The Role of Cflip in Regulatory T Cell Homeostasis
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Epigenetic Reprogramming Sensitizes CML Stem Cells to Combined EZH2 and Tyrosine
Published OnlineFirst September 14, 2016; DOI: 10.1158/2159-8290.CD-16-0263 RESEARCH BRIEF Epigenetic Reprogramming Sensitizes CML Stem Cells to Combined EZH2 and Tyrosine Kinase Inhibition Mary T. Scott 1 , 2 , Koorosh Korfi 1 , 2 , Peter Saffrey 1 , Lisa E.M. Hopcroft 2 , Ross Kinstrie 1 , Francesca Pellicano 2 , Carla Guenther 1 , 2 , Paolo Gallipoli 2 , Michelle Cruz 1 , Karen Dunn 2 , Heather G. Jorgensen 2 , Jennifer E. Cassels 2 , Ashley Hamilton 2 , Andrew Crossan 1 , Amy Sinclair 2 , Tessa L. Holyoake 2 , and David Vetrie 1 ABSTRACT A major obstacle to curing chronic myeloid leukemia (CML) is residual disease main- tained by tyrosine kinase inhibitor (TKI)–persistent leukemic stem cells (LSC). These are BCR–ABL1 kinase independent, refractory to apoptosis, and serve as a reservoir to drive relapse or TKI resistance. We demonstrate that Polycomb Repressive Complex 2 is misregulated in chronic phase CML LSCs. This is associated with extensive reprogramming of H3K27me3 targets in LSCs, thus sensi- tizing them to apoptosis upon treatment with an EZH2-specifi c inhibitor (EZH2i). EZH2i does not impair normal hematopoietic stem cell survival. Strikingly, treatment of primary CML cells with either EZH2i or TKI alone caused signifi cant upregulation of H3K27me3 targets, and combined treatment further potentiated these effects and resulted in signifi cant loss of LSCs compared to TKI alone, in vitro , and in long-term bone marrow murine xenografts. Our fi ndings point to a promising epigenetic-based thera- peutic strategy to more effectively target LSCs in patients with CML receiving TKIs. SIGNIFICANCE: In CML, TKI-persistent LSCs remain an obstacle to cure, and approaches to eradicate them remain a signifi cant unmet clinical need. -

Gene Essentiality Landscape and Druggable Oncogenic Dependencies in Herpesviral Primary Effusion Lymphoma
ARTICLE DOI: 10.1038/s41467-018-05506-9 OPEN Gene essentiality landscape and druggable oncogenic dependencies in herpesviral primary effusion lymphoma Mark Manzano1, Ajinkya Patil1, Alexander Waldrop2, Sandeep S. Dave2, Amir Behdad3 & Eva Gottwein1 Primary effusion lymphoma (PEL) is caused by Kaposi’s sarcoma-associated herpesvirus. Our understanding of PEL is poor and therefore treatment strategies are lacking. To address this 1234567890():,; need, we conducted genome-wide CRISPR/Cas9 knockout screens in eight PEL cell lines. Integration with data from unrelated cancers identifies 210 genes as PEL-specific oncogenic dependencies. Genetic requirements of PEL cell lines are largely independent of Epstein-Barr virus co-infection. Genes of the NF-κB pathway are individually non-essential. Instead, we demonstrate requirements for IRF4 and MDM2. PEL cell lines depend on cellular cyclin D2 and c-FLIP despite expression of viral homologs. Moreover, PEL cell lines are addicted to high levels of MCL1 expression, which are also evident in PEL tumors. Strong dependencies on cyclin D2 and MCL1 render PEL cell lines highly sensitive to palbociclib and S63845. In summary, this work comprehensively identifies genetic dependencies in PEL cell lines and identifies novel strategies for therapeutic intervention. 1 Department of Microbiology-Immunology, Feinberg School of Medicine, Northwestern University, Chicago, IL 60611, USA. 2 Duke Cancer Institute and Center for Genomic and Computational Biology, Duke University, Durham, NC 27708, USA. 3 Department of Pathology, Feinberg School of Medicine, Northwestern University, Chicago, IL 60611, USA. Correspondence and requests for materials should be addressed to E.G. (email: [email protected]) NATURE COMMUNICATIONS | (2018) 9:3263 | DOI: 10.1038/s41467-018-05506-9 | www.nature.com/naturecommunications 1 ARTICLE NATURE COMMUNICATIONS | DOI: 10.1038/s41467-018-05506-9 he human oncogenic γ-herpesvirus Kaposi’s sarcoma- (IRF4), a critical oncogene in multiple myeloma33. -
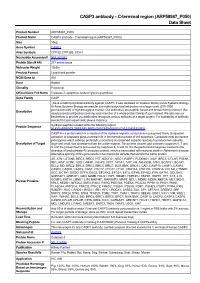
C-Terminal Region (ARP58987 P050) Data Sheet
CASP3 antibody - C-terminal region (ARP58987_P050) Data Sheet Product Number ARP58987_P050 Product Name CASP3 antibody - C-terminal region (ARP58987_P050) Size 50ug Gene Symbol CASP3 Alias Symbols CPP32; CPP32B; SCA-1 Nucleotide Accession# NM_032991 Protein Size (# AA) 277 amino acids Molecular Weight 12kDa Product Format Lyophilized powder NCBI Gene Id 836 Host Rabbit Clonality Polyclonal Official Gene Full Name Caspase 3, apoptosis-related cysteine peptidase Gene Family CASP This is a rabbit polyclonal antibody against CASP3. It was validated on Western Blot by Aviva Systems Biology. At Aviva Systems Biology we manufacture rabbit polyclonal antibodies on a large scale (200-1000 Description products/month) of high throughput manner. Our antibodies are peptide based and protein family oriented. We usually provide antibodies covering each member of a whole protein family of your interest. We also use our best efforts to provide you antibodies recognize various epitopes of a target protein. For availability of antibody needed for your experiment, please inquire (). Peptide Sequence Synthetic peptide located within the following region: NLKYEVRNKNDLTREEIVELMRDVSKEDHSKRSSFVCVLLSHGEEGIIFG CASP3 is a protein which is a member of the cysteine-aspartic acid protease (caspase) family. Sequential activation of caspases plays a central role in the execution-phase of cell apoptosis. Caspases exist as inactive proenzymes which undergo proteolytic processing at conserved aspartic residues to produce two subunits, Description of Target large and small, that dimerize to form the active enzyme. This protein cleaves and activates caspases 6, 7 and 9, and the protein itself is processed by caspases 8, 9 and 10. It is the predominant caspase involved in the cleavage of amyloid-beta 4A precursor protein, which is associated with neuronal death in Alzheimer's disease. -

Supplementary Material and Methods
Supplementary material and methods Generation of cultured human epidermal sheets Normal human epidermal keratinocytes were isolated from human breast skin. Keratinocytes were grown on a feeder layer of irradiated human fibroblasts pre-seeded at 4000 cells /cm² in keratinocyte culture medium (KCM) containing a mix of 3:1 DMEM and HAM’s F12 (Invitrogen, Carlsbad, USA), supplemented with 10% FCS, 10ng/ml epidermal growth factor (EGF; R&D systems, Minneapolis, MN, USA), 0.12 IU/ml insulin (Lilly, Saint- Cloud, France), 0.4 mg/ml hydrocortisone (UpJohn, St Quentin en Yvelelines, France) , 5 mg/ml triiodo-L- thyronine (Sigma, St Quentin Fallavier, France), 24.3 mg/ml adenine (Sigma), isoproterenol (Isuprel, Hospira France, Meudon, France) and antibiotics (20 mg/ml gentamicin (Phanpharma, Fougères, France), 100 IU/ml penicillin (Phanpharma), and 1 mg/ml amphotericin B (Phanpharma)). The medium was changed every two days. NHEK were then cultured over a period of 13 days according to the protocol currently used at the Bank of Tissues and Cells for the generation of clinical grade epidermal sheets used for the treatment of severe extended burns (Ref). When needed, cells were harvested with trypsin-EDTA 0.05% (Thermo Fisher Scientific, Waltham, MA, USA) and collected for analysis. Clonogenic assay Keratinocytes were seeded on a feeder layer of irradiated fibroblasts, at a clonal density of 10-20 cells/cm² and cultivated for 10 to 14 days. Three flasks per tested condition were fixed and colored in a single 30 mns step using rhodamine B (Sigma) diluted at 0.01 g/ml in 4% paraformaldehyde. In each tested condition, cells from 3 other flasks were numerated after detachment by trypsin treatment. -

The Human Cytomegalovirus–Encoded Chemokine Receptor US28 Promotes Angiogenesis and Tumor Formation Via Cyclooxygenase-2
Published OnlineFirst March 24, 2009; DOI: 10.1158/0008-5472.CAN-08-2487 Research Article The Human Cytomegalovirus–Encoded Chemokine Receptor US28 Promotes Angiogenesis and Tumor Formation via Cyclooxygenase-2 David Maussang,1 Ellen Langemeijer,1 Carlos P. Fitzsimons,1 Marijke Stigter-van Walsum,2 Remco Dijkman,3 Martin K. Borg,3 Erik Slinger,1 Andreas Schreiber,4 Detlef Michel,4 Cornelis P. Tensen,3 Guus A.M.S. van Dongen,2 Rob Leurs,1 and Martine J. Smit1 1Leiden/Amsterdam Center for Drug Research, Division of Medicinal Chemistry, Faculty of Sciences, Vrije Universiteit Amsterdam; 2Department of Otolaryngology/Head and Neck Surgery, Vrije Universiteit Medical Center, Amsterdam, the Netherlands; 3Department of Dermatology, Leiden University Medical Center, Leiden, the Netherlands; and 4Institute of Virology, University Clinic Ulm, Ulm, Germany Abstract considered an oncogenic herpesvirus (5), but it has been suggested The human cytomegalovirus (HCMV), potentially associated to act as an oncomodulator (6). The presence of HCMV proteins with the development of malignancies, encodes the constitu- has been detected in several malignancies, such as colon cancer (7), tively active chemokine receptor US28. Previously, we have malignant glioblastoma (8), and breast cancer (9). Importantly, shown that US28 expression induces an oncogenic phenotype HCMV preferably infects tumor cells, leading to enhanced cell both in vitro and in vivo. Microarray analysis revealed proliferation, angiogenesis, and resistance to apoptosis (6, 10). differential expression of genes involved in oncogenic signal- Of interest, most herpesviruses contain one or more genes that ing in US28-expressing NIH-3T3 cells. In particular, the encode for constitutively active G-protein coupled receptors (1). -

MIND Bomb 2 Prevents RIPK1 Kinase Activity-Dependent and -Independent Apoptosis Through Ubiquitylation of Cflipl
ARTICLE https://doi.org/10.1038/s42003-020-01603-y OPEN MIND bomb 2 prevents RIPK1 kinase activity-dependent and -independent apoptosis through ubiquitylation of cFLIPL Osamu Nakabayashi 1, Hirotaka Takahashi2, Kenta Moriwaki1, Sachiko Komazawa-Sakon1, Fumiaki Ohtake3, 1234567890():,; Shin Murai 1, Yuichi Tsuchiya1, Yuki Koyahara1, Yasushi Saeki 4, Yukiko Yoshida4, Soh Yamazaki1, ✉ Fuminori Tokunaga 5, Tatsuya Sawasaki 2 & Hiroyasu Nakano 1 Mind bomb 2 (MIB2) is an E3 ligase involved in Notch signalling and attenuates TNF-induced apoptosis through ubiquitylation of receptor-interacting protein kinase 1 (RIPK1) and cylin- dromatosis. Here we show that MIB2 bound and conjugated K48– and K63–linked poly- ubiquitin chains to a long-form of cellular FLICE-inhibitory protein (cFLIPL), a catalytically inactive homologue of caspase 8. Deletion of MIB2 did not impair the TNF-induced complex I formation that mediates NF-κB activation but significantly enhanced formation of cytosolic death-inducing signalling complex II. TNF-induced RIPK1 Ser166 phosphorylation, a hallmark of RIPK1 death-inducing activity, was enhanced in MIB2 knockout cells, as was RIPK1 kinase activity-dependent and -independent apoptosis. Moreover, RIPK1 kinase activity-independent apoptosis was induced in cells expressing cFLIPL mutants lacking MIB2-dependent ubiqui- tylation. Together, these results suggest that MIB2 suppresses both RIPK1 kinase activity- dependent and -independent apoptosis, through suppression of RIPK1 kinase activity and ubiquitylation of cFLIPL, respectively. 1 Department of Biochemistry, Toho University School of Medicine, 5-21-16 Omori-Nishi, Ota-ku, Tokyo 143-8540, Japan. 2 Division of Cell-Free Sciences, Proteo-Science Center (PROS), 3 Bunkyo-cho, Matsuyama, Ehime 790-8577, Japan. -

The Pseudo-Caspase FLIP(L) Regulates Cell Fate Following P53 Activation
The pseudo-caspase FLIP(L) regulates cell fate following p53 activation Andrea Leesa,1, Alexander J. McIntyrea,1, Nyree T. Crawforda, Fiammetta Falconea, Christopher McCanna, Caitriona Holohana, Gerard P. Quinna, Jamie Z. Robertsa, Tamas Sesslera, Peter F. Gallaghera, Gemma M. A. Gregga, Katherine McAllistera, Kirsty M. McLaughlina, Wendy L. Allena, Laurence J. Eganb, Aideen E. Ryanb,c, Melissa J. Labonte-Wilsona, Philip D. Dunnea, Mark Wappetta, Vicky M. Coylea, Patrick G. Johnstona, Emma M. Kerra, Daniel B. Longleya,2,3, and Simon S. McDadea,2,3 aPatrick G Johnston Centre for Cancer Research, Queen’s University Belfast, Belfast, Northern Ireland BT9 7BL, United Kingdom; bDiscipline of Pharmacology & Therapeutics, Lambe Institute for Translational Research, School of Medicine, College of Medicine, Nursing and Health Sciences, National University of Ireland Galway, Galway, Ireland; and cRegenerative Medicine Institute, College of Medicine, Nursing and Health Sciences, National University of Ireland Galway, Galway, Ireland Edited by Karen H. Vousden, Francis Crick Institute, London, United Kingdom, and approved June 8, 2020 (received for review February 12, 2020) p53 is the most frequently mutated, well-studied tumor-suppressor switch from cell-cycle arrest to cell death induction remain gene, yet the molecular basis of the switch from p53-induced cell- poorly understood, although p53-mediated transcriptional up- cycle arrest to apoptosis remains poorly understood. Using a combi- regulation of PUMA has been suggested to be crucial in a nation of transcriptomics and functional genomics, we unexpectedly number of studies (10, 11). identified a nodal role for the caspase-8 paralog and only human Despite p53/TP53 being the most frequently mutated gene in pseudo-caspase, FLIP(L), in regulating this switch. -

The Human Gene Connectome As a Map of Short Cuts for Morbid Allele Discovery
The human gene connectome as a map of short cuts for morbid allele discovery Yuval Itana,1, Shen-Ying Zhanga,b, Guillaume Vogta,b, Avinash Abhyankara, Melina Hermana, Patrick Nitschkec, Dror Friedd, Lluis Quintana-Murcie, Laurent Abela,b, and Jean-Laurent Casanovaa,b,f aSt. Giles Laboratory of Human Genetics of Infectious Diseases, Rockefeller Branch, The Rockefeller University, New York, NY 10065; bLaboratory of Human Genetics of Infectious Diseases, Necker Branch, Paris Descartes University, Institut National de la Santé et de la Recherche Médicale U980, Necker Medical School, 75015 Paris, France; cPlateforme Bioinformatique, Université Paris Descartes, 75116 Paris, France; dDepartment of Computer Science, Ben-Gurion University of the Negev, Beer-Sheva 84105, Israel; eUnit of Human Evolutionary Genetics, Centre National de la Recherche Scientifique, Unité de Recherche Associée 3012, Institut Pasteur, F-75015 Paris, France; and fPediatric Immunology-Hematology Unit, Necker Hospital for Sick Children, 75015 Paris, France Edited* by Bruce Beutler, University of Texas Southwestern Medical Center, Dallas, TX, and approved February 15, 2013 (received for review October 19, 2012) High-throughput genomic data reveal thousands of gene variants to detect a single mutated gene, with the other polymorphic genes per patient, and it is often difficult to determine which of these being of less interest. This goes some way to explaining why, variants underlies disease in a given individual. However, at the despite the abundance of NGS data, the discovery of disease- population level, there may be some degree of phenotypic homo- causing alleles from such data remains somewhat limited. geneity, with alterations of specific physiological pathways under- We developed the human gene connectome (HGC) to over- come this problem. -

NIK Controls Classical and Alternative NF-Kb Activation and Is Necessary for the Survival of Human T-Cell Lymphoma Cells
Published OnlineFirst March 27, 2013; DOI: 10.1158/1078-0432.CCR-12-3151 Clinical Cancer Human Cancer Biology Research NIK Controls Classical and Alternative NF-kB Activation and Is Necessary for the Survival of Human T-cell Lymphoma Cells Lina Odqvist1, Margarita Sanchez-Beato 1,3, Santiago Montes-Moreno1,10, Esperanza Martín-Sanchez 1, Raquel Pajares2, Lydia Sanchez-Verde 2, Pablo L. Ortiz-Romero4, Jose Rodriguez5, Socorro M. Rodríguez-Pinilla1,6, Francisca Iniesta-Martínez9, Juan Carlos Solera-Arroyo11, Rafael Ramos-Asensio12, Teresa Flores13, Javier Menarguez Palanca7, Federico García Bragado14, Purificacion Domínguez Franjo8, and Miguel A. Piris1,10 Abstract Purpose: Peripheral T-cell lymphomas (PTCL) are a heterogeneous entity of neoplasms with poor prognosis, a lack of effective therapies, and a largely unknown molecular pathology. Deregulated NF-kB activity has been associated with several lymphoproliferative diseases, but its importance in T-cell lymphomagenesis is poorly understood. We investigated the function of the NF-kB–inducing kinase (NIK), in this pathway and its role as a potential molecular target in T-cell lymphomas. Experimental Design: We used immunohistochemistry to analyze the expression of different NF-kB members in primary human PTCL samples and to study its clinical impact. With the aim of inhibiting the pathway, we used genetic silencing of NIK in several T-cell lymphoma cell lines and observed its effect on downstream targets and cell viability. Results: We showed that the NF-kB pathway was activated in a subset of PTCLs associated with poor overall survival. NIK was overexpressed in a number of PTCL cell lines and primary samples, and a pivotal role for NIK in the survival of these tumor cells was unveiled. -

BIIB021, an Hsp90 Inhibitor: a Promising Therapeutic Strategy for Blood Malignancies (Review)
ONCOLOGY REPORTS 40: 3-15, 2018 BIIB021, an Hsp90 inhibitor: A promising therapeutic strategy for blood malignancies (Review) WEI HE and HUIXIAN HU Department of Hematology, Jinhua Municipal Central Hospital, Jinhua, Zhejiang 321000, P.R. China Received August 25, 2017; Accepted April 17, 2018 DOI: 10.3892/or.2018.6422 Abstract. Heat shock proteins (HSPs) are molecular chaper- a benzoquinone antineoplastic antibiotic isolated from the ones that are consistently increased to help cells survive under bacterium Streptomyces hygroscopicus, and its derivative, conditions of stress. As a member of the Hsps, Hsp90 is involved 17‑AAG, were first developed as Hsp90 inhibitors and exhib- in protein post-translational maturation and disposition. This ited effective anticancer potency. Whereas, severe side effects protein is ubiquitously expressed in normal cells. However, in and low solubility restricted their application at the clinical cancer cells and particularly in hematological malignancies, level, BIIB021, a novel and fully synthetic inhibitor of Hsp90, Hsp90 is unexpectedly abundant to maintain levels of proteins is water soluble and well-tolerated. Beyond degrading onco- vital for cancer pathology. Hsp90 inhibitors can target the ATP genic protein, BIIB021 can overcome multidrug resistance and domain of Hsp90 and prohibit its exchange of ADP for ATP, potentiate the effects of other therapeutics. phase I/II trials leading to the degradation of client proteins and disruption of have been conducted to evaluate the dosing schedules and signaling cascades. Concomitantly, Hsp90 inhibitors induce activity of this agent. The present review focuses on the anti- tumor cell apoptosis, promote cell cycle arrest and abrogate tumor profile of BIIB021. -

Alterations of the Pro-Survival Bcl-2 Protein Interactome in Breast Cancer
bioRxiv preprint doi: https://doi.org/10.1101/695379; this version posted July 12, 2019. The copyright holder for this preprint (which was not certified by peer review) is the author/funder, who has granted bioRxiv a license to display the preprint in perpetuity. It is made available under aCC-BY-NC-ND 4.0 International license. 1 Alterations of the pro-survival Bcl-2 protein interactome in 2 breast cancer at the transcriptional, mutational and 3 structural level 4 5 Simon Mathis Kønig1, Vendela Rissler1, Thilde Terkelsen1, Matteo Lambrughi1, Elena 6 Papaleo1,2 * 7 1Computational Biology Laboratory, Danish Cancer Society Research Center, 8 Strandboulevarden 49, 2100, Copenhagen 9 10 2Translational Disease Systems Biology, Faculty of Health and Medical Sciences, Novo 11 Nordisk Foundation Center for Protein Research University of Copenhagen, Copenhagen, 12 Denmark 13 14 Abstract 15 16 Apoptosis is an essential defensive mechanism against tumorigenesis. Proteins of the B-cell 17 lymphoma-2 (Bcl-2) family regulates programmed cell death by the mitochondrial apoptosis 18 pathway. In response to intracellular stresses, the apoptotic balance is governed by interactions 19 of three distinct subgroups of proteins; the activator/sensitizer BH3 (Bcl-2 homology 3)-only 20 proteins, the pro-survival, and the pro-apoptotic executioner proteins. Changes in expression 21 levels, stability, and functional impairment of pro-survival proteins can lead to an imbalance 22 in tissue homeostasis. Their overexpression or hyperactivation can result in oncogenic effects. 23 Pro-survival Bcl-2 family members carry out their function by binding the BH3 short linear 24 motif of pro-apoptotic proteins in a modular way, creating a complex network of protein- 25 protein interactions. -
Func6onal Profiling from Babelomics 5
Func%onal profiling from Babelomics 5 Dan Crespo [email protected] March 3th, 2016 Where are we? General NGS pipeline: Func9onal analysis: • Single enrichment: Fa9GO • Gene set enrichment: Logisc Model Genomics Transcriptomics Where are we? Func9onal analysis Implemented in: Differenal expression hp://babelomics.org Genes Gene Sets Fa9GO GSA logisc model Ques9ons we try to answer • Is there any significant func%onal enrichment in my gene list / gene sets? Ques9ons we try to answer • Is there any significat func%onal enrichment in my gene list / gene sets? • Are these genes involved in common pathways? Ques9ons we try to answer • Is there any significat func%onal enrichment in my gene list / gene sets? • Are these genes involved in common pathways? • Do they share specific regulaon? Ques9ons we try to answer • Is there any significat func%onal enrichment in my gene list / gene sets? • Are these genes involved in common pathways? • Do they share specific regulaon? • Are they involved in the same disease? Babelomics 5: FaGO Single enrichment Comparison between two list of genes with user defined annotaons Single enrichment Comparison between two list of genes with user defined annotaons List 1: User provided List 2: Func9onal annotaons: • Gene symbols • User provided • Pre-defined annotaons • Probe Ids • Rest of genome • Custom annotaons • Entrez Ids … • Complementary list Mul9ple tesng context Fisher exact test Benjamini – Hochberg p-value correcon Ranked results Single enrichment List 1 List 2 Func9onal annotaons AATF BIRC7 CIAS1 PEA15 ACTA1 DNAI1 KIF3B