoid, Cytokine, and Chemokine Secretion
0031-3998/09/6602-0212 Vol. 66, No. 2, 2009 PEDIATRIC RESEARCH Printed in U.S.A. Copyright © 2009 International Pediatric Research Foundation, Inc. The Effects of Omega-3 Fatty Acid Supplementation in Pregnancy on Maternal Eicosanoid, Cytokine, and Chemokine Secretion KRISTINA WARSTEDT, CATRIN FURUHJELM, KAREL DUCHE´ N, KARIN FA¨ LTH-MAGNUSSON, AND MALIN FAGERÅS Department of Clinical and Experimental Medicine [K.W., C.F., K.D., K.F.-M., M.F.], Clinical and Experimental Research [K.W., M.F.], Linko¨ping University, Linko¨ping, Sweden ABSTRACT: The incidence of allergic diseases has increased, and i.e. eicosapentaenoic acid (EPA) and docosahexaenoic acid a relation between allergy and dietary fatty acids has been proposed. (DHA), may dampen the proinflammatory effects of AA at Modulation of the maternal immune function during pregnancy may multiple levels (3). -3 LCPUFA supplementation may result have an impact on future clinical outcomes in the child. The aim of in decreased production of AA-derived eicosanoids (3) and this study was to determine the effects of omega ( )-3 long-chain has been reported to decrease lipopolysaccharide (LPS)- polyunsaturated fatty acids (LCPUFA) supplementation during preg- induced interleukin (IL)-1, IL-6, and tumor necrosis factor nancy on the plasma fatty acid composition in relation to the maternal immune function. Pregnant women with allergic disease in their (TNF) production by mononuclear cells (5). immediate family were supplemented daily with 2.7 g -3 LCPUFA Epidemiologic studies suggest that the period from early (n ϭ 70) or 2.8 g soybean oil as placebo (n ϭ 75) from the 25th fetal life to about3yofageisthemost critical time period for gestational week. -

Retinoid X Receptor Activation Is Essential for Docosahexaenoic Acid Protection of Retina Photoreceptors
Retinoid X receptor activation is essential for docosahexaenoic acid protection of retina photoreceptors 1 1 Olga L. German , Sandra Monaco , Daniela L. Agnolazza , Nora P. Rotstein , and Luis E. Politi Instituto de Investigaciones Bioquímicas de Bahía Blanca, Universidad Nacional del Sur-CONICET , Buenos Aires, Argentina Downloaded from Abstract We have established that docosahexaenoic acid retinitis pigmentosa and age-related macular degeneration. (DHA), the major polyunsaturated fatty acid in the retina, Photoreceptor loss in these pathologies occurs by apopto- promotes survival of rat retina photoreceptors during early sis and oxidative stress, and lack of trophic factors is impli- development in vitro and upon oxidative stress by activating cated in the activation of the apoptotic mechanisms ( 1 ). the ERK/MAPK signaling pathway. Here we have investi- Identifying the trophic factors and intracellular pathways gated whether DHA turns on this pathway through activa- www.jlr.org tion of retinoid X receptors (RXRs) or by inducing tyrosine activated to prevent this apoptosis is crucial for designing kinase (Trk) receptor activation. We also evaluated whether procedures to rescue photoreceptors in these diseases. DHA release from phospholipids was required for its pro- Previous research from our laboratory has demonstrated tective effect. Addition of RXR antagonists (HX531, PA452) that docosahexaenoic acid (DHA), the major n-3 polyun- at Univ of Oklahoma R M Bird Hlth Sci Lib, on July 10, 2013 to rat retinal neuronal cultures inhibited DHA protection saturated fatty acid (PUFA) in the retina, acts as a trophic during early development in vitro and upon oxidative stress factor for photoreceptor cells. DHA promotes differentia- induced with Paraquat or H 2 O2 . -

Utilization of Volatile Fatty Acids from Microalgae for the Production of High Added Value Compounds
fermentation Review Utilization of Volatile Fatty Acids from Microalgae for the Production of High Added Value Compounds Angelina Chalima 1, Laura Oliver 2, Laura Fernández de Castro 2, Anthi Karnaouri 1, Thomas Dietrich 2 and Evangelos Topakas 1,3,* ID 1 IndBioCat group, Biotechnology Laboratory, School of Chemical Engineering, National Technical University of Athens, 5 Iroon Polytechniou Str., Zografou Campus,15780 Athens, Greece; [email protected] (A.C.); [email protected] (A.K.) 2 Food & Health Group, Health Division, Tecnalia Research & Innovation, Parque Tecnológico de Álava, Leonardo Da Vinci, 11, E-01510 Miñano-Álava, Spain; [email protected] (L.O.); [email protected] (L.F.d.C.); [email protected] (T.D.) 3 Biochemical and Chemical Process Engineering, Division of Sustainable Process Engineering, Department of Civil Environmental and Natural Resources Engineering, Luleå University of Technology, SE-97187 Luleå, Sweden * Correspondence: [email protected]; Tel.: +30-210-772-3264 Received: 9 September 2017; Accepted: 9 October 2017; Published: 15 October 2017 Abstract: Volatile Fatty Acids (VFA) are small organic compounds that have attracted much attention lately, due to their use as a carbon source for microorganisms involved in the production of bioactive compounds, biodegradable materials and energy. Low cost production of VFA from different types of waste streams can occur via dark fermentation, offering a promising approach for the production of biofuels and biochemicals with simultaneous reduction of waste volume. VFA can be subsequently utilized in fermentation processes and efficiently transformed into bioactive compounds that can be used in the food and nutraceutical industry for the development of functional foods with scientifically sustained claims. -
EPA/DHA and Vitamin a Supplementation Improves Spatial Memory and Alleviates the Age-Related Decrease in Hippocampal Rxrγ and Kinase Expression in Rats
fnagi-08-00103 May 5, 2016 Time: 16:44 # 1 ORIGINAL RESEARCH published: 09 May 2016 doi: 10.3389/fnagi.2016.00103 EPA/DHA and Vitamin A Supplementation Improves Spatial Memory and Alleviates the Age-related Decrease in Hippocampal RXRg and Kinase Expression in Rats Anne Létondor1,2,3,4, Benjamin Buaud4, Carole Vaysse4, Emmanuel Richard5, Sophie Layé1,2, Véronique Pallet1,2,3† and Serge Alfos1,2,3*† 1 Université de Bordeaux, Nutrition et Neurobiologie Intégrée, UMR 1286, Bordeaux, France, 2 INRA, Nutrition et Neurobiologie Intégrée, UMR 1286, Bordeaux, France, 3 Bordeaux INP, Nutrition et Neurobiologie Intégrée, UMR 1286, Bordeaux, France, 4 ITERG, Institut des Corps Gras, Pessac, France, 5 INSERM, Biothérapie des Maladies Génétiques Inflammatoires et Cancers, U1035, Bordeaux, France Edited by: Elizabeth J. Johnson, Studies suggest that eicosapentaenoic acid (EPA), docosahexaenoic acid (DHA), and Tufts University, USA vitamin A are critical to delay aged-related cognitive decline. These nutrients regulate Reviewed by: gene expression in the brain by binding to nuclear receptors such as the retinoid Kathy R. Magnusson, X receptors (RXRs) and the retinoic acid receptors (RARs). Moreover, EPA/DHA and Oregon State University, USA Cathy W. Levenson, retinoids activate notably kinase signaling pathways such as AKT or MAPK, which Florida State University College includes ERK1/2. This suggests that these nutrients may modulate brain function in a of Medicine, USA Simon C. Dyall, similar way. Therefore, we investigated in middle-aged rats the behavioral and molecular Bournemouth University, UK effects of supplementations with EPA/DHA and vitamin A alone or combined. 18-month- *Correspondence: old rats exhibited reference and working memory deficits in the Morris water maze, Serge Alfos associated with a decrease in serum vitamin A and hippocampal EPA/DHA contents.