Frequent Occurrence of SARS-Cov-2 Transmission Among Non-Close Contacts Exposed to COVID-19 Patients
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

CURRENT APPLIED PHYSICS "Physics, Chemistry and Materials Science"
CURRENT APPLIED PHYSICS "Physics, Chemistry and Materials Science" AUTHOR INFORMATION PACK TABLE OF CONTENTS XXX . • Description p.1 • Audience p.1 • Impact Factor p.1 • Abstracting and Indexing p.2 • Editorial Board p.2 • Guide for Authors p.4 ISSN: 1567-1739 DESCRIPTION . Current Applied Physics (Curr. Appl. Phys.) is a monthly published international interdisciplinary journal covering all applied science in physics, chemistry, and materials science, with their fundamental and engineering aspects. Topics covered in the journal are diverse and reflect the most current applied research, including: • Spintronics and superconductivity • Photonics, optoelectronics, and spectroscopy • Semiconductor device physics • Physics and applications of nanoscale materials • Plasma physics and technology • Advanced materials physics and engineering • Dielectrics, functional oxides, and multiferroics • Organic electronics and photonics • Energy-related materials and devices • Advanced optics and optical engineering • Biophysics and bioengineering, including soft matters and fluids • Emerging, interdisciplinary and others related to applied physics • Regular research papers, letters and review articles with contents meeting the scope of the journal will be considered for publication after peer review. The journal is owned by the Korean Physical Society (http://www.kps.or.kr ) AUDIENCE . Chemists, physicists, materials scientists and engineers with an interest in advanced materials for future applications. IMPACT FACTOR . 2020: 2.480 © Clarivate Analytics -

Curriculum Vitae
CURRICULUM VITAE Min-Hee Ryu, M.D., Ph.D. Professor Department of Oncology Asan Medical Center University of Ulsan College of Medicine Seoul, Korea Address (Work) Department of Oncology Asan Medical Center 88, Olympic-ro, 43-gil, Songpa-gu Seoul 05505 Korea Tel: 82-2-3010-5935, 3010-3210 Fax: 82-2-3010-6961 e-mail: [email protected] Education 1987. 3 – 1989. 2 Pre-Medicine College of Natural Sciences Seoul National University Seoul, Korea 1989. 3 – 1994. 2 M.D. College of Medicine Seoul National University Seoul, Korea 1996. 3 – 1998. 2 Master of Science Postgraduate School Seoul National University Seoul, Korea 2002. 3 – 2006. 2 Ph.D. Postgraduate School University of Ulsan College of Medicine Seoul, Korea Graduate Training 1994. 3 – 1995. 2 Internship Seoul National University Hospital Seoul, Korea 1995. 3 – 1999. 2 Residency, Internal Medicine Seoul National University Hospital Seoul, Korea 2002. 5 – 2004. 2 Fellowship, Hematology/Oncology Asan Medical Center University of Ulsan College of Medicine Seoul, Korea Professional Experience 2004. 3 – 2009. 10 Assistant Professor Department of Oncology Asan Medical Center University of Ulsan College of Medicine Seoul, Korea 2009. 10 – 2015 .09 Associate Professor Department of Oncology Asan Medical Center University of Ulsan College of Medicine Seoul, Korea 2015. 10 – Present Professor Department of Oncology Asan Medical Center University of Ulsan College of Medicine Seoul, Korea 2020. 3 – Present Chief Department of Oncology Asan Medical Center University of UlsanCollege of Medicine Seoul, -

UNIVERSITY of ULSAN(UOU) at a GLANCE What Is UIBP
Do you know SOUTH KOREA ? UNIVERSITY OF ULSAN(UOU) AT A GLANCE APPLY FOR UIBP ? Seoul GDP USD 1.4 trillion (11th in the world) Incheon Establishment Year 1970 ELIGIBILITY REQUIRED DOCUMENTS FOR ADMISSION Daejeon Daegu Kyungju Founder Ju-yung CHUNG (Founder of HYUNDAI Group) GDP per Capita USD 28,000 (28th in the world) Category Details Documents Details Ulsan Gwangju Busan Governance Hyundai Heavy Industries(HHI) Trade USD 1 trillion (8th in the world) Forms downloadable from UOU a) Anyone with foreign citizenship whose parents Application Form Honorary Chancellor Mong-joon CHUNG (Major Shareholder of HHI) global homepage Population 51 million (26th in the world) both also have foreign citizenship, or * http://global.ulsan.ac.kr > Admissions Major Industries Electronic and Electrical, Automotive, Shipbuilding, Chancellor Chung Kil CHUNG (Former Presidential Chief of Staff, Korea) * Applicants(including parents) with dual-citizenship of Statement of Purpose > Overview > Forms & Downloads Korea are not eligible Mechanical, Petrochemical, Steel, Retail, etc. President Yeon Cheon OH (Former President of Seoul National University) Nationality Requirement * Taiwanese applicants are eligible even if one of their Graduation Certificate of MNCs Samsung, LG, Hyundai, SK, POSCO, Lotte, Hanwha, etc. Official Ranking parents holds Korean citizenship Secondary Education, or - 90th in the World (2015 THE 100 under 50 Rankings) b) Anyone with foreign citizenship who completed both Certificate of Equivalent Course - 11th in Korea, 85th in Asia (2015 THE -
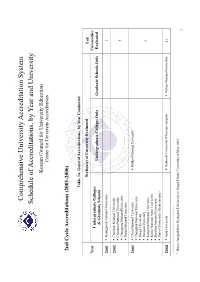
Schedule of Accreditations, by Year and University
Comprehensive University Accreditation System Schedule of Accreditations, by Year and University Korean Council for University Education Center for University Accreditation 2nd Cycle Accreditations (2001-2006) Table 1a: General Accreditations, by Year Conducted Section(s) of University Evaluated # of Year Universities Undergraduate Colleges Undergraduate Colleges Only Graduate Schools Only Evaluated & Graduate Schools 2001 Kyungpook National University 1 2002 Chonbuk National University Chonnam National University 4 Chungnam National University Pusan National University 2003 Cheju National University Mokpo National University Chungbuk National University Daegu University Daejeon University 9 Kangwon National University Korea National Sport University Sunchon National University Yonsei University (Seoul campus) 2004 Ajou University Dankook University (Cheonan campus) Mokpo National University 41 1 Name changed from Kyungsan University to Daegu Haany University in May 2003. 1 Andong National University Hanyang University (Ansan campus) Catholic University of Daegu Yonsei University (Wonju campus) Catholic University of Korea Changwon National University Chosun University Daegu Haany University1 Dankook University (Seoul campus) Dong-A University Dong-eui University Dongseo University Ewha Womans University Gyeongsang National University Hallym University Hanshin University Hansung University Hanyang University Hoseo University Inha University Inje University Jeonju University Konkuk University Korea -

RHEE Joo Yull
RHEE Joo Yull Professor Department of Physics Office 32310B, Science Building 2, Sungkyunkwan University (SKKU) Natural Sciences Campus, 2066 Seobu-ro, Jangan-gu, Suwon, Gyeonggi-do, Republic of Korea Phone 82-31-299-4540 Website E-mail [email protected] Social Media Key Words Electronic Structures, Magnetic materials, Optical Properties, Metamaterials, Research Area Condensed-matter physics, Metamaterials Education 1992 PhD Iowa State University, USA 1980 MSc KAIST, Korea 1978 BSc Seoul National University,Korea Experience Sep. 2005 - Now Professor, Sungkyunkwan University Mar. 1994 - Aug.2005 Professor, Hoseo University Aug.1992 -Feb.1994 Post-doctoralFellow, AmesLab, USA Mar. 1980 - Aug. 1985 Assistant Professor, University of Ulsan, Korea Jan. 2009 – Dec. 2010 Editor-in-Chief, Journal of the Korean Physical Society, and Vice President of the Korean Physical Society, Korea Sep. 2011 – Dec. 2012 Editor-in-Chief and Vice President of the Korean Vacuum Society, Korea Position Sep. 2009 - Now Chairman of Dept. of Phys., SKKU Jan. 2010 - Now Editor, Chines Physics B Sep. 2014 - Now Chair, Publication Committee, NanoKorea2015 and NanoKorea2016 Selected Generalized susceptibility and magnetic ordering in rare-earth nickel boride carbides.Phys. Rev. B Publication 51, 15 585 (1995). Realization of room-temperature ferromagnetism and of improved carrier mobility in Mn-doped ZnO film by oxygen deficiency, introduced by hydrogen and heat treatments,Adv. Mater. 19, 3496– 3500 (2007). Realization of a large magnetic moment in the ferromagnetic CoPt bulk phase,Phys. Rev. Lett. 87, 067208 (2001) One-dimensional magnetic grating structure made easy,Appl. Phys. Lett. 89, 151111 (2006) Active manipulation of plasmonic electromagnetically-induced transparency based on magnetic plasmon resonance, Opt. -

Copyright by Min Jung Son 2004
Copyright by Min Jung Son 2004 The Dissertation Committee for Min Jung Son certifies that this is the approved version of the following dissertation: The Politics of the Traditional Korean Popular Song Style T’ŭrot’ŭ Committee: Stephen Slawek, Supervisor Gerard Béhague Martha Menchaca Avron Boretz Elizabeth Crist The Politics of the Traditional Korean Popular Song Style T’ŭrot’ŭ by Min Jung Son, B.M., M.M., M.M. Dissertation Presented to the Faculty of the Graduate School of the University of Texas at Austin in Partial Fulfillment of the Requirements for the Degree of Doctoral of Philosophy The University of Texas at Austin May, 2004 Dedication To my husband Yn Bok Lee with gratitude and love Acknowledgements This dissertation would not have been possible without the extraordinary guidance of my dissertation committee. My deepest gratitude and sincere admiration must go to professor Stephen Slawek whose scholarship, insight, and advice have enhanced this project. I am indebted to professor Gerard Béhague for his invaluable advice and theoretical suggestions of the project. Special thanks are also due to professors Martha Menchaca, for her gracious, wise, and patient counsel; Avron Boretz, for his enthusiasm, expertise, and willingness to share his knowledge of East Asian popular culture; Elizabeth Crist, for her attention to detail and musicological abilities that continue to inspire my respect. I acknowledge the assistance and support of many informants of my fieldwork in 2002-2003: t’ŭrot’ŭ singers Kim Sŏn-Jung, Lawrence Cho, Han Song-Hŭi, Lee Su-Jin, Chŏng Hye-Ryŏn, T’ae Min, Ko Yŏng-Jun, and Sul Woon- Do; songwriters Park Nam-Ch’un, O Min-U, and Pan Wa-Yŏl; sound engineer Coi Dong-Kwon; producers Park Kŏ-Yŏl and Chŏng Chin-Yŏng; fans Kim Kwang-Jin and Kwon Yong-Ae. -

NKU Academic Exchange in Ulsan, South Korea
NKU Academic Exchange in Ulsan, South Korea https://www.cia.gov Spend a semester or academic year studying at The University of Ulsan A brief introduction… Office of Education Abroad (859) 572-6908 NKU Academic Exchanges The Office of Education Abroad offers academic exchanges as a study abroad option for independent and mature NKU students interested in a semester or year-long immersion experience in another country. The information in this packet is meant to provide an overview of the experience available through an academic exchange in Ulsan, South Korea. However, please keep in mind that this information, especially those regarding visa requirements, is subject to change. It is the responsibility of each NKU student participating in an exchange to take the initiative in the pre-departure process with regards to visa application, application to the Exchange University, air travel arrangements, housing arrangements, and pre-approval of courses. Before and after departure for an academic exchange, the Office of Education Abroad will remain a resource and guide for participating exchange students. South Korea South Korea is a country swathed in green and the Koreans are a people passionate about nature. Spread over the national parks, peaks and valleys, and hot springs are numerous cultural relics and temples that serve to remind visitors of Korea’s long history. Still, the country’s dedication to keeping up with contemporary times is evident in cutting- edge technologies and the worldwide success of companies such as Samsung, LG and Hyundai. Korea has two distinct seasons, with a wet, hot, monsoon summer and a very cold winter. -

Optic Aphasia: a Case Study
Journal of Clinical Neurology / Volume 2 / December, 2006 Case Report Optic Aphasia: A Case Study Miseon Kwon, Ph.D., Jae-Hong Lee, M.D. Department of Neurology, University of Ulsan College of Medicine, Asan Medical Center Optic aphasia is a rare syndrome in which patients are unable to name visually presented objects but have no difficulty in naming those objects on tactile or verbal presentation. We report a 79-year-old man who exhibited anomic aphasia after a left posterior cerebral artery territory infarction. His naming ability was intact on tactile and verbal semantic presentation. The results of the systematic assessment of visual processing of objects and letters indicated that he had optic aphasia with mixed features of visual associative agnosia. Interestingly, although he had difficulty reading Hanja (an ideogram), he could point to Hanja letters on verbal description of their meaning, suggesting that the processes of recognizing objects and Hanja share a common mechanism. J Clin Neurol 2(4):258-261, 2006 Key Words : Optic aphasia, Visual agnosia, Dyslexia INTRODUCTION CASE REPORT The disturbance of naming objects is a common K.D., a 79-year-old, hypertensive, right-handed man symptom in patients with brain damage. However, who had received 11 years of education, visited our naming deficits can be modality specific. Optic aphasia hospital for further management of the stroke that had is the inability to name objects only when they are experienced occurred 9 years previously. We could not presented in a visual mode - the patient can name obtain the medical records from the previous hospital, the objects on tactile or verbal presentation. -
On Korea Began in December 2006 with the Initiation of KEI’S Academic Paper AC Series, a Year-Long Program That Provides an Opportunity for Both Leading
2013 On Korea began in December 2006 with the initiation of KEI’s Academic Paper AC Series, a year-long program that provides an opportunity for both leading Korea scholars and new voices from around the world to speak and write on ADEMIC P current events and trends on the Korean Peninsula. Each year, KEI commissions approximately ten papers and distributes them individually to over 5,000 government officials, think tank experts, and scholars around the United States and the world. Authors are invited to the Korea Economic Institute of America to discuss their research before a Washington, DC policy audience. At the conclusion of each series, the papers are compiled APER SERIES and published together as the On Korea volume. To learn more about how to contribute to future Academic Papers Series forums and other programs at KEI, please visit: www.keia.org. ON KOREA ON K OREA Vo lu me Volume 6: 6 North Korea After Kim Jong-il Korean Trends in an Asia-Pacific Century 1800 K St. NW, Suite 1010 Washington, DC 20006 Korean Politics and Security t. 202.464.1982 f. 202.464.1987 www.keia.org ON KOREA 2013: ACADEMIC PAPER SERIES Volume 6 KEI Editorial Board KEI Editors: Abraham Kim, Nicholas Hamisevicz Contract Editor: Gimga Group Design: Gimga Group. Cover photo courtesy of NASA. The Korea Economic Institute of America is registered under the Foreign Agents Regis- tration Act as an agent of the Korea Institute for International Economic Policy, a public corporation established by the Government of the Repubic of Korea. This material is filed with the Department of Justice, where the required registration statement is available for public inspection. -

Korea-Organization.Pdf
Korea Node Profile Organization NAME INSTITUTION E‐MAIL EXPERTISE / POSITION Youngbae Suh Seoul National University, Seoul [email protected] Land plant taxonomy Gi‐Sik Min Inha University, Incheon [email protected] Molecular taxonomy of invertebrates Jung‐Ki park Chungbuk National University, [email protected] Molecular taxonomy of mollusc Cheongju Jongwoo Jung Ewha Womans University, Seoul [email protected] Population genetics of invertebrates Hang Lee Seoul National University, Seoul [email protected] Conservation biology of vertebrates Mi‐Sook Min Seoul National University, Seoul [email protected] Molecular taxonomy of amphibians Jin Koo Kim Pukyong National University, [email protected] Fish taxonomy Busan Ho‐Yeon Han Yonsei University, Wonju [email protected] Entomology Soowon Cho Chungbuk National University, [email protected] Entomology Cheongju Seunghwan Lee Seoul National University, Seoul [email protected] Entomology Jun‐Im Song Ewha Womans University, Seoul [email protected] Taxonomy of corals Sook Shin Sahmyook University, Seoul [email protected] Taxonomy of echinoderms Kyung Jin Lee National Institute of Biological [email protected] Taxonomy of sponges Resources, Incheon Sung Min Boo Chungnam National University, [email protected] Taxonomy of marine Daejeon macroalgae Jang ‐Seo Ki Sangmyung University, Seoul [email protected] Molecular taxonomy of microalgae Man Kyoon University of Ulsan, Ulsan [email protected] Taxonomy of protozoans Shin Yunho Lee Korea Ocean Research & [email protected] Molecular taxonomy and Development Institute, Ansan technology development Jong Bhak Personal Genomics Institute, [email protected] Database and data analysis Suwon Ui Wook Hwang Kyungpook National University, [email protected] Molecular phylogeny of Daegu arthropods Seung Yong GenoCheck Co., Ansan [email protected] Technology development Hwang . -
Congress Program
Congress Program BMJD 6TH WORLD CONGRESS on Controversies, Debates & Consensus in Bone, Muscle & Joint Diseases Bangkok, Thailand Endorsed by November 8-10, 2018 bmjd-congress.org Timetable Thursday, November 8, 2018 Hall A 15:15-15:45 Opening Session 15:45-16:10 Break Asia Pacific League of Associations for Rheumatology (APLAR) Symposium: 16:10-17:00 Recent progress on genetic and cellular rheumatology in APLAR 17:00-17:10 Break Industry Symposium: 17:10-18:00 Understanding patient needs in the treatment of symptomatic osteoarthritis Supported by Mylan 18:00 Networking Reception Friday, November 9, 2018 Hall A Session: 08:00-08:50 JAK inhibitors should be first line before biologic agents Supported by Pfizer 08:50-08:55 Break Industry Symposium: 08:55-09:45 Management strategies for rheumatoid arthritis in 2018 Supported by Eli Lilly 09:45-10:00 Break Session: 10:00-10:50 How to deal with vaccination of patients with inflammatory arthritis 10:50-10:55 Break Meet the Experts: 10:55-11:45 Inflammation in osteoarthritis as a therapeutic target 11:45-11:55 Break Industry Lunch Symposium: 11:55-12:45 New perspectives with Diacerein Supported by TRB 12:45-12:55 Break Meet the Experts: 12:55-13:45 How to best manage osteoporosis in patients with arthritis 13:45-14:00 Break Session: Osteoarthritis, a disease of the bone/subchondral bone? 14:00-14:50 Implication for treatment Supported by Samumed 14:50-14:55 Break Session: 14:55-15:45 Biosimilars: Are rheumatologists and patients ready for transitioning patients from an originator to a biosimilar? -

Books KOREAN FOLK TALES for CHILDREN SERIES
Books on KOREA Winter 2018-19 kodansha europe www.kodansha.eu Kodansha Europe is a wholly-owned subsidiary of Kodansha Ltd. of Tokyo, Japan. In addition to the English-language titles published within the group, we also represent a number of other publishers from other parts of Asia, as well as Africa. In this catalogue you will find all our English language books on all aspects of Korea currently available from Hollym Corp., as well as the variety of publishers exported under the umbrella of Kong & Park. These include selected titles from Jimoondang, Longtail Books, Yonsei University Press, The Academy of Korean Studies Press, Cum Libro, Bookhouse and, of course, Kong & Park. While this catalogue is semi-annual (Spring and Autumn), it is also updated if required in between. It is currently only available in PDF format. We welcome interest from anyone with books about Korea in English seeking distribution and trade representation in the U.K., continental Europe, Africa, the Middle East and Southeast Asia who feels that their books or products may fit our portfolio. You can reach us via our website, or by email at: [email protected] PRICES CORRECT AT JULY 31ST, 2018 Our books are imported and paid for in foreign currency. Owing to the continuing volatility of GBP in the currency markets, prices may be subject to further change over the course of the next 12 months: up or down. The PDF of this catalogue will be updated accordingly. FOREIGN RIGHTS Rights enquiries for all our Korean books should be directed to the original publisher.