Piebaldism in Children
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
July 2020 Goal the Goal of the Residency Program Is to Develop Future Leaders in Both Research and Clinical Medicine
Residency Training Program July 2020 Goal The goal of the Residency Program is to develop future leaders in both research and clinical medicine. Flexibility within the program allows for the acquisition of fundamental working knowledge in all subspecialties of dermatology. All residents are taught a scholarly approach to patient care, aimed at integrating clinicopathologic observation with an understanding of the basic pathophysiologic processes of normal and abnormal skin. Penn’s Residency Program consists of conferences, seminars, clinical rotations, research, and an opportunity to participate in the teaching of medical students. An extensive introduction into the department and the William D. James, M.D. Director of Residency Program clinic/patient care service is given to first-year residents. A distinguished clinical faculty and research faculty, coupled with the clinical and laboratory facilities, provides residents with comprehensive training. An appreciation of and participation in the investigative process is an integral part of our residency. Graduates frequently earn clinical or basic science fellowship appointments at universities across the country. Examples of these include: pediatric dermatology, dermatopathology, dermatologic surgery, dermatoepidemiology, postdoctoral and Clinical Educator fellowships. Additional post graduate training has occurred at the NIH and CDC. Graduates of our program populate the faculty at Harvard, Penn, Johns Hopkins, MD Anderson, Dartmouth, Penn State, Washington University, and the Universities of Washington, Pittsburgh, Vermont, South Carolina, Massachusetts, Wisconsin, and the University of California San Francisco. Additionally, some enter private practice to become pillars of community medicine. Misha A. Rosenbach, M.D. Associate Director of Residency Program History The first medical school in America, founded in 1765, was named the College of Philadelphia. -

Update on Challenging Disorders of Pigmentation in Skin of Color Heather Woolery-Lloyd, M.D
Update on Challenging Disorders of Pigmentation in Skin of Color Heather Woolery-Lloyd, M.D. Director of Ethnic Skin Care Voluntary Assistant Professor Miller/University of Miami School of Medicine Department of Dermatology and Cutaneous Surgery What Determines Skin Color? What Determines Skin Color? No significant difference in the number of melanocytes between the races 2000 epidermal melanocytes/mm2 on head and forearm 1000 epidermal melanocytes/mm2 on the rest of the body differences present at birth Jimbow K, Quevedo WC, Prota G, Fitzpatrick TB (1999) Biology of melanocytes. In I. M. Freedberg, A.Z. Eisen, K. Wolff,K.F. Austen, L.A. Goldsmith, S. I. Katz, T. B. Fitzpatrick (Eds.), Dermatology in General Medicine 5th ed., pp192-220, New York, NY: McGraw Hill Melanosomes in Black and White Skin Black White Szabo G, Gerald AB, Pathak MA, Fitzpatrick TB. Nature1969;222:1081-1082 Jimbow K, Quevedo WC, Prota G, Fitzpatrick TB (1999) Biology of melanocytes. In I. M. Freedberg, A.Z. Eisen, K. Wolff, K.F. Austen, L.A. Goldsmith, S. I. Katz, T. B. Fitzpatrick (Eds.), Dermatology in General Medicine 5th ed., pp192- 220, New York, NY: McGraw Hill Role of Melanin-Advantages Melanin absorbs and scatters energy from UV and visible light to protect epidermal cells from UV damage Disadvantages Inflammation or injury to the skin is almost immediately accompanied by alteration in pigmentation Hyperpigmentation Hypopigmentation Dyschromias Post-Inflammatory hyperpigmentation Acne Melasma Lichen Planus Pigmentosus Progressive Macular Hypomelanosis -

General Dermatology Practice Brochure
Appointments Our Providers David A. Cowan, MD, FAAD We are currently accepting • Fellow, American Academy of Dermatology new patients. • Associate, American College of Call today to schedule your appointment Mohs Micrographic Surgery Monday - Friday, 8:00am to 4:30pm Rebecca G. Pomerantz, MD 1-877-661-3376 • Board Certified, American Academy of Cancellations & “No Show” Policy Dermatology If you are unable to keep your scheduled Lisa L. Ellis, MPAS, PA-C appointment, please call the office and we will • Member, American Academy of Physician be more than happy to reschedule for you. Assistants Failure to notify us at least 48 hours prior to your • Member, PA Society of Physician Assistants Medical and appointment may result in a cancellation fee. • Member, Society of Dermatology Physician Prescription Refills Assistants Surgical Refill requests are handled during normal office Sheri L. Rolewski, MSN, CRNP-BC hours when our staff has full access to medical • National Board Certification, Family Nurse Dermatology records. Refills cannot be called in on holidays, Practitioner Specialty weekends or more than twelve months after your • Member, Dermatology Nurse Association last exam. Please have your pharmacy contact our office directly. Test Results SMy Dermatology Appointment You will be notified when we receive your Date/Day _____________________________________ pathology or other test results, usually within two weeks from the date of your procedure. If you Time _________________________________________ do not hear from us within three -

Generalized Hypertrichosis
Letters to the Editor case of female. Ambras syndrome is a type of universal Generalized hypertrichosis affecting the vellus hair, where there is uniform overgrowth of hair over the face and external hypertrichosis ear with or without dysmorphic facies.[3] Patients with Gingival fi bromaatosis also have generalized hypertrichosis Sir, especially on the face.[4] Congenital hypertrichosis can A 4-year-old girl born out of non-consanguinous marriage occur due to fetal alcohol syndrome and fetal hydentoin presented with generalized increase in body hair noticed syndrome.[5] Prepubertal hypertrichosis is seen in otherwise since birth. None of the other family members were healthy infants and children. There is involvement of affected. Hair was pigmented and soft suggesting vellus hair. face back and extremities Distribution of hair shows an There was generalized increase in body hair predominantly inverted fi r-tree pattern on the back. More commonly seen affecting the back of trunk arms and legs [Figures 1 and 2]. in Mediterranean and South Asian descendants.[6] There is Face was relatively spared except for fore head. Palms and soles were spared. Scalp hair was normal. Teeth and nail usually no hormonal alterations. Various genodermatosis were normal. There was no gingival hypertrophy. No other associated with hypertrichosis as the main or secondary skeletal or systemic abnormalities were detected clinically. diagnostic symptom are: Routine blood investigations were normal. Hormonal Lipoatrophy (Lawrernce Seip syndrome) study was within normal limit for her age. With this Cornelia de Lange syndrome clinical picture of generalized hypertrichosis with no other Craniofacial dysostosis associated anomalies a diagnosis of universal hypertrichosis Winchester syndrome was made. -

Dermatology at the Berkeley Outpatient Center
Dermatology Berkeley Outpatient Center Overview Encompassing both medical and cosmetic dermatology, our experts at the Berkeley Outpatient Center offer a full range of diagnostic, treatment and surgical services for patients with cutaneous conditions. Surgical Dermatology • Fellowship-trained expertise in • Close coordination with Plastic Surgery Mohs micrographic surgery for at the Berkeley Outpatient Center, treatment of skin cancers including allowing for streamlined treatment for basal cell carcinomas and squamous related procedures in one location cell carcinomas, as well as treatment of • Outpatient surgery for removal of melanoma in situ with MART-1 staining benign skin growths and skin cancers Medical Dermatology - Conditions Treated/Services Offered • Acne, rosacea and related conditions • Mole/Atypical nevus/Melanoma • Sun-damaged skin surveillance • Aesthetic/Cosmetic dermatology • Non-melanoma skin cancers • Eczema and atopic dermatitis • Pigmentation disorders • HIV/AIDS-related skin conditions • Psoriasis • Lumps under the skin • Rashes • Infections of the skin (bacterial, viral, • Skin checks for patients with fungal and other) concerning lesions • Melanoma • Warts When to see a Dermatologist For more information, please call Dermatology Services at (510) 985-5200. Dermatology Services Providing integrated care in the community. Our Dermatology Team Erin Amerson, MD Drew Saylor, MD, MPH UCSF Health UCSF Health Dermatologist Dermatologic surgeon To learn more about our doctors, visit ucsfhealth.org/find_a_doctor. Office location: Berkeley Outpatient Center 3100 San Pablo Avenue Berkeley, CA 94702 (510) 985-5200 To learn more about our Berkeley Outpatient Center, Adeline St visit johnmuirhealth.com/ September 2020 berkeleyopc.. -

Iris Mammillations: Significance and Associations
IRIS MAMMILLATIONS: SIGNIFICANCE AND ASSOCIATIONS 2 l NICOLA K. RAGGEL2, 1. ACHESON and A. LINN MURPHREE Los Angeles and London SUMMARY mammiform (nipple- or teat-like) protuberances. Iris mammillations are rarely described, distinctive Iris mammillations are an occasional finding with few previous reports. They are most commonly villiform protuberances that can cover the iris. In the l--6 majority of reported cases they are unilateral and found in association with melanosis oculi, with or sporadic, and are seen in association with oculodermal without periocular skin involvement in a naevus of melanosis. In past literature and current clinical Ota. They are thus often less precisely referred to as practice they are frequently confused with tbe iris iris melanosis, a term which should best be reserved nodules seen in neurofibromatosis type 1. Their clinical for increased pigmentation of the iris, irrespective of significance is not established, although it has been the presence of iris elevations overlying the pigmen 7 suggested that iris mammillations may be an external ted areas. This is supported by the rare descriptions sign of ocular hypertension or intraocular malignancy. of iris elevations in the absence of any increased iris We report a series of 9 patients between the ages of 3 pigmentation?,8 and 28 years with iris mammillations. The mammilla Iris mammillations are usually unilateral, often tions appear as regularly spaced, deep brown, smooth, presenting as heterochromia iridis. Occasional bilat 7 conical elevations on the iris, of uniform height or eral cases have been described. ,8 Iris mammillations increasing in height as the pupil margin is approached. -

Unexplained White Spots on Your Skin Could Be Caused by Aging
Unexplained White Spots on Your Skin Could Be Caused by Aging By GERRIE SUMMERS. June 12, 2019 Many of us take great pains to make sure our skin is clear and pristine. (At Byrdie HQ, we've got the robust skincare regimens to prove it.) So, anytime something out of the ordinary pops up that we don't automatically know how to deal with, things can reach panic mode pretty quickly. For example, age spots. And we're not just talking about dark sunspots; we've got a pretty good handle on those. We're talking little white spots, which can look a bit like confetti or white freckles. "It is a little- known fact that sun damage causes not only brown spots, but also white spots," says Dr. Anna Guanche, board-certified dermatologist and celebrity beauty expert at Bella Skin Institute. "I liken them to 'gray hairs' in the skin." More than likely, these are a result of a harmless condition called Idiopathic Guttate Hypomelanosis (IGH). "IGH is a skin condition characterized by multiple round [or] oval white spots that are usually flat. It is very commonly found on the arms and legs of patients over 50," says Dr. Marla Diakow of Schweiger Dermatology Group in Garden City, NY. "[It's] a completely benign entity, but often one of cosmetic concern to patients." These white spots occur due to localized loss of pigmentation of the skin. Read on to get the full scoop on this condition and how it can be treated. How to Treat IGH If you begin to notice unexplained white spots, you should visit your dermatologist ASAP to rule out other conditions that have similar characteristics. -
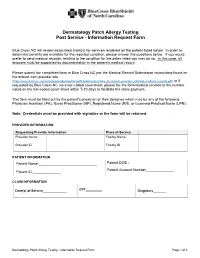
Dermatology Patch Allergy Testing Post Service - Information Request Form
Dermatology Patch Allergy Testing Post Service - Information Request Form Blue Cross NC will review associated claim(s) for services rendered on the patient listed below. In order to determine benefits are available for the reported condition, please answer the questions below. If you would prefer to send medical records, relating to the condition for the dates listed you may do so. In this case, all answers must be supported by documentation in the patient's medical record. Please submit the completed form to Blue Cross NC per the Medical Record Submission instructions found on the bcbsnc.com provider site (https://www.bcbsnc.com/assets/providers/public/pdfs/submissions/how_to_submit_provider_initiated_medical_records.pdf) or if requested by Blue Cross NC via a bar-coded coversheet, please fax the form/medical records to the number noted on the bar-coded cover sheet within 7-10 days to facilitate the claim payment. This form must be filled out by the patient's physician or their designee which may be any of the following: Physician Assistant (PA), Nurse Practitioner (NP), Registered Nurse (RN), or Licensed Practical Nurse (LPN). Note: Credentials must be provided with signature or the form will be returned. PROVIDER INFORMATION Requesting Provider Information Place of Service Provider Name Facility Name Provider ID Facility ID PATIENT INFORMATION Patient Name:_____________________________ Patient DOB :_____________ Patient Account Number______________ Patient ID:______________ CLAIM INFORMATION Date(s) of Service_____________ CPT_________ Diagnosis_______ Dermatology Patch Allergy Testing - Information Request Form Page 1 of 3 CLINICAL INFORMATION Did the patient have direct skin testing (for immediate hypersensitivity) by: Percutaneous or epicutaneous (scratch, prick, or puncture)? ________________ Intradermal testing? ___________________________________ Inhalant allergy evaluation? _________________ Did the patient have patch (application) testing (most commonly used: T.R.U.E. -

Blueprint Genetics Craniosynostosis Panel
Craniosynostosis Panel Test code: MA2901 Is a 38 gene panel that includes assessment of non-coding variants. Is ideal for patients with craniosynostosis. About Craniosynostosis Craniosynostosis is defined as the premature fusion of one or more cranial sutures leading to secondary distortion of skull shape. It may result from a primary defect of ossification (primary craniosynostosis) or, more commonly, from a failure of brain growth (secondary craniosynostosis). Premature closure of the sutures (fibrous joints) causes the pressure inside of the head to increase and the skull or facial bones to change from a normal, symmetrical appearance resulting in skull deformities with a variable presentation. Craniosynostosis may occur in an isolated setting or as part of a syndrome with a variety of inheritance patterns and reccurrence risks. Craniosynostosis occurs in 1/2,200 live births. Availability 4 weeks Gene Set Description Genes in the Craniosynostosis Panel and their clinical significance Gene Associated phenotypes Inheritance ClinVar HGMD ALPL Odontohypophosphatasia, Hypophosphatasia perinatal lethal, AD/AR 78 291 infantile, juvenile and adult forms ALX3 Frontonasal dysplasia type 1 AR 8 8 ALX4 Frontonasal dysplasia type 2, Parietal foramina AD/AR 15 24 BMP4 Microphthalmia, syndromic, Orofacial cleft AD 8 39 CDC45 Meier-Gorlin syndrome 7 AR 10 19 EDNRB Hirschsprung disease, ABCD syndrome, Waardenburg syndrome AD/AR 12 66 EFNB1 Craniofrontonasal dysplasia XL 28 116 ERF Craniosynostosis 4 AD 17 16 ESCO2 SC phocomelia syndrome, Roberts syndrome -

MECHANISMS in ENDOCRINOLOGY: Novel Genetic Causes of Short Stature
J M Wit and others Genetics of short stature 174:4 R145–R173 Review MECHANISMS IN ENDOCRINOLOGY Novel genetic causes of short stature 1 1 2 2 Jan M Wit , Wilma Oostdijk , Monique Losekoot , Hermine A van Duyvenvoorde , Correspondence Claudia A L Ruivenkamp2 and Sarina G Kant2 should be addressed to J M Wit Departments of 1Paediatrics and 2Clinical Genetics, Leiden University Medical Center, PO Box 9600, 2300 RC Leiden, Email The Netherlands [email protected] Abstract The fast technological development, particularly single nucleotide polymorphism array, array-comparative genomic hybridization, and whole exome sequencing, has led to the discovery of many novel genetic causes of growth failure. In this review we discuss a selection of these, according to a diagnostic classification centred on the epiphyseal growth plate. We successively discuss disorders in hormone signalling, paracrine factors, matrix molecules, intracellular pathways, and fundamental cellular processes, followed by chromosomal aberrations including copy number variants (CNVs) and imprinting disorders associated with short stature. Many novel causes of GH deficiency (GHD) as part of combined pituitary hormone deficiency have been uncovered. The most frequent genetic causes of isolated GHD are GH1 and GHRHR defects, but several novel causes have recently been found, such as GHSR, RNPC3, and IFT172 mutations. Besides well-defined causes of GH insensitivity (GHR, STAT5B, IGFALS, IGF1 defects), disorders of NFkB signalling, STAT3 and IGF2 have recently been discovered. Heterozygous IGF1R defects are a relatively frequent cause of prenatal and postnatal growth retardation. TRHA mutations cause a syndromic form of short stature with elevated T3/T4 ratio. Disorders of signalling of various paracrine factors (FGFs, BMPs, WNTs, PTHrP/IHH, and CNP/NPR2) or genetic defects affecting cartilage extracellular matrix usually cause disproportionate short stature. -

A Novel De Novo 20Q13.32&Ndash;Q13.33
Journal of Human Genetics (2015) 60, 313–317 & 2015 The Japan Society of Human Genetics All rights reserved 1434-5161/15 www.nature.com/jhg ORIGINAL ARTICLE Anovelde novo 20q13.32–q13.33 deletion in a 2-year-old child with poor growth, feeding difficulties and low bone mass Meena Balasubramanian1, Edward Atack2, Kath Smith2 and Michael James Parker1 Interstitial deletions of the long arm of chromosome 20 are rarely reported in the literature. We report a 2-year-old child with a 2.6 Mb deletion of 20q13.32–q13.33, detected by microarray-based comparative genomic hybridization, who presented with poor growth, feeding difficulties, abnormal subcutaneous fat distribution with the lack of adipose tissue on clinical examination, facial dysmorphism and low bone mass. This report adds to rare publications describing constitutional aberrations of chromosome 20q, and adds further evidence to the fact that deletion of the GNAS complex may not always be associated with an Albright’s hereditary osteodystrophy phenotype as described previously. Journal of Human Genetics (2015) 60, 313–317; doi:10.1038/jhg.2015.22; published online 12 March 2015 INTRODUCTION resuscitation immediately after birth and Apgar scores were 9 and 9 at 1 and Reports of isolated subtelomeric deletions of the long arm of 10 min, respectively, of age. Birth parameters were: weight ~ 1.56 kg (0.4th–2nd chromosome 20 are rare, but a few cases have been reported in the centile), length ~ 40 cm (o0.4th centile) and head circumference ~ 28.2 cm o fi literature over the past 30 years.1–13 Traylor et al.12 provided an ( 0.4th centile). -

Waardenburg's Syndrome and Familial Periodic Paralysis C
Postgraduate Medical Journal (June 1971) 47, 354-360. Postgrad Med J: first published as 10.1136/pgmj.47.548.354 on 1 June 1971. Downloaded from CLINICAL REVIEW Waardenburg's syndrome and familial periodic paralysis C. H. TAY A.M., M.B., B.S., M.R.C.P.(Glas.) Senior Medical Registrar and Clinical Teacher, Medical Unit II, Department of Clinical Medicine, University of Singapore, Outram Road General Hospital, Singapore, 3 Summary McKenzie, 1958; Fisch, 1959; Arnvig, 1958; Nine members in three generations of a Chinese Partington, 1959; Di George, Olmsted & Harley, family were found to have Waardenburg's syndrome 1960; Campbell, Campbell & Swift, 1962; Chew, comprising, mainly, lateral displacement of the inner Chen & Tan, 1968). canthi, broadening of the nasal root and hyper- It is also known as a variant of the first arch trichosis of the eyebrows. Other minor features were syndrome (McKenzie, 1958; Campbell et al., 1962) also found. and later other minor characteristics of the syndrome Two patients had in addition, hypokalemic periodic were added: (1) abnormal depigmentation of the paralysis of the familial type, one had prominent skin (Klein, 1950; Mende, 1926; Partington, 1959; frontal bossing and another, bilateral cleft lips and Campbell et al, 1962), (2) pigmentary changes of the palate. These associated anomalies have not been fundi (Waardenburg, 1951; Di George et al., 1960)Protected by copyright. previously documented and the presence of two auto- and (3) abnormal facial appearance to maldevelop- somal dominant genetic defects in this family is of ment of the maxilla and mandible (Fisch, 1959; particular interest. Campbell et al., 1962).