The WHO Application of ICD-10 to Deaths During the Perinatal Period: ICD-PM WHO Library Cataloguing-In-Publication Data
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

N35.12 Postinfective Urethral Stricture, NEC, Female N35.811 Other
N35.12 Postinfective urethral stricture, NEC, female N35.811 Other urethral stricture, male, meatal N35.812 Other urethral bulbous stricture, male N35.813 Other membranous urethral stricture, male N35.814 Other anterior urethral stricture, male, anterior N35.816 Other urethral stricture, male, overlapping sites N35.819 Other urethral stricture, male, unspecified site N35.82 Other urethral stricture, female N35.911 Unspecified urethral stricture, male, meatal N35.912 Unspecified bulbous urethral stricture, male N35.913 Unspecified membranous urethral stricture, male N35.914 Unspecified anterior urethral stricture, male N35.916 Unspecified urethral stricture, male, overlapping sites N35.919 Unspecified urethral stricture, male, unspecified site N35.92 Unspecified urethral stricture, female N36.0 Urethral fistula N36.1 Urethral diverticulum N36.2 Urethral caruncle N36.41 Hypermobility of urethra N36.42 Intrinsic sphincter deficiency (ISD) N36.43 Combined hypermobility of urethra and intrns sphincter defic N36.44 Muscular disorders of urethra N36.5 Urethral false passage N36.8 Other specified disorders of urethra N36.9 Urethral disorder, unspecified N37 Urethral disorders in diseases classified elsewhere N39.0 Urinary tract infection, site not specified N39.3 Stress incontinence (female) (male) N39.41 Urge incontinence N39.42 Incontinence without sensory awareness N39.43 Post-void dribbling N39.44 Nocturnal enuresis N39.45 Continuous leakage N39.46 Mixed incontinence N39.490 Overflow incontinence N39.491 Coital incontinence N39.492 Postural -

Subset of Alphabetical Index to Diseases and Nature of Injury for Use with Perinatal Conditions (P00-P96)
Subset of alphabetical index to diseases and nature of injury for use with perinatal conditions (P00-P96) SUBSET OF ALPHABETICAL INDEX TO DISEASES AND NATURE OF INJURY FOR USE WITH PERINATAL CONDITIONS (P00-P96) Conditions arising in the perinatal period Conditions arising—continued - abnormal, abnormality—continued Note - Conditions arising in the perinatal - - fetus, fetal period, even though death or morbidity - - - causing disproportion occurs later, should, as far as possible, be - - - - affecting fetus or newborn P03.1 coded to chapter XVI, which takes - - forces of labor precedence over chapters containing codes - - - affecting fetus or newborn P03.6 for diseases by their anatomical site. - - labor NEC - - - affecting fetus or newborn P03.6 These exclude: - - membranes (fetal) Congenital malformations, deformations - - - affecting fetus or newborn P02.9 and chromosomal abnormalities - - - specified type NEC, affecting fetus or (Q00-Q99) newborn P02.8 Endocrine, nutritional and metabolic - - organs or tissues of maternal pelvis diseases (E00-E99) - - - in pregnancy or childbirth Injury, poisoning and certain other - - - - affecting fetus or newborn P03.8 consequences of external causes (S00-T99) - - - - causing obstructed labor Neoplasms (C00-D48) - - - - - affecting fetus or newborn P03.1 Tetanus neonatorum (A33) - - parturition - - - affecting fetus or newborn P03.9 - ablatio, ablation - - presentation (fetus) (see also Presentation, - - placentae (see also Abruptio placentae) fetal, abnormal) - - - affecting fetus or newborn -

Mortality Perinatal Subset, 2013
ICD-10 Mortality Perinatal Subset (2013) Subset of alphabetical index to diseases and nature of injury for use with perinatal conditions (P00-P96) Conditions arising in the perinatal period Note - Conditions arising in the perinatal period, even though death or morbidity occurs later, should, as far as possible, be coded to chapter XVI, which takes precedence over chapters containing codes for diseases by their anatomical site. These exclude: Congenital malformations, deformations and chromosomal abnormalities (Q00-Q99) Endocrine, nutritional and metabolic diseases (E00-E99) Injury, poisoning and certain other consequences of external causes (S00-T99) Neoplasms (C00-D48) Tetanus neonatorum (A33 2a) A -ablatio, ablation - - placentae (see alsoAbruptio placentae) - - - affecting fetus or newborn P02.1 2a -abnormal, abnormality, abnormalities - see also Anomaly - - alphafetoprotein - - - maternal, affecting fetus or newborn P00.8 - - amnion, amniotic fluid - - - affecting fetus or newborn P02.9 - - anticoagulation - - - newborn (transient) P61.6 - - cervix NEC, maternal (acquired) (congenital), in pregnancy or childbirth - - - causing obstructed labor - - - - affecting fetus or newborn P03.1 - - chorion - - - affecting fetus or newborn P02.9 - - coagulation - - - newborn, transient P61.6 - - fetus, fetal 1 ICD-10 Mortality Perinatal Subset (2013) - - - causing disproportion - - - - affecting fetus or newborn P03.1 - - forces of labor - - - affecting fetus or newborn P03.6 - - labor NEC - - - affecting fetus or newborn P03.6 - - membranes -
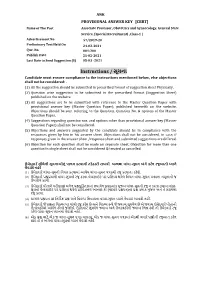
Instructions / સૂચના Candidate Must Ensure Compliance to the Instructions Mentioned Below, Else Objections Shall Not Be Considered:
ANK PROVISIONAL ANSWER KEY [CBRT] Name of The Post Associate Professor, Obstetrics and Gynaecology, General State Service, (Special Recruitment) ,Class-1 | Advertisement No 57/2019-20 Preliminary Test Held On 24-02-2021 Que. No. 001-200 Publish Date 25-02-2021 Last Date to Send Suggestion (S) 05-03 -2021 Instructions / સૂચના Candidate must ensure compliance to the instructions mentioned below, else objections shall not be considered: - (1) All the suggestion should be submitted in prescribed format of suggestion sheet Physically. (2) Question wise suggestion to be submitted in the prescribed formatr (Suggestion rSheet) published on the website.r r (3) All suggestions are to be submitted with reference to the Maste Question Pape withr provisional answe key (Maste Question Paper), published herewith on the website. Objections should be sent referring to the Question, rQuestion No. & options ofr the Maste Question Paper. (4) Suggestions regarding question nos. and options othe than provisional answe key (Master Question Paper) shall not be considered. r (5) Objections and answers suggestedr by the candidate should be in compliance with the responses givenr by him in his answe sheet. Objections shall not be considered, r in case, if responses given in the answe sheet /response sheet and submitted suggestions are differed. (6) Objection fo each question shall be made on separate sheet. Objection fo more than one question in single sheet shall not be considered & treated as cancelled. ઉમેદવાર ે નીચેની સૂચનાઓનું પાલન કરવાની તકેદારી રાખવી, અયથા વાંધા-સૂચન અંગે કર ેલ રજૂઆતો યાને લેવાશે નહીં (1) ઉમેદવારે વાંધા-સૂચનો િનયત કરવામાં આવેલ વાંધા-સૂચન પકથી રજૂ કરવાના રહેશે. -

Parturitional Brain Injury Definition of Parturitional Injury
Parturitional Brain Injury Definition of parturitional injury Thierry A.G.M. Huisman, MD • Any condition that affects the fetus adversely Director Pediatric Radiology and Pediatric Neuroradiology Johns Hopkins Hospital during labor and delivery • May be caused by: – Hypoxia and infection (birth injury) – Mechanical forces (birth trauma) Definition of parturitional injury Introduction • Life starts with a mechanical trauma – Squeezed together by a muscular wrapping • Any condition that affects the fetus adversely – Pushed through a narrow, bony canal with multiple bumps during labor and delivery – Getting your neck extended, rotated and pulled – Life line (umbilical cord) may be compressed – Possibly additional “medieval” instrumentation • May be caused by: – All of this for many minutes or even hours – Hypoxia and infection (birth injury) – Mechanical forces (birth trauma) Introduction Introduction • Life starts with a mechanical trauma • Life starts with a “stress” trauma – Or even worse, within minutes you are squeezed – And than suddenly lots of light, noise and many and “ejected” crying/emotional people around you,…. 1 Subjects who try to relive the „Scientific approach” “I am stuck feeling” Tortuguero expedition. www.philsheldon.wordpress.com Guettler FV, et al. Magnetic resonance imaging of the active second stage of labour: Proof of principle Eur Radiol 2012;22:2020-2026 Epidemiology Epidemiology • Significant variability across the world • Dramatically decreased in last decades • Birth trauma in 3% of all live births • Accounts for less than 2% of neonatal deaths • Even when the injuries are benign, birth trauma may result in significant anxiety for a family Disability adjusted life year (DALY): Measure of overall disease burden expressed as number of years lost due to ill-health, disability or early death Reichard R. -

Alphabetical Index to Diseases and Nature of Injury for Use with Perinatal Conditions (P00-P96)
Subset of alphabetical index to diseases and nature of injury for use with perinatal conditions (P00-P96) SUBSET OF ALPHABETICAL INDEX TO DISEASES AND NATURE OF INJURY FOR USE WITH PERINATAL CONDITIONS (P00-P96) Conditions arising in the perinatal period Conditions arising—continued - abnormal, abnormality—continued Note - Conditions arising in the perinatal - - fetus, fetal period, even though death or morbidity occurs - - - causing disproportion later, should, as far as possible, be coded to - - - - affecting fetus or newborn P03.1 chapter XVI, which takes precedence over - - forces of labor chapters containing codes for diseases by - - - affecting fetus or newborn P03.6 their anatomical site. - - labor NEC - - - affecting fetus or newborn P03.6 These exclude: - - membranes (fetal) Congenital malformations, deformations - - - affecting fetus or newborn P02.9 and chromosomal abnormalities - - - specified type NEC, affecting fetus or (Q00-Q99) newborn P02.8 Endocrine, nutritional and metabolic - - organs or tissues of maternal pelvis diseases (E00-E99) - - - in pregnancy or childbirth Injury, poisoning and certain other - - - - affecting fetus or newborn P03.8 consequences of external causes (S00-T99) - - - - causing obstructed labor Neoplasms (C00-D48) - - - - - affecting fetus or newborn P03.1 Tetanus neonatorum (A33) - - parturition - - - affecting fetus or newborn P03.9 - ablatio, ablation - - presentation (fetus) (see also Presentation, - - placentae (see also Abruptio placentae) fetal, abnormal) - - - affecting fetus or newborn P02.1 -

Operative Vaginal Delivery
FOURTH EDITION OF THE ALARM INTERNATIONAL PROGRAM CHAPTER 18 OPERATIVE VAGINAL DELIVERY Learning Objectives By the end of this chapter, the participant will: 1. Compare and contrast the methods available for operative vaginal delivery including the benefits, risks and indications for each method. 2. Describe the mnemonic for the safe use of vacuum and forceps for operative vaginal delivery. 3. Describe the appropriate documentation that should be recorded after every operative vaginal delivery. Introduction Operative vaginal delivery refers to the use of a vacuum or forceps in vaginal deliveries. Both methods are safe and reliable for assisting childbirth, if appropriate attention is paid to the indications and contraindications for the procedures. The benefits and risks to both the woman and her fetus of using either instrument or the risks associated with proceeding to the alternative of cesarean section delivery must be considered in every case. The choice of instrument should suit both the clinical circumstances, the skill of the health care provider and the acceptance of the woman. The health care provider should have training, experience and judgmental ability with the instrument chosen. Informed consent is an essential step in preparing for an operative vaginal delivery. Operative vaginal delivery should be avoided in women who are HIV positive to reduce mother-to-child transmission. If forceps or vacuum is necessary, avoid performing an episiotomy. Assessing the Descent of the Baby Prior to performing an operative delivery, it is essential to determine that the vertex is fully engaged. Descent of the baby may be assessed abdominally or vaginally. When there is a significant degree of caput (swelling) or molding (overlapping of the fetal skull bones), assessment by abdominal palpation using ―fifths of head palpable‖ is more useful than assessment by vaginal examination. -

ICD-10-Mortality Perinatal Subset - 2017
ICD-10-Mortality Perinatal Subset - 2017 Subset of alphabetical index to diseases and nature of injury for use with perinatal conditions (P00-P96) Conditions arising in the perinatal period Note - Conditions arising in the perinatal period, even though death or morbidity occurs later, should, as far as possible, be coded to chapter XVI, which takes precedence over chapters containing codes for diseases by their anatomical site. These exclude: Congenital malformations, deformations and chromosomal abnormalities (Q00-Q99) Endocrine, nutritional and metabolic diseases (E00-E99) Injury, poisoning and certain other consequences of external causes (S00-T99) Neoplasms (C00-D48) Tetanus neonatorum (A33 2a ) A - ablatio, ablation - - placentae (see also Abruptio placentae) - - - affecting fetus or newborn P02.1 2a - abnormal, abnormality, abnormalities - see also Anomaly - - alphafetoprotein - - - maternal, affecting fetus or newborn P00.8 - - amnion, amniotic fluid - - - affecting fetus or newborn P02.9 - - anticoagulation - - - newborn (transient) P61.6 - - cervix NEC, maternal (acquired) (congenital), in pregnancy or childbirth - - - causing obstructed labor - - - - affecting fetus or newborn P03.1 - - chorion - - - affecting fetus or newborn P02.9 - - coagulation - - - newborn, transient P61.6 - - fetus, fetal - - - causing disproportion - - - - affecting fetus or newborn P03.1 - - forces of labor - - - affecting fetus or newborn P03.6 - - labor NEC - - - affecting fetus or newborn P03.6 - - membranes (fetal) - - - affecting fetus or newborn -

Newborn Payment Policy Applies to the Following Tufts Health Plan Products
Newborn Payment Policy Applies to the following Tufts Health Plan products: ☒ Tufts Health Plan Commercial (including Tufts Health Freedom Plan)1 ☐ Tufts Medicare Preferred HMO (a Medicare Advantage product) ☐ Tufts Health Plan Senior Care Options (SCO) (a dual-eligible product) The following payment policy applies to Tufts Health Plan contracting inpatient facilities and professional providers who render newborn services in an inpatient setting. In addition to the specific information contained in this policy, providers must adhere to the information outlined in the Professional Services and Facilities Payment Policy. Note: Audit and disclaimer information is located at the end of this document. POLICY Tufts Health Plan covers medically necessary well and sick newborn services, in accordance with the member’s benefits and in accordance with federal and applicable state mandate coverage including, but not limited to the provisions of, Chapter 175 Section 47C, Chapter 175 Section 47F and Chapter 176G Section 4. GENERAL BENEFIT INFORMATION Services and subsequent payment are pursuant to the member's benefit plan document. Member eligibility and benefit specifics should be verified prior to initiating services by logging on to the secure Provider website or by contacting Commercial Provider Services. PREVENTIVE SERVICES Due to the Patient Protection and Affordable Care Act (commonly referred to as federal health care reform), with the exception of groups maintaining “grandfathered” status, all Tufts Health Plan products provide 100% coverage for preventive care services. Grandfathered groups are not subject to this requirement, but many have opted to cover preventive services with no cost sharing. This means that most members will have no cost-sharing responsibility when preventive services are rendered by an in-network provider. -

Pregnancy, Labour, Birth and the Early Days of Parenthood Information We Recommend That You Read the Information Within This Book As Your Pregnancy Progresses
Pregnancy, Labour, Birth and the Early Days of Parenthood Information We recommend that you read the information within this book as your pregnancy progresses. Mid Cheshire Hospitals Maternity Services Congratulations on your pregnancy. The staff of the Maternity Unit warmly welcomes you and your family. We wish to offer a safe and high-quality service. Our aim is to be sensitive to your physical and emotional needs and to be flexible in our care so that your individual wishes are met. All healthcare professionals you encounter will respect you as an individual undergoing a significant and emotionally intense life experience. You will be in control, listened to and cared for with compassion. We will give you adequate information, so that you can make informed choices and your consent will be sought for any intervention or treatment offered. We hope that this book will be helpful to you during your pregnancy and after your baby is born. At Mid Cheshire Maternity Unit, we have a Consultant Led Unit and Midwifery Led Unit (MLU) in a semi-rural area undertaking approximately 3000 births per year. Our Maternity Unit provides services for all women. • You will be given the choice of where to their families around problems with drugs, have your baby including; Homebirth, alcohol, mental health, domestic violence Midwifery Led Unit (MLU) or Consultant and abuse. We appreciate it may be difficult Led Unit. During the antenatal period to think about these issues but we are the most suitable place of birth will be committed to making sure you get the help discussed depending on your individual you are entitled to. -

ICD-9-CM Coordination and Maintenance Committee Meeting
ICD-9-CM Coordination and Maintenance Committee Meeting December 6, 2002 Diagnosis Agenda Welcome and announcements Donna Pickett, MPH, RHIA Co-chair, ICD-9-CM C & M Committee Septic shock and Sepsis .......................................................................................................... pg.4-6 Howard Levy, M.D. Eli Lilly and Company Dementia.....................................................................................................................................pg.7 John Hart, M.D. American Academy of Neurology Urologic topics...................................................................................................................... pg.8-12 Scrotal transposition Peyronie=s disease Penile injury Urgency of urination Pre-operative insertion of ureteral stent for ureteral visualization Jeffery Dann, M.D. American Urological Association Impaired fasting glucose...........................................................................................................pg.13 Lavonne Berg, M.D. American Association of Clinical Endocrinologists Carnitine deficiency............................................................................................................ pg.14-15 Rhabdomyolysis........................................................................................................................pg.16 Hypercoagulable states .............................................................................................................pg.17 Hyperaldosteronism..................................................................................................................pg.18 -

Observation of the Newborn Following Vacuum Assisted Birth Identification and Management of Subgaleal Haemorrhage
Observation of the Newborn following Vacuum Assisted Birth Identification and management of subgaleal haemorrhage The aim of the clinical practice guideline is to facilitate an interdisciplinary approach to the prevention, early identification and prompt management of subgaleal haemorrhage in the at risk newborn. Background Although the rate of instrumental delivery remained steady at 10-11%, the rate of vacuum extraction compared with forceps delivery continues to rise1. As the number of births using vacuum extraction has now overtaken forceps deliveries1 (3.5% versus 7.9%) at RPA Women and Babies, it is important to be aware of potential risks and follow clinical practice guidelines relating to the procedure - refer RPA Women and Babies Guideline for Assisted Delivery. Extra cranial Haemorrhage The Cochrane systematic review of trials comparing forceps and vacuum assisted delivery show lower rates of maternal morbidity with vacuum extraction but higher rates of cephalohaematoma, retinal haemorrhages and jaundice in the newborn2,3,4. Nearly all infants delivered with the assistance of vacuum extraction have soft tissue sequelae to the scalp and although these injuries are usually insignificant they can cause anxiety for parents. Scalp abrasions and lacerations are common and are usually associated with more difficult vacuum deliveries such as occiput posterior positions. Retinal haemorrhages occur more commonly with vacuum assisted deliveries compared with forceps deliveries or spontaneous vaginal birth.2 These haemorrhages are usually transient with no long term ophthalmological sequelae. Chignon The chignon or artificial caput succedaneum is caused by a collection of interstitial fluid and small haemorrhages that occur under the cap. It may cross suture lines, is most obvious after immediate removal of the cap and is firm in consistency.