Role of the Mannose Receptor (CD206) in Innate Immunity to Ricin Toxin
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Chemical Disinfectants for Biohazardous Materials (3/21)
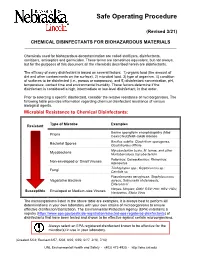
Safe Operating Procedure (Revised 3/21) CHEMICAL DISINFECTANTS FOR BIOHAZARDOUS MATERIALS ____________________________________________________________________________ Chemicals used for biohazardous decontamination are called sterilizers, disinfectants, sanitizers, antiseptics and germicides. These terms are sometimes equivalent, but not always, but for the purposes of this document all the chemicals described herein are disinfectants. The efficacy of every disinfectant is based on several factors: 1) organic load (the amount of dirt and other contaminants on the surface), 2) microbial load, 3) type of organism, 4) condition of surfaces to be disinfected (i.e., porous or nonporous), and 5) disinfectant concentration, pH, temperature, contact time and environmental humidity. These factors determine if the disinfectant is considered a high, intermediate or low-level disinfectant, in that order. Prior to selecting a specific disinfectant, consider the relative resistance of microorganisms. The following table provides information regarding chemical disinfectant resistance of various biological agents. Microbial Resistance to Chemical Disinfectants: Type of Microbe Examples Resistant Bovine spongiform encephalopathy (Mad Prions Cow) Creutzfeldt-Jakob disease Bacillus subtilis; Clostridium sporogenes, Bacterial Spores Clostridioides difficile Mycobacterium bovis, M. terrae, and other Mycobacteria Nontuberculous mycobacterium Poliovirus; Coxsackievirus; Rhinovirus; Non-enveloped or Small Viruses Adenovirus Trichophyton spp.; Cryptococcus sp.; -

Chemical Threat Agents Call Poison Control 24/7 for Treatment Information 1.800.222.1222 Blood Nerve Blister Pulmonary Metals Toxins
CHEMICAL THREAT AGENTS CALL POISON CONTROL 24/7 FOR TREATMENT INFORMATION 1.800.222.1222 BLOOD NERVE BLISTER PULMONARY METALS TOXINS SYMPTOMS SYMPTOMS SYMPTOMS SYMPTOMS SYMPTOMS SYMPTOMS • Vertigo • Diarrhea, diaphoresis • Itching • Upper respiratory tract • Cough • Shock • Tachycardia • Urination • Erythema irritation • Metallic taste • Organ failure • Tachypnea • Miosis • Yellowish blisters • Rhinitis • CNS effects • Cyanosis • Bradycardia, bronchospasm • Flu-like symptoms • Coughing • Shortness of breath • Flu-like symptoms • Emesis • Delayed eye irritation • Choking • Flu-like symptoms • Nonspecific neurological • Lacrimation • Delayed pulmonary edema • Visual disturbances symptoms • Salivation, sweating INDICATIVE LAB TESTS INDICATIVE LAB TESTS INDICATIVE LAB TEST INDICATIVE LAB TESTS INDICATIVE LAB TESTS INDICATIVE LAB TESTS • Increased anion gap • Decreased cholinesterase • Thiodiglycol present in urine • Decreased pO2 • Proteinuria None Available • Metabolic acidosis • Increased anion gap • Decreased pCO2 • Renal assessment • Narrow pO2 difference • Metabolic acidosis • Arterial blood gas between arterial and venous • Chest radiography samples DEFINITIVE TEST DEFINITIVE TEST DEFINITIVE TEST DEFINITIVE TESTS DEFINITIVE TESTS • Blood cyanide levels • Urine nerve agent • Urine blister agent No definitive tests available • Blood metals panel • Urine ricinine metabolites metabolites • Urine metals panel • Urine abrine POTENTIAL AGENTS POTENTIAL AGENTS POTENTIAL AGENTS POTENTIAL AGENTS POTENTIAL AGENTS POTENTIAL AGENTS • Hydrogen Cyanide -

Human and Mouse CD Marker Handbook Human and Mouse CD Marker Key Markers - Human Key Markers - Mouse
Welcome to More Choice CD Marker Handbook For more information, please visit: Human bdbiosciences.com/eu/go/humancdmarkers Mouse bdbiosciences.com/eu/go/mousecdmarkers Human and Mouse CD Marker Handbook Human and Mouse CD Marker Key Markers - Human Key Markers - Mouse CD3 CD3 CD (cluster of differentiation) molecules are cell surface markers T Cell CD4 CD4 useful for the identification and characterization of leukocytes. The CD CD8 CD8 nomenclature was developed and is maintained through the HLDA (Human Leukocyte Differentiation Antigens) workshop started in 1982. CD45R/B220 CD19 CD19 The goal is to provide standardization of monoclonal antibodies to B Cell CD20 CD22 (B cell activation marker) human antigens across laboratories. To characterize or “workshop” the antibodies, multiple laboratories carry out blind analyses of antibodies. These results independently validate antibody specificity. CD11c CD11c Dendritic Cell CD123 CD123 While the CD nomenclature has been developed for use with human antigens, it is applied to corresponding mouse antigens as well as antigens from other species. However, the mouse and other species NK Cell CD56 CD335 (NKp46) antibodies are not tested by HLDA. Human CD markers were reviewed by the HLDA. New CD markers Stem Cell/ CD34 CD34 were established at the HLDA9 meeting held in Barcelona in 2010. For Precursor hematopoetic stem cell only hematopoetic stem cell only additional information and CD markers please visit www.hcdm.org. Macrophage/ CD14 CD11b/ Mac-1 Monocyte CD33 Ly-71 (F4/80) CD66b Granulocyte CD66b Gr-1/Ly6G Ly6C CD41 CD41 CD61 (Integrin b3) CD61 Platelet CD9 CD62 CD62P (activated platelets) CD235a CD235a Erythrocyte Ter-119 CD146 MECA-32 CD106 CD146 Endothelial Cell CD31 CD62E (activated endothelial cells) Epithelial Cell CD236 CD326 (EPCAM1) For Research Use Only. -

Macrophage Activation Markers, CD163 and CD206, in Acute-On-Chronic Liver Failure
cells Review Macrophage Activation Markers, CD163 and CD206, in Acute-on-Chronic Liver Failure Marlene Christina Nielsen 1 , Rasmus Hvidbjerg Gantzel 2 , Joan Clària 3,4 , Jonel Trebicka 3,5 , Holger Jon Møller 1 and Henning Grønbæk 2,* 1 Department of Clinical Biochemistry, Aarhus University Hospital, 8200 Aarhus N, Denmark; [email protected] (M.C.N.); [email protected] (H.J.M.) 2 Department of Hepatology & Gastroenterology, Aarhus University Hospital, 8200 Aarhus N, Denmark; [email protected] 3 European Foundation for the Study of Chronic Liver Failure (EF-CLIF), 08021 Barcelona, Spain; [email protected] (J.C.); [email protected] (J.T.) 4 Department of Biochemistry and Molecular Genetics, Hospital Clínic-IDIBAPS, 08036 Barcelona, Spain 5 Translational Hepatology, Department of Internal Medicine I, Goethe University Frankfurt, 60323 Frankfurt, Germany * Correspondence: [email protected]; Tel.: +45-21-67-92-81 Received: 1 April 2020; Accepted: 4 May 2020; Published: 9 May 2020 Abstract: Macrophages facilitate essential homeostatic functions e.g., endocytosis, phagocytosis, and signaling during inflammation, and express a variety of scavenger receptors including CD163 and CD206, which are upregulated in response to inflammation. In healthy individuals, soluble forms of CD163 and CD206 are constitutively shed from macrophages, however, during inflammation pathogen- and damage-associated stimuli induce this shedding. Activation of resident liver macrophages viz. Kupffer cells is part of the inflammatory cascade occurring in acute and chronic liver diseases. We here review the existing literature on sCD163 and sCD206 function and shedding, and potential as biomarkers in acute and chronic liver diseases with a particular focus on Acute-on-Chronic Liver Failure (ACLF). -

In Sickness and in Health: the Immunological Roles of the Lymphatic System
International Journal of Molecular Sciences Review In Sickness and in Health: The Immunological Roles of the Lymphatic System Louise A. Johnson MRC Human Immunology Unit, MRC Weatherall Institute of Molecular Medicine, University of Oxford, John Radcliffe Hospital, Headington, Oxford OX3 9DS, UK; [email protected] Abstract: The lymphatic system plays crucial roles in immunity far beyond those of simply providing conduits for leukocytes and antigens in lymph fluid. Endothelial cells within this vasculature are dis- tinct and highly specialized to perform roles based upon their location. Afferent lymphatic capillaries have unique intercellular junctions for efficient uptake of fluid and macromolecules, while expressing chemotactic and adhesion molecules that permit selective trafficking of specific immune cell subsets. Moreover, in response to events within peripheral tissue such as inflammation or infection, soluble factors from lymphatic endothelial cells exert “remote control” to modulate leukocyte migration across high endothelial venules from the blood to lymph nodes draining the tissue. These immune hubs are highly organized and perfectly arrayed to survey antigens from peripheral tissue while optimizing encounters between antigen-presenting cells and cognate lymphocytes. Furthermore, subsets of lymphatic endothelial cells exhibit differences in gene expression relating to specific func- tions and locality within the lymph node, facilitating both innate and acquired immune responses through antigen presentation, lymph node remodeling and regulation of leukocyte entry and exit. This review details the immune cell subsets in afferent and efferent lymph, and explores the mech- anisms by which endothelial cells of the lymphatic system regulate such trafficking, for immune surveillance and tolerance during steady-state conditions, and in response to infection, acute and Citation: Johnson, L.A. -

2018 Annual Survey of Biological and Chemical Agents Regulated by Homeland Security (And Carcinogens Regulated by OSHA)
Name: Dept: Date: 2018 Annual Survey of Biological and Chemical Agents regulated by Homeland Security (and carcinogens regulated by OSHA) Due (date) All labs that do not have a current chemical inventory in Chematix MUST complete this survey. The University is required to make an annual report of all chemicals on the Chemical Facility Anti-Terrorism Standards (CFATS) lists. Additional information regarding the regulations is available on the EH&S website at http://www.safety.rochester.edu/restricted/occsafe/chemicalagent.html and https://www.selectagents.gov. 1. Please review the lists on the following pages and indicate if any are possessed by your lab. The CAS# has been added to the list for ease of searching databases. The CAS# is a Chemical Abstract Service numbering system which assigns a unique number to every chemical substance based on structure; this helps avoid confusion by use of synonyms or different naming conventions. a. If yes for possession, place an X in the applicable box and if requested, include the quantity held in your lab. b. If no, leave blank. 2. After reviewing the list, please complete the information box below (or on last page for possession), then sign, date and return to EH&S. 3. Please call Donna Douglass at 275-2402 if you have any questions. Thank you for your cooperation in collecting data required by the Department of Homeland Security! Possession: 1) Fill in applicable boxes, 2) have PI sign last page, 3) return all pages to Donna Douglass OR Non-possession: 1) Check only one box on the left, 2) sign, 3) return just this page to Donna Douglass I do not have a lab, do not work in a lab, nor do I possess any of the agents in this survey. -

Insights Into Interactions of Mycobacteria with the Host Innate
This is an open access article published under a Creative Commons Attribution (CC-BY) License, which permits unrestricted use, distribution and reproduction in any medium, provided the author and source are cited. Articles pubs.acs.org/acschemicalbiology Insights into Interactions of Mycobacteria with the Host Innate Immune System from a Novel Array of Synthetic Mycobacterial Glycans † ‡ † † † † Ruixiang Blake Zheng, Sabine A. F. Jegouzo,́ Maju Joe, Yu Bai, Huu-Anh Tran, Ke Shen, † † † † § § Jörn Saupe, Li Xia, Md. Faiaz Ahmed, Yu-Hsuan Liu, Pratap Subhashrao Patil, Ashish Tripathi, § ‡ † ‡ Shang-Cheng Hung, Maureen E. Taylor,*, Todd L. Lowary,*, and Kurt Drickamer*, † Department of Chemistry and Alberta Glycomics Centre, University of Alberta, Edmonton, AB T6G 2G2, Canada ‡ Department of Life Sciences, Imperial College, London SW7 2AZ, United Kingdom § Genomics Research Centre, Academia Sinica, Nangang, Taipei 11529, Taiwan *S Supporting Information ABSTRACT: An array of homogeneous glycans representing all the major carbohydrate structures present in the cell wall of the human pathogen Mycobacterium tuberculosis and other mycobacteria has been probed with a panel of glycan-binding receptors expressed on cells of the mammalian innate immune system. The results provide an overview of interactions between mycobacterial glycans and receptors that mediate uptake and survival in macrophages, dendritic cells, and sinusoidal endothelial cells. A subset of the wide variety of glycan structures present on mycobacterial surfaces interact with cells of the innate immune system through the receptors tested. Endocytic receptors, including the mannose receptor, DC-SIGN, langerin, and DC-SIGNR (L-SIGN), interact predominantly with mannose-containing caps found on the mycobacterial polysaccharide lipoarabinomannan. Some of these receptors also interact with phosphatidyl-myo-inositol mannosides and mannose-containing phenolic glycolipids. -

The Role of Langerin Transfer From
Inhibition of Two Temporal Phases of HIV-1 Transfer from Primary Langerhans Cells to T Cells: The Role of Langerin This information is current as Najla Nasr, Joey Lai, Rachel A. Botting, Sarah K. Mercier, of September 29, 2021. Andrew N. Harman, Min Kim, Stuart Turville, Rob J. Center, Teresa Domagala, Paul R. Gorry, Norman Olbourne and Anthony L. Cunningham J Immunol 2014; 193:2554-2564; Prepublished online 28 July 2014; Downloaded from doi: 10.4049/jimmunol.1400630 http://www.jimmunol.org/content/193/5/2554 Supplementary http://www.jimmunol.org/content/suppl/2014/07/26/jimmunol.140063 http://www.jimmunol.org/ Material 0.DCSupplemental References This article cites 60 articles, 30 of which you can access for free at: http://www.jimmunol.org/content/193/5/2554.full#ref-list-1 Why The JI? Submit online. by guest on September 29, 2021 • Rapid Reviews! 30 days* from submission to initial decision • No Triage! Every submission reviewed by practicing scientists • Fast Publication! 4 weeks from acceptance to publication *average Subscription Information about subscribing to The Journal of Immunology is online at: http://jimmunol.org/subscription Permissions Submit copyright permission requests at: http://www.aai.org/About/Publications/JI/copyright.html Email Alerts Receive free email-alerts when new articles cite this article. Sign up at: http://jimmunol.org/alerts The Journal of Immunology is published twice each month by The American Association of Immunologists, Inc., 1451 Rockville Pike, Suite 650, Rockville, MD 20852 Copyright © 2014 by The American Association of Immunologists, Inc. All rights reserved. Print ISSN: 0022-1767 Online ISSN: 1550-6606. -

Human Lectins, Their Carbohydrate Affinities and Where to Find Them
biomolecules Review Human Lectins, Their Carbohydrate Affinities and Where to Review HumanFind Them Lectins, Their Carbohydrate Affinities and Where to FindCláudia ThemD. Raposo 1,*, André B. Canelas 2 and M. Teresa Barros 1 1, 2 1 Cláudia D. Raposo * , Andr1 é LAQVB. Canelas‐Requimte,and Department M. Teresa of Chemistry, Barros NOVA School of Science and Technology, Universidade NOVA de Lisboa, 2829‐516 Caparica, Portugal; [email protected] 12 GlanbiaLAQV-Requimte,‐AgriChemWhey, Department Lisheen of Chemistry, Mine, Killoran, NOVA Moyne, School E41 of ScienceR622 Co. and Tipperary, Technology, Ireland; canelas‐ [email protected] NOVA de Lisboa, 2829-516 Caparica, Portugal; [email protected] 2* Correspondence:Glanbia-AgriChemWhey, [email protected]; Lisheen Mine, Tel.: Killoran, +351‐212948550 Moyne, E41 R622 Tipperary, Ireland; [email protected] * Correspondence: [email protected]; Tel.: +351-212948550 Abstract: Lectins are a class of proteins responsible for several biological roles such as cell‐cell in‐ Abstract:teractions,Lectins signaling are pathways, a class of and proteins several responsible innate immune for several responses biological against roles pathogens. such as Since cell-cell lec‐ interactions,tins are able signalingto bind to pathways, carbohydrates, and several they can innate be a immuneviable target responses for targeted against drug pathogens. delivery Since sys‐ lectinstems. In are fact, able several to bind lectins to carbohydrates, were approved they by canFood be and a viable Drug targetAdministration for targeted for drugthat purpose. delivery systems.Information In fact, about several specific lectins carbohydrate were approved recognition by Food by andlectin Drug receptors Administration was gathered for that herein, purpose. plus Informationthe specific organs about specific where those carbohydrate lectins can recognition be found by within lectin the receptors human was body. -

Exploiting Manipulated Small Extracellular Vesicles to Subvert Immunosuppression at the Tumor Microenvironment Through Mannose Receptor/CD206 Targeting
International Journal of Molecular Sciences Review Exploiting Manipulated Small Extracellular Vesicles to Subvert Immunosuppression at the Tumor Microenvironment through Mannose Receptor/CD206 Targeting Maria Luisa Fiani *, Valeria Barreca, Massimo Sargiacomo, Flavia Ferrantelli, Francesco Manfredi and Maurizio Federico * National Center for Global Health, Istituto Superiore di Sanità, 00161 Rome, Italy; [email protected] (V.B.); [email protected] (M.S.); fl[email protected] (F.F.); [email protected] (F.M.) * Correspondence: maria.fi[email protected] (M.L.F.); [email protected] (M.F.); Tel.: +39-06-4990-2518 (M.L.F.); +39-06-4990-6016 (M.F.) Received: 6 July 2020; Accepted: 27 August 2020; Published: 31 August 2020 Abstract: Immunosuppression at tumor microenvironment (TME) is one of the major obstacles to be overcome for an effective therapeutic intervention against solid tumors. Tumor-associated macrophages (TAMs) comprise a sub-population that plays multiple pro-tumoral roles in tumor development including general immunosuppression, which can be identified in terms of high expression of mannose receptor (MR or CD206). Immunosuppressive TAMs, like other macrophage sub-populations, display functional plasticity that allows them to be re-programmed to inflammatory macrophages. In order to mitigate immunosuppression at the TME, several efforts are ongoing to effectively re-educate pro-tumoral TAMs. Extracellular vesicles (EVs), released by both normal and tumor cells types, are emerging as key mediators of the cell to cell communication and have been shown to have a role in the modulation of immune responses in the TME. Recent studies demonstrated the enrichment of high mannose glycans on the surface of small EVs (sEVs), a subtype of EVs of endosomal origin of 30–150 nm in diameter. -

Abrin Fact Sheet
ABRIN FACT SHEET What is abrin? Abrin is a natural poison that is found in the seeds of a plant called rosary pea. Abrin can be made in the form of a powder, a mist and a pellet, or it can be dissolved in water. Abrin is a stable substance that can last for a long time in the environment regardless of extreme hot or cold temperature conditions. Avoid exposure to abrin because there is no antidote that exists. How can you be exposed to abrin? It will take a deliberate act to obtain abrin from rosary pea seeds and use it to poison people. Breathing in abrin (mist or powder) can expose you. You could be exposed if you touch any surfaces where the particles or droplets have landed or if the droplets have landed on your skin or in your eyes. You could ingest abrin if it is in the food or water. Abrin poisoning is not contagious. It cannot be spread from one person to another through casual contact. What are the immediate symptoms of exposure to abrin? If you inhale abrin, within a few hours you may have the following symptoms: difficulty breathing, fever, cough, nausea, heavy sweating, tightness in the chest and fluid building up in the lungs. If you ingest a large amount of abrin, you will develop vomiting and diarrhea that may become bloody. Next, severe dehydration followed by low blood pressure. Other symptoms may include hallucinations, seizures and blood in the urine. If you have skin and eye exposure, the mist or powder abrin can cause redness and pain of the skin and the eyes. -

SUMMARY of PARTICULARLY HAZARDOUS SUBSTANCES (By
SUMMARY OF PARTICULARLY HAZARDOUS SUBSTANCES (by alpha) Key: SC -- Select Carcinogens RT -- Reproductive Toxins AT -- Acute Toxins SA -- Readily Absorbed Through the Skin DHS -- Chemicals of Interest Revised: 11/2012 ________________________________________________________ ___________ _ _ _ _ _ _ _ _ _ _ _ ||| | | | CHEMICAL NAME CAS # |SC|RT| AT | SA |DHS| ________________________________________________________ ___________ | _ | _ | _ | _ | __ | | | | | | | 2,4,5-T 000093-76-5 | | x | | x | | ABRIN 001393-62-0 | | | x | | | ACETALDEHYDE 000075-07-0 | x | | | | | ACETAMIDE 000060-35-5 | x | | | | | ACETOHYDROXAMIC ACID 000546-88-3 ||x| | x | | ACETONE CYANOHYDRIN, STABILIZED 000075-86-5 | | | x | | x | ACETYLAMINOFLUORENE,2- 000053-96-3 | x | | | | | ACID MIST, STRONG INORGANIC 000000-00-0 | x | | | | | ACROLEIN 000107-02-8 | | x | x | x | | ACRYLAMIDE 000079-06-1 | x | x | | x | | ACRYLONITRILE 000107-13-1 | x | x | x | x | | ACTINOMYCIN D 000050-76-0 ||x| | x | | ADIPONITRILE 000111-69-3 | | | x | | | ADRIAMYCIN 023214-92-8 | x | | | | | AFLATOXIN B1 001162-65-8 | x | | | | | AFLATOXIN M1 006795-23-9 | x | | | | | AFLATOXINS 001402-68-2 | x | | x | | | ALL-TRANS RETINOIC ACID 000302-79-4 | | x | | x | | ALPRAZOMAN 028981-97-7 | | x | | x | | ALUMINUM PHOSPHIDE 020859-73-8 | | | x | | x | AMANTADINE HYDROCHLORIDE 000665-66-7 | | x | | x | | AMINO-2,4-DIBROMOANTHRAQUINONE 000081-49-2 | x | | | | | AMINO-2-METHYLANTHRAQUINONE, 1- 000082-28-0 | x | | | | | AMINO-3,4-DIMETHYL-3h-IMIDAZO(4,5f)QUINOLINE,2- 077094-11-2 | x | | | | | AMINO-3,8-DIMETHYL-3H-IMIDAZO(4,5-f)QUINOXALINE,