Dod COVID-19 PMG V3
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
The Web That Has No Weaver
THE WEB THAT HAS NO WEAVER Understanding Chinese Medicine “The Web That Has No Weaver opens the great door of understanding to the profoundness of Chinese medicine.” —People’s Daily, Beijing, China “The Web That Has No Weaver with its manifold merits … is a successful introduction to Chinese medicine. We recommend it to our colleagues in China.” —Chinese Journal of Integrated Traditional and Chinese Medicine, Beijing, China “Ted Kaptchuk’s book [has] something for practically everyone . Kaptchuk, himself an extraordinary combination of elements, is a thinker whose writing is more accessible than that of Joseph Needham or Manfred Porkert with no less scholarship. There is more here to think about, chew over, ponder or reflect upon than you are liable to find elsewhere. This may sound like a rave review: it is.” —Journal of Traditional Acupuncture “The Web That Has No Weaver is an encyclopedia of how to tell from the Eastern perspective ‘what is wrong.’” —Larry Dossey, author of Space, Time, and Medicine “Valuable as a compendium of traditional Chinese medical doctrine.” —Joseph Needham, author of Science and Civilization in China “The only approximation for authenticity is The Barefoot Doctor’s Manual, and this will take readers much further.” —The Kirkus Reviews “Kaptchuk has become a lyricist for the art of healing. And the more he tells us about traditional Chinese medicine, the more clearly we see the link between philosophy, art, and the physician’s craft.” —Houston Chronicle “Ted Kaptchuk’s book was inspirational in the development of my acupuncture practice and gave me a deep understanding of traditional Chinese medicine. -

Roadside Picnic
ROADSIDE PICNIC Arkady and Boris Strugatsky Translated from the Russian by Antonina W. Bouis Cryptomaoist Editions FROM AN INTERVIEW BY A SPECIAL CORRESPONDENT FROM HARMONT RADIO WITH DOCTOR VALENTINE PILMAN, RECIPIENT OF THE NOBEL PRIZE IN PHYSICS FOR 19.. "I suppose that your first serious discovery, Dr. Pilman, should be considered what is now called the Pilman Radiant?" "I don't think so. The Pilman Radiant wasn't the first, nor was it serious, nor was it really a discovery. And it wasn't completely mine, either." "Surely you're joking, doctor. The Pilman Radiant is a concept known to every schoolchild." "That doesn't surprise me. According to some sources, the Pilman Radiant was discovered by a schoolboy. Unfortunately, I don't remember his name. Look it up in Stetson's History of the Visitation -- it's described in full detail there. His version is that the radiant was discovered by a schoolboy, that a college student published the coordinates, but that for some unknown reason it was named after me." "Yes, many amazing things can happen with a discovery. Would you mind explaining it to our listeners, Dr. Pilman?" "The Pilman Radiant is simplicity itself. Imagine that you spin a huge globe and you start firing bullets into it. The bullet holes would lie on the surface in a smooth curve. The whole point of what you call my first serious discovery lies in the simple fact that all six Visitation Zones are situated on the surface of our planet as though someone had taken six shots at Earth from a pistol located some- where along the Earth-Deneb line. -

View of the Colony Itself (Being on the Top Floor of the Security Building Has Its Rewards, If Only That One Reward Was a Nice Sunset Every Now and Again)
The Bright Garden by Alex Puncekar Submitted in Partial Fulfillment of the Requirements for the Degree of Master of Fine Arts in the Northeast Ohio Master of Fine Arts Program YOUNGSTOWN STATE UNIVERSITY May, 2017 The Bright Garden Alex Puncekar I hereby release this thesis to the public. I understand that this thesis will be made available from the OhioLINK ETD Center and the Maag Library Circulation Desk for public access. I also authorize the University or other individuals to make copies of this thesis as needed for scholarly research. Signature: Alex Puncekar, Student Date Approvals: Christopher Barzak, Thesis Advisor Date Imad Rahman, Committee Member Date Eric Wasserman, Committee Member Date Dr. Salvatore A. Sanders, Dean of Graduate Studies Date ABSTRACT Calli Hayford lives on Kipos, a recently colonized planet far from Earth. Amongst the jungles and ravenous animals that threaten the various settlements across the planet’s surface, Calli is dealing with something much more dire: her sick mother, who is slowly dying from an unknown sickness. With funds scarce, Calli decides to do the impossible: to locate auracite, a rare mineral native to Kipos, in the hopes that it will provide her with the money to afford a cure. She leaves home with her friend, the sly and scruffy Sera, and encounters a whole new world outside of her own, one that will force her to answer questions she never knew she needed to answer: how far is she willing to go for someone she loves? iii Table of Contents Prologue 1 Chapter 1 6 Chapter 2 21 Chapter 3 35 Chapter 4 57 Chapter 5 80 Chapter 6 92 Chapter 7 123 Chapter 8 136 Chapter 9 156 Chapter 10 165 Chapter 11 192 Chapter 12 220 Chapter 13 245 Chapter 14 260 Chapter 15 279 Chapter 16 296 Chapter 17 313 Chapter 18 333 Chapter 19 358 Chapter 20 374 Chapter 21 387 iv Chapter 22 397 Epilogue 403 v Prologue Diana Hayford remembers Autumn. -

Volume 17 2016 Hard Work and Sweat
ime kills buildings he alien’s opaque Tas much as it kills Thelmet turned people. The shattered toward me. A single windows and the pinpoint of crimson empty space felt light glowed dully crowded. Even years at its crest. So far later, it smelled of as I could tell, the Volume 17 2016 hard work and sweat. helmet was made Light came in every entirely of a matte crack and hole like black alloy. The water in a sinking armor was similarly ship, and I loved flat and nondescript, the way the light sharpened and played in the room. I angular at the joints preferred to come to the silos during the day; I but relatively light-looking, made of thin layers loved the way the place looked, almost sad and of some metal I’d already seen deflect bullets at broken and empty inside, but beautiful in all its point-blank range. Lights blinked at his elbows mysterious ways. I often thought maybe people and knees. In the smoke and dust-dimmed could be that way, too. light of the half-wrecked hallway, I could make Brandon James Poppert, out a single symbol etched into the breastplate, “Empty Building, Empty Soul” a circle bisected by a stylized shape not unlike the Nike swoosh. I considered reaching for a gun, but I knew that was pointless. I n small intervals across the kitchen table, considered trying a hand-to-hand fight, but Ihe shared the mayhem of that time spent even if that armor didn’t have strength assists, overseas, revealing sounds that echoed through it was still a combat-trained alien in a suit of the night and images of an astonishing orange super dense metal armor against unarmored, glow that burst in the sky so close that he non-combat-trained me. -

Adventure Time, Volume 4 Free
FREE ADVENTURE TIME, VOLUME 4 PDF Ryan North,Braden Lamb,Shelli Paroline,Pendleton Ward | 1 pages | 11 Feb 2014 | Kaboom | 9781608863518 | English | Los Angeles, CA, United States Adventure Time Vol. 4 by Ryan North Goodreads helps you keep track Volume 4 books you want to read. Want to Read saving…. Want Adventure Time Read Currently Reading Read. Other editions. Enlarge cover. Error rating book. Refresh and try again. Open Preview See a Problem? Details if other :. Thanks for telling us about the problem. Return to Book Page. Preview — Adventure Time Vol. Adventure Time Vol. Braden Lamb Illustrations. Shelli Paroline Goodreads Author Illustrations. The highly anticipated fourth volume Volume 4 the all-ages bestseller Adventure Time is here! After a nice battle of ice and saving princess, Finn and Volume 4 discover a series of dungeons just ready for exploring! It's a fun time with pals and Collecting the latest arc of the fan-favorite series with loads of extra materials in this beautiful hardcover edition! Get A Copy. Paperbackpages. More Details Other Editions Friend Reviews. To see what your friends thought of this book, please sign up. To ask other readers questions about Adventure Time Vol. See 1 question about Adventure Time Vol. Lists with This Book. Community Reviews. Showing Average rating 4. Rating details. More filters. Sort order. Start your Volume 4 of Adventure Time Vol. Oh well, I guess it's okay, since the adventure is inside a dungeon he created!!! What time is it? Is sad Ice King backstory time!!! It breaks my heart every time it is mentioned anywhere!!! Not a big fun of the s Polynomial! Not a big fun of the story line there basically is none but the Adventure Time and the characters are rad as usual! Aug 30, Henry rated it really liked it. -

Universidade De São Paulo Escola De Comunicações E Artes
UNIVERSIDADE DE SÃO PAULO ESCOLA DE COMUNICAÇÕES E ARTES ELENA GUERRA ALTHEMAN A Construção do Universo Ficcional e a Serialidade Sutil em Hora de Aventura São Paulo 2019 1 ELENA GUERRA ALTHEMAN A Construção do Universo Ficcional e a Serialidade Sutil em Hora de Aventura Versão Original Dissertação apresentada à Escola de Comunicações e Artes da Universidade de São Paulo para obtenção do título de Mestre em Meios e Processos Audiovisuais. Área de Concentração: História, Teoria e Crítica Orientadora: Profa. Dra. Cecilia Antakly de Mello São Paulo 2019 Autorizo a reprodução e divulgação total ou parcial deste trabalho, por qualquer meio convencional ou eletrônico, para fins de estudo e pesquisa, desde que citada a fonte. Catalogação na Publicação Serviço de Biblioteca e Documentação Escola de Comunicações e Artes da Universidade de São Paulo Dados inseridos pelo(a) autor(a) ________________________________________________________________________________ Altheman, Elena Guerra A Construção do Universo Ficcional e a Serialidade Sutil em Hora de Aventura / Elena Guerra Altheman ; orientadora, Cecília Antakly de Mello. -- São Paulo, 2019. 110 p.: il. Dissertação (Mestrado) - Programa de Pós-Graduação em Meios e Processos Audiovisuais - Escola de Comunicações e Artes / Universidade de São Paulo. Bibliografia Versão original 1. Animação 2. Narrativa Complexa 3. Serialidade Sutil 4. Hora de Aventura 5. Universo Ficcional I. Mello, Cecília Antakly de II. Título. CDD 21.ed. - 791.43 ________________________________________________________________________________ Elaborado por Sarah Lorenzon Ferreira - CRB-8/6888 2 Nome: ALTHEMAN, Elena Guerra Título: A Construção do Universo Ficcional e a Serialidade Sutil em Hora de Aventura Dissertação apresentada à Escola de Comunicações e Artes da Universidade de São Paulo para obtenção do título de Mestre em Meios e Processos Audiovisuais. -

University of Huddersfield Repository
University of Huddersfield Repository Crump, Simon and Stewart, Michael I You He She It - Experiments in Viewpoint Original Citation Crump, Simon and Stewart, Michael (2017) I You He She It - Experiments in Viewpoint. Grist Anthology, 2017 . University of Huddersfield Press. ISBN 978-1-86218-142-7 This version is available at http://eprints.hud.ac.uk/31523/ The University Repository is a digital collection of the research output of the University, available on Open Access. Copyright and Moral Rights for the items on this site are retained by the individual author and/or other copyright owners. Users may access full items free of charge; copies of full text items generally can be reproduced, displayed or performed and given to third parties in any format or medium for personal research or study, educational or not-for-profit purposes without prior permission or charge, provided: • The authors, title and full bibliographic details is credited in any copy; • A hyperlink and/or URL is included for the original metadata page; and • The content is not changed in any way. For more information, including our policy and submission procedure, please contact the Repository Team at: [email protected]. http://eprints.hud.ac.uk/ I YOU HE SHE IT Published by University of Huddersfield Press University of Huddersfield Press The University of Huddersfield Queensgate Huddersfield HD1 3DH Email enquiries [email protected] First published 2017 Text © 2017 all named authors and Editor Simon Crump. This work is licensed under a Creative Commons Attribution 4.0 International License Images © as attributed Every effort has been made to locate copyright holders of materials included and to obtain permission for their publication. -

Bradshaw Stanley Abstract. in This Thesis I View Th
Stanley 1 MA VCS Thesis Proposal Title: But We, To Whom The World Is Author: Bradshaw Stanley Abstract. In this thesis I view the animated children’s show Adventure Time as a 21st century “surrogate,” in the sense developed by performance theorist Joseph Roach, for Mark Twain’s Adventures of Huckleberry Finn. By viewing “surrogation,” reconstruction, and even re-enactment as occurring between two artworks rather than two artists, I outline a theory of desubstantialized “body-to-body transmission” that does not rely on “real” or substantial bodies for its support. I conclude by arguing that embodiment can be understood as a formal problem rather than one defined by organic function or phenomenological sensoria. Research Areas. Embodiment, Affect Theory, Formalism, Animation Theory, Performance Studies, American Studies, Childhood Studies, Queer Theory, Film Studies, New Media, Visual Studies, Critical Theory Agenda. Popularly acclaimed as “the trippiest show on television” (Rolling Stone), “groundbreaking…[and] ever more experimental” (AV Club), “sneakily sophisticated” (New York Times), and “dark, gripping and almost nightmarish” (Indiewire), Adventure Time may sound more like an HBO series than a Cartoon Network animated children’s program. Because such accolades are typically reserved for adult (not to mention live- action, "underground" or foreign) productions, it is unsurprising that Adventure Time has been used to satirize conservative cultural anxieties, as in a ChristWire article that, perhaps picking up on the show’s “trippiness” and eagerness to experiment, asks whether it is “a gateway drug to LSD, homosexuality, and the rave lifestyle.” Such satire indicates a bleed between the formal qualities of a work and the embodied responses its viewers, in this case young children, may have: being exposed to trippy and experimental work, the thinking goes, may incline one to seek out trips and experimentation in other contexts. -

Welcome to Impact Listening 2! the Impact Listening Series Is Designed to Help Your Students Become Better Listeners and More Profi- Cient at English
To the Teacher Welcome to Impact Listening 2! The Impact Listening series is designed to help your students become better listeners and more profi- cient at English. Impact Listening is intended to make teaching listening strategies stimulating and engaging, and to make learning fun and effective. The Impact Listening series is based on four main principles: 1. Rich Input Learners need rich input in order to develop their language ability. The most useful input is contex- tualized, authentic, and interesting for the learners. Input that is slightly above the learners’ profi- ciency level provides a challenge to motivate them. Impact Listening features extracts drawn from or based on authentic conversations, in common social, academic, and business contexts. The audio recordings for the series employ a wide variety of speakers to provide an abundance of interesting speech. 2. Clear Tasks In order to develop their attention span, learners need guidance in what to listen for. Clear tasks guide the student in what to focus on and on what to remember. Task cycles allow students to listen to the same extract more than once, in order to practice controlling their attention and expanding their ability to process more complex speech. Each section in Impact Listening provides a transpar- ent, structured task that is easy to use in the classroom. 3. Listening Strategies In order to become more confident and relaxed, learners need to learn how to listen. By using suc- cessful listening strategies, learners will become more fluent and confident. By teaching listening strategies, teachers encourage their students to learn more efficiently. -
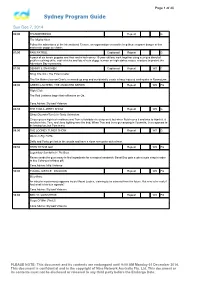
Sydney Program Guide
Page 1 of 40 Sydney Program Guide Sun Dec 7, 2014 06:00 THUNDERBIRDS Repeat G The Mighty Atom Follow the adventures of the International Rescue, an organisation created to help those in grave danger in this marionette puppetry classic. 07:00 PAW PATROL Captioned Repeat G A pack of six heroic puppies and their and a tech-savvy 10-year-old boy work together using a unique blend of problem-solving skills, cool vehicles and lots of cute doggy humour on high-stakes rescue missions to protect the Adventure Bay community. 07:30 DENNIS & GNASHER Captioned Repeat WS C Bring The Din / The Exterminator The Din Makers borrow Gran’s menaced-up amp and accidentally create a bass induced earthquake in Beanotown. 08:00 GREEN LANTERN: THE ANIMATED SERIES Repeat WS PG Flight Club The Red Lanterns begin their offensive on Oa. Cons.Advice: Stylised Violence 08:30 THE TOM & JERRY SHOW Repeat WS G Sleep Disorder/Tom's In-Tents Adventure Ginger gets a high tech mattress and Tom is forbidden to sleep on it, but when Butch sees it and tries to hijack it, it results in him, Tom, and Jerry fighting over the bed. When Tom and Jerry go camping in Yosemite, Jerry appears to be having fun, but Tom is not. 09:00 THE LOONEY TUNES SHOW Repeat WS G We're In Big Truffle Daffy and Porky get lost in the woods and have a close encounter with a bear. 09:30 TEEN TITANS GO! Repeat WS PG Legendary Sandwhich / Pie Bros Raven sends the guys away to find ingredients for a magical sandwich. -
Scout Resource Guide 2016
Scout Resource Guide 2016 DISTRIBUTED BY: GOOSE CREEK DISTRICT NATIONAL CAPITAL AREA COUNCIL BOY SCOUTS OF AMERICA January 2016 Scout Resource Guide 2016 Page 1 The resources listed in this document are articles from previous Goose Creek District monthly newsletters (2011-2015). They include BSA policy guidance, methods, places of interest, websites, books, and much more. All of the links have been rechecked to ensure that they are still active. The articles have been organized into the following categories: PROGRAM DEVELOPMENT ........................................................................ 3 SAFE SCOUTING AND YOUTH PROTECTION .................................................. 3 UNIT/DISTRICT/NATIONAL ORGANIZATION .................................................. 10 FINANCE .................................................................................................. 12 CUB SCOUT ............................................................................................. 14 BOY SCOUT ............................................................................................. 21 RECRUITMENT ......................................................................................... 33 UNIFORMS ............................................................................................... 39 SERVICE .................................................................................................. 46 TRAINING ................................................................................................. 49 SPECIAL NEEDS ...................................................................................... -

Didactica Leopoldo Lugones Pdf
Didactica leopoldo lugones pdf Continue This item is out of stock. If you use the Add to the list you want to add this problem to the list you want, we'll email you when it becomes available. 1st print. Lloyd Cordill. Adventure Time Card Wars is a game of skill, action, strategy and a lot of unusual humor. This is a huge success among fans of the show, as well as fans of games. Now, players can master this exciting game with information and game tips in this official guidebook! This guidebook, with an accompanying poster, will help players of all levels develop their game plan, build amazing decks, and outsmart their opponents. Without skimping on humor, this guide breaks down the strengths and weaknesses of each deck of cards, and includes tips on how to combine cards for the ultimate strategic advantage. Soft cover, 6th x 9th, 176 pages, full color. The cover price is $12.99. Viewing the contents of the shared data community is available according to CC-BY-SA, unless otherwise stated. Arc System Works returns with another metal entry to the Guilty Gear franchise. Here's what you need to know about Guilty Gear -Strive-. 15. Siiskkuta Kello 15.30 Maps of War Official Guide (Adventure Time) View source Share Reddit: Card Wars Kingdom Subreddit Reddit. The latest Community Action content is available under CC-BY-SA unless otherwise stated. See Source Share Pilot: 2007 Season 1: 2010 No. total number in the season Title card Name viewers (in millions) Prod. Airdate 1 1 Slumber Party Panic 2.50 692-009 April 5, 2010 Finn and Princess Bubblegum must protect Candy Kingdom from a horde of zombie candy zombies they accidentally created.