Parturitional Brain Injury Definition of Parturitional Injury
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Journal Pre-Proof
Journal Pre-proof Society for Maternal-Fetal Medicine (SMFM) Consult Series #56: Hepatitis C in Pregnancy: Updated Guidelines Society for Maternal-Fetal Medicine (SMFM), Sarah K. Dotters-Katz, MD MMHPE, Jeffrey A. Kuller, MD, Brenna L. Hughes, MD, MSc PII: S0002-9378(21)00639-6 DOI: https://doi.org/10.1016/j.ajog.2021.06.008 Reference: YMOB 13905 To appear in: American Journal of Obstetrics and Gynecology Please cite this article as: Society for Maternal-Fetal Medicine (SMFM), Dotters-Katz SK, Kuller JA, Hughes BL, Society for Maternal-Fetal Medicine (SMFM) Consult Series #56: Hepatitis C in Pregnancy: Updated Guidelines, American Journal of Obstetrics and Gynecology (2021), doi: https:// doi.org/10.1016/j.ajog.2021.06.008. This is a PDF file of an article that has undergone enhancements after acceptance, such as the addition of a cover page and metadata, and formatting for readability, but it is not yet the definitive version of record. This version will undergo additional copyediting, typesetting and review before it is published in its final form, but we are providing this version to give early visibility of the article. Please note that, during the production process, errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain. © 2021 Published by Elsevier Inc. 1 Society for Maternal-Fetal Medicine (SMFM) Consult Series #56: Hepatitis C in 2 Pregnancy: Updated Guidelines 3 4 Society for Maternal-Fetal Medicine (SMFM); Sarah K. Dotters-Katz, MD MMHPE; Jeffrey A. 5 Kuller, MD; Brenna L. Hughes, MD, MSc 6 7 (Replaces Consult #43, November 2017) 8 9 10 Address all correspondence to: 11 The Society for Maternal-Fetal Medicine: Publications Committee 12 409 12th St, SW 13 Washington, DC 20024 14 Phone: 202-863-2476 15 Fax: 202-554-1132 16 Email: [email protected] Journal Pre-proof 17 18 Reprints will not be available 19 20 Condensation: This Consult reviews the current literature on hepatitis C in pregnancy and 21 provides recommendations based on the available evidence. -

SUBGALEAL HEMATOMA Sarah Meyers MS4 Ilse Castro-Aragon MD CASE HISTORY
SUBGALEAL HEMATOMA Sarah Meyers MS4 Ilse Castro-Aragon MD CASE HISTORY Ex-FT (37w6d) male infant born by low transverse C-section for arrest of descent and chorioamnionitis to a 34-year-old G2P1 mother. The infant had 1- and 5-minute APGAR scores of 9 and 9, weighed 3.625 kg (54th %ile), and had a head circumference of 34.5 cm (30th %ile). Following a challenging delivery of the head during C/s, the infant was noted to have left-sided parietal and occipital bogginess, and an ultrasound was ordered due to concern for subgaleal hematoma. PEDIATRIC HEAD ULTRASOUND: SUBGALEAL HEMATOMA Superficial pediatric head ultrasound showing moderately echogenic fluid collection (green arrow), superficial to the periosteum (blue arrow), crossing the sagittal suture (red arrow). Findings on U/S consistent with large parieto-occipital subgaleal hematoma. PEDIATRIC HEAD ULTRASOUND: SUBGALEAL HEMATOMA Superficial pediatric head ultrasound showing moderately echogenic fluid collection (green arrow), consistent with large parieto-occipital subgaleal hematoma. CLINICAL FOLLOW UP - Subgaleal hematoma was confirmed on ultrasound and the infant was transferred from the newborn nursery to the NICU for close monitoring, including hourly head circumferences and repeat hematocrit measurements - Serial head circumferences remained stable around 34 cm and hematocrit remained stable between 39 and 41 throughout hospital course - The infant was subsequently treated with phototherapy for hyperbilirubinemia, thought to be secondary to resorption of the SGH IN A NUTSHELL: -

N35.12 Postinfective Urethral Stricture, NEC, Female N35.811 Other
N35.12 Postinfective urethral stricture, NEC, female N35.811 Other urethral stricture, male, meatal N35.812 Other urethral bulbous stricture, male N35.813 Other membranous urethral stricture, male N35.814 Other anterior urethral stricture, male, anterior N35.816 Other urethral stricture, male, overlapping sites N35.819 Other urethral stricture, male, unspecified site N35.82 Other urethral stricture, female N35.911 Unspecified urethral stricture, male, meatal N35.912 Unspecified bulbous urethral stricture, male N35.913 Unspecified membranous urethral stricture, male N35.914 Unspecified anterior urethral stricture, male N35.916 Unspecified urethral stricture, male, overlapping sites N35.919 Unspecified urethral stricture, male, unspecified site N35.92 Unspecified urethral stricture, female N36.0 Urethral fistula N36.1 Urethral diverticulum N36.2 Urethral caruncle N36.41 Hypermobility of urethra N36.42 Intrinsic sphincter deficiency (ISD) N36.43 Combined hypermobility of urethra and intrns sphincter defic N36.44 Muscular disorders of urethra N36.5 Urethral false passage N36.8 Other specified disorders of urethra N36.9 Urethral disorder, unspecified N37 Urethral disorders in diseases classified elsewhere N39.0 Urinary tract infection, site not specified N39.3 Stress incontinence (female) (male) N39.41 Urge incontinence N39.42 Incontinence without sensory awareness N39.43 Post-void dribbling N39.44 Nocturnal enuresis N39.45 Continuous leakage N39.46 Mixed incontinence N39.490 Overflow incontinence N39.491 Coital incontinence N39.492 Postural -

Swollen Scalp (Caput Succedaneum and Cephalohematoma) N
n Swollen Scalp (Caput Succedaneum and Cephalohematoma) n What are some possible Some babies are born with swelling or a large bump on the scalp. Caput succedaneum is complications of swollen sculp? swelling under the skin of the scalp, while cepha- With caput succedaneum, complications are rare. lohematoma results from bleeding under the With cephalohematoma, complications occur occasion- scalp. Both conditions are related to pressure on ally: the baby’s head during birth. They are usually harmless. Skull fracture may occur. These fractures usually heal without problems. If the collection of blood is large, it may result in anemia (low hemoglobin). What are caput succedaneum and Large cephalohematomas may result in jaundice. This is cephalohematoma, and what do a yellow color of the skin caused by excess bilirubin, a they look like? substance produced by breakdown of blood as the cepha- lohematoma is resolving. Caput succedaneum. More serious complications, such as bleeding into the Swelling (edema) of the scalp. The swelling is caused by brain or injury to the brain from skull fracture, occur only pressure on the head during delivery. Sometimes there is rarely. bruising, but the swelling is not from blood in the scalp. Occasionally, calcium deposits develop in the area of the There may be swelling and bruising of the face, if your cephalohematoma. This may leave a hard bump that lasts baby was born face first. for several months. Swelling goes down after a few days. When it does, you may notice “molding,” a pointed appearance of your baby’s head that wasn’t obvious before. -

Subset of Alphabetical Index to Diseases and Nature of Injury for Use with Perinatal Conditions (P00-P96)
Subset of alphabetical index to diseases and nature of injury for use with perinatal conditions (P00-P96) SUBSET OF ALPHABETICAL INDEX TO DISEASES AND NATURE OF INJURY FOR USE WITH PERINATAL CONDITIONS (P00-P96) Conditions arising in the perinatal period Conditions arising—continued - abnormal, abnormality—continued Note - Conditions arising in the perinatal - - fetus, fetal period, even though death or morbidity - - - causing disproportion occurs later, should, as far as possible, be - - - - affecting fetus or newborn P03.1 coded to chapter XVI, which takes - - forces of labor precedence over chapters containing codes - - - affecting fetus or newborn P03.6 for diseases by their anatomical site. - - labor NEC - - - affecting fetus or newborn P03.6 These exclude: - - membranes (fetal) Congenital malformations, deformations - - - affecting fetus or newborn P02.9 and chromosomal abnormalities - - - specified type NEC, affecting fetus or (Q00-Q99) newborn P02.8 Endocrine, nutritional and metabolic - - organs or tissues of maternal pelvis diseases (E00-E99) - - - in pregnancy or childbirth Injury, poisoning and certain other - - - - affecting fetus or newborn P03.8 consequences of external causes (S00-T99) - - - - causing obstructed labor Neoplasms (C00-D48) - - - - - affecting fetus or newborn P03.1 Tetanus neonatorum (A33) - - parturition - - - affecting fetus or newborn P03.9 - ablatio, ablation - - presentation (fetus) (see also Presentation, - - placentae (see also Abruptio placentae) fetal, abnormal) - - - affecting fetus or newborn -

Mortality Perinatal Subset, 2013
ICD-10 Mortality Perinatal Subset (2013) Subset of alphabetical index to diseases and nature of injury for use with perinatal conditions (P00-P96) Conditions arising in the perinatal period Note - Conditions arising in the perinatal period, even though death or morbidity occurs later, should, as far as possible, be coded to chapter XVI, which takes precedence over chapters containing codes for diseases by their anatomical site. These exclude: Congenital malformations, deformations and chromosomal abnormalities (Q00-Q99) Endocrine, nutritional and metabolic diseases (E00-E99) Injury, poisoning and certain other consequences of external causes (S00-T99) Neoplasms (C00-D48) Tetanus neonatorum (A33 2a) A -ablatio, ablation - - placentae (see alsoAbruptio placentae) - - - affecting fetus or newborn P02.1 2a -abnormal, abnormality, abnormalities - see also Anomaly - - alphafetoprotein - - - maternal, affecting fetus or newborn P00.8 - - amnion, amniotic fluid - - - affecting fetus or newborn P02.9 - - anticoagulation - - - newborn (transient) P61.6 - - cervix NEC, maternal (acquired) (congenital), in pregnancy or childbirth - - - causing obstructed labor - - - - affecting fetus or newborn P03.1 - - chorion - - - affecting fetus or newborn P02.9 - - coagulation - - - newborn, transient P61.6 - - fetus, fetal 1 ICD-10 Mortality Perinatal Subset (2013) - - - causing disproportion - - - - affecting fetus or newborn P03.1 - - forces of labor - - - affecting fetus or newborn P03.6 - - labor NEC - - - affecting fetus or newborn P03.6 - - membranes -

Hyperbilirubinemia in Term Newborns Needing Phototherapy Within 48 Hours After Birth in a Japanese Birth Center
Kobe J. Med. Sci., Vol. 64, No. 1, pp. E20-E25, 2018 Hyperbilirubinemia in Term Newborns Needing Phototherapy within 48 Hours after Birth in a Japanese Birth Center SAEKO TSUJIMAE1,2, KATSUHIKO YOSHII2, KEIJI YAMANA1, KAZUMICHI FUJIOKA1, KAZUMOTO IIJIMA1 and ICHIRO MORIOKA1,* 1Department of Pediatrics, Kobe University Graduate School of Medicine, Kobe, Japan 2Department of Pediatrics, Chibune General Hospital, Osaka, Japan * Corresponding author Received 12 January 2018 / Accepted 9 February 2018 Keywords: early-onset hyperbilirubinemia, term newborns, total serum bilirubin, unbound bilirubin Background: Hyperbilirubinemia in term newborns needing phototherapy within 48 hours after birth, early-onset hyperbilirubinemia, has not been evaluated in recent Japanese healthy birth centers. In this study, we sought to determine the cause of early-onset hyperbilirubinemia in a Japanese healthy birth center and to evaluate the 1992 Kobe University phototherapy treatment criterion requiring total serum bilirubin (TSB) and unbound bilirubin (UB). Methods: In this retrospective observational study, we collected data on newborns diagnosed with early- onset hyperbilirubinemia between 2009 and 2016 at the Chibune General Hospital. Causes of the disease were investigated, as well as which index (TSB or UB) was used for treatment decisions. Results: Overall, 76 term newborns were included in the analysis. Twenty-seven newborns (36%) found the cause (ABO blood type incompatibility [n=17, 22%], polycythemia [n=8, 11%], and cephalohematoma [n=2, 3%]). However, 49 newborns (64%) did not find any causes (i.e., idiopathic hyperbilirubinemia). Of these, 27 observed more than 5% weight loss from birth weight. Seventy (92%) newborns had abnormal TSB only, and 5 (7%) had abnormal TSB and UB values. -
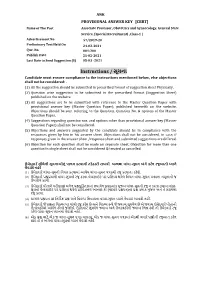
Instructions / સૂચના Candidate Must Ensure Compliance to the Instructions Mentioned Below, Else Objections Shall Not Be Considered:
ANK PROVISIONAL ANSWER KEY [CBRT] Name of The Post Associate Professor, Obstetrics and Gynaecology, General State Service, (Special Recruitment) ,Class-1 | Advertisement No 57/2019-20 Preliminary Test Held On 24-02-2021 Que. No. 001-200 Publish Date 25-02-2021 Last Date to Send Suggestion (S) 05-03 -2021 Instructions / સૂચના Candidate must ensure compliance to the instructions mentioned below, else objections shall not be considered: - (1) All the suggestion should be submitted in prescribed format of suggestion sheet Physically. (2) Question wise suggestion to be submitted in the prescribed formatr (Suggestion rSheet) published on the website.r r (3) All suggestions are to be submitted with reference to the Maste Question Pape withr provisional answe key (Maste Question Paper), published herewith on the website. Objections should be sent referring to the Question, rQuestion No. & options ofr the Maste Question Paper. (4) Suggestions regarding question nos. and options othe than provisional answe key (Master Question Paper) shall not be considered. r (5) Objections and answers suggestedr by the candidate should be in compliance with the responses givenr by him in his answe sheet. Objections shall not be considered, r in case, if responses given in the answe sheet /response sheet and submitted suggestions are differed. (6) Objection fo each question shall be made on separate sheet. Objection fo more than one question in single sheet shall not be considered & treated as cancelled. ઉમેદવાર ે નીચેની સૂચનાઓનું પાલન કરવાની તકેદારી રાખવી, અયથા વાંધા-સૂચન અંગે કર ેલ રજૂઆતો યાને લેવાશે નહીં (1) ઉમેદવારે વાંધા-સૂચનો િનયત કરવામાં આવેલ વાંધા-સૂચન પકથી રજૂ કરવાના રહેશે. -

Managing the Jaundiced Newborn: a Persistent Challenge
CMAJ Review CME Managing the jaundiced newborn: a persistent challenge M. Jeffrey Maisels MB BCh DSc See related infographic, www.cmaj.ca/lookup/suppl/doi:10.1503/cmaj.122117/-/DC1 ediatricians and family physicians deal regu- bin level that is above the normal maximum adult Competing interests: larly with jaundiced newborn infants who level of 17.1 μmol/L (1 mg/dL) because they have Jeffrey Maisels is a consultant to Dräger Pemerge unscathed from their transient expo- an increased turnover of erythrocytes, produce Medical Inc., the supplier of sure to an elevated serum bilirubin level. Yet, more than twice the amount of bilirubin produced the JM-103 transcutaneous despite published guidelines for the management of daily by an adult9 and have a transient deficiency in bilirubinometer. neonatal jaundice, there are rare infants in whom their ability to conjugate and clear bilirubin. This This article has been peer bilirubin encephalopathy develops. Canada cur- imbalance between bilirubin production and conju- reviewed. rently reports the highest incidence in the devel- gation is fundamental to the pathogenesis of neona- Correspondence to: oped world of 1 in 67 000 to 1 in 44 000 live births.1 tal bilirubinemia.10 It results in a steady increase in M. Jeffrey Maisels, jmaisels In this review, I present an approach to manag- total serum bilirubin levels for the first three to five @beaumont.edu ing the jaundiced newborn that is based on pub- days, and sometimes more (Figure 1), followed by CMAJ 2015. DOI:10.1503 lished guidelines.2–5 The aim is to help clinicians a decrease in levels as the rate of bilirubin produc- /cmaj.122117 identify and manage jaundice in the newborn, in- tion declines and conjugation improves. -

AMERICAN ACADEMY of PEDIATRICS Management of Hyperbilirubinemia in the Newborn Infant 35 Or More Weeks of Gestation
AMERICAN ACADEMY OF PEDIATRICS CLINICAL PRACTICE GUIDELINE Subcommittee on Hyperbilirubinemia Management of Hyperbilirubinemia in the Newborn Infant 35 or More Weeks of Gestation ABSTRACT. Jaundice occurs in most newborn infants. Hyperbilirubinemia”3 for a description of the meth- Most jaundice is benign, but because of the potential odology, questions addressed, and conclusions of toxicity of bilirubin, newborn infants must be monitored this report.) This guideline is intended for use by to identify those who might develop severe hyperbili- hospitals and pediatricians, neonatologists, family rubinemia and, in rare cases, acute bilirubin encephalop- physicians, physician assistants, and advanced prac- athy or kernicterus. The focus of this guideline is to tice nurses who treat newborn infants in the hospital reduce the incidence of severe hyperbilirubinemia and bilirubin encephalopathy while minimizing the risks of and as outpatients. A list of frequently asked ques- unintended harm such as maternal anxiety, decreased tions and answers for parents is available in English breastfeeding, and unnecessary costs or treatment. Al- and Spanish at www.aap.org/family/jaundicefaq. though kernicterus should almost always be prevent- htm. able, cases continue to occur. These guidelines provide a framework for the prevention and management of DEFINITION OF RECOMMENDATIONS hyperbilirubinemia in newborn infants of 35 or more The evidence-based approach to guideline devel- weeks of gestation. In every infant, we recommend that clinicians 1) promote and support successful breastfeed- opment requires that the evidence in support of a ing; 2) perform a systematic assessment before discharge policy be identified, appraised, and summarized and for the risk of severe hyperbilirubinemia; 3) provide that an explicit link between evidence and recom- early and focused follow-up based on the risk assess- mendations be defined. -

Point-Of-Care Ultrasound to Distinguish Subgaleal and Cephalohematoma: Case Report
Case Report Point-of-care Ultrasound to Distinguish Subgaleal and Cephalohematoma: Case Report Josie Acuña, MD University of Arizona, Department of Emergency Medicine, Tucson, Arizona Srikar Adhikari, MD, MS Section Editor: Shadi Lahham, MD, MS Submission history: Submitted December 29, 2020; Revision received February 19, 2021; Accepted March 5, 2021 Electronically published April 19, 2021 Full text available through open access at http://escholarship.org/uc/uciem_cpcem DOI: 10.5811/cpcem.2021.3.51375 Introduction: Cephalohematomas generally do not pose a significant risk to the patient and resolve spontaneously. Conversely, a subgaleal hematoma is a rare but more serious condition. While it may be challenging to make this diagnostic distinction based on a physical examination alone, the findings that differentiate these two conditions can be appreciated on point-of-care ultrasound (POCUS). We describe two pediatric patient cases where POCUS was used to distinguish between a subgaleal hematoma and a cephalohematoma. Case Reports: We describe one case of a 14-month-old male brought to the pediatric emergency department (PED) with concern for head injury. A POCUS examination revealed a large fluid collection that did not cross the sagittal suture. Thus, the hematoma was more consistent with a cephalohematoma and less compatible with a subgaleal hematoma. Given these findings, further emergent imaging was deferred in the PED and the patient was kept for observation. In the second case an 8-week-old male presented with suspected swelling over the right parietal region. A POCUS examination was performed, which demonstrated an extensive, simple fluid collection that extended across the suture line, making it more concerning for a subgaleal hematoma. -

Alphabetical Index to Diseases and Nature of Injury for Use with Perinatal Conditions (P00-P96)
Subset of alphabetical index to diseases and nature of injury for use with perinatal conditions (P00-P96) SUBSET OF ALPHABETICAL INDEX TO DISEASES AND NATURE OF INJURY FOR USE WITH PERINATAL CONDITIONS (P00-P96) Conditions arising in the perinatal period Conditions arising—continued - abnormal, abnormality—continued Note - Conditions arising in the perinatal - - fetus, fetal period, even though death or morbidity occurs - - - causing disproportion later, should, as far as possible, be coded to - - - - affecting fetus or newborn P03.1 chapter XVI, which takes precedence over - - forces of labor chapters containing codes for diseases by - - - affecting fetus or newborn P03.6 their anatomical site. - - labor NEC - - - affecting fetus or newborn P03.6 These exclude: - - membranes (fetal) Congenital malformations, deformations - - - affecting fetus or newborn P02.9 and chromosomal abnormalities - - - specified type NEC, affecting fetus or (Q00-Q99) newborn P02.8 Endocrine, nutritional and metabolic - - organs or tissues of maternal pelvis diseases (E00-E99) - - - in pregnancy or childbirth Injury, poisoning and certain other - - - - affecting fetus or newborn P03.8 consequences of external causes (S00-T99) - - - - causing obstructed labor Neoplasms (C00-D48) - - - - - affecting fetus or newborn P03.1 Tetanus neonatorum (A33) - - parturition - - - affecting fetus or newborn P03.9 - ablatio, ablation - - presentation (fetus) (see also Presentation, - - placentae (see also Abruptio placentae) fetal, abnormal) - - - affecting fetus or newborn P02.1