ABSTRACT RICHARDS, ANDREW LATIMER. Experimental
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Pet Shop Boys Discography (The Complete Singles Collection) Mp3, Flac, Wma
Pet Shop Boys Discography (The Complete Singles Collection) mp3, flac, wma DOWNLOAD LINKS (Clickable) Genre: Electronic Album: Discography (The Complete Singles Collection) Country: UK Released: 1991 Style: Synth-pop MP3 version RAR size: 1810 mb FLAC version RAR size: 1420 mb WMA version RAR size: 1355 mb Rating: 4.5 Votes: 255 Other Formats: VOC VQF AU WAV MIDI DMF DTS Tracklist Hide Credits West End Girls 1 4:00 Engineer – David JacobProducer – Stephen HagueWritten-By – Tennant / Lowe Love Comes Quickly 2 4:18 Engineer – David JacobProducer – Stephen HagueWritten-By – Hague*, Tennant / Lowe Opportunities (Let's Make Lots Of Money) Producer [Additional Production], Remix – Stephen HagueProducer [New York Overdubs] – 3 3:38 Ron Dean MillerProducer [Original Recording] – J.J. Jeczalik, Nicholas FroomeWritten-By – Tennant / Lowe Suburbia 4 4:04 Producer, Engineer – Julian MendelsohnWritten-By – Tennant / Lowe It's A Sin 5 Mixed By, Producer [Additional] – Stephen HagueProducer, Engineer – Julian 5:01 MendelsohnWritten-By – Tennant / Lowe What Have I Done To Deserve This? 6 Engineer – David JacobMixed By – Julian MendelsohnProducer – Stephen HagueVocals – 4:20 Dusty SpringfieldWritten-By – Willis*, Tennant / Lowe Rent 7 Mixed By – Stephen HagueProducer, Engineer – Julian MendelsohnWritten-By – Tennant / 3:33 Lowe Always On My Mind 8 Producer – Julian Mendelsohn, Pet Shop BoysProducer [Original Track] – David 3:54 JacobWritten-By – Christopher*, James*, Thompson* Heart 9 Engineer – Tony PhillipsProducer – Andy Richards, Pet Shop BoysWritten-By -

Slap Magazine: Issue 67 (March 2017)
Issue 67 Mar2017 FREE Lamb & Flag The Tything, Worcester, WR1 1JL Fantastic Food, Superior Craft Ales Cocktails & Exceptional Guinness... Folk Music, Poetry Conkers! Local Cider, Backgammon, Tradition We Have It All!! Fresh, Homemade, Authentic Italian Cuisine Thurs - Sun Cocktail Master Class! Open 7 Days - Parties & Functions Catered For [email protected] Tel: 01905 729415 www.twocraftybrewers.co.uk Well February shot by in the blink of an eye and here we are again! Welcome to the March edition of Slap. I was hoping to say ‘Spring is in the air’ but I’ve just seen the weather forecast and it’s far from Spring-like. It really feels like it’s been a long winter of discontent with news of more venue closures almost weekly. The latest to go at the end of February was the Pig and Drum in Worcester which has been prominent on the local music seen for a few years now. Thanks to the efforts of landlady Rachel Cale bands from out of town loved playing there. We don’t yet know the long term fate of the Boar’s Mar 2017 Head in Kidderminster since Sid & Sandra announced they’re moving on in the summer, But I don’t think it’ll be the last to go. With business rates rises due very soon and so many people feeling the pinch, these places are really suffering. There are SLAP MAGAZINE rumours of other venues around the counties who may also be Unit 3a, Lowesmoor Wharf, shutting their doors soon. And It’s not just the music scene that Worcester WR1 2RS suffers either, many of these spaces are now multi functional art Telephone: 01905 26660 spaces as well as platforms for comedy, spoken word and poetry. -
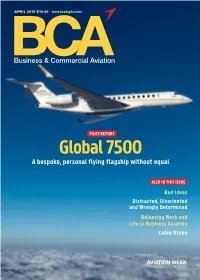
April 2019 Vol
BUSINESS & COMMERCIAL AVIATION PILOT REPORT: GLOBAL 7500 CABIN APRIL 2019 $10.00 www.bcadigital.com Business & Commercial Aviation PILOT REPORT OZONE WORK/LIFE BALANCE APRIL 2019 VOL. 115 NO. 4 Global 7500 A bespoke, personal flying flagship without equal ALSO IN THIS ISSUE Bad Ideas Distracted, Disoriented and Wrongly Determined Balancing Work and Life in Business Aviation Cabin Ozone Digital Edition Copyright Notice The content contained in this digital edition (“Digital Material”), as well as its selection and arrangement, is owned by Informa. and its affiliated companies, licensors, and suppliers, and is protected by their respective copyright, trademark and other proprietary rights. Upon payment of the subscription price, if applicable, you are hereby authorized to view, download, copy, and print Digital Material solely for your own personal, non-commercial use, provided that by doing any of the foregoing, you acknowledge that (i) you do not and will not acquire any ownership rights of any kind in the Digital Material or any portion thereof, (ii) you must preserve all copyright and other proprietary notices included in any downloaded Digital Material, and (iii) you must comply in all respects with the use restrictions set forth below and in the Informa Privacy Policy and the Informa Terms of Use (the “Use Restrictions”), each of which is hereby incorporated by reference. Any use not in accordance with, and any failure to comply fully with, the Use Restrictions is expressly prohibited by law, and may result in severe civil and criminal penalties. Violators will be prosecuted to the maximum possible extent. You may not modify, publish, license, transmit (including by way of email, facsimile or other electronic means), transfer, sell, reproduce (including by copying or posting on any network computer), create derivative works from, display, store, or in any way exploit, broadcast, disseminate or distribute, in any format or media of any kind, any of the Digital Material, in whole or in part, without the express prior written consent of Informa. -

The BG News August 29, 2006
Bowling Green State University ScholarWorks@BGSU BG News (Student Newspaper) University Publications 8-29-2006 The BG News August 29, 2006 Bowling Green State University Follow this and additional works at: https://scholarworks.bgsu.edu/bg-news Recommended Citation Bowling Green State University, "The BG News August 29, 2006" (2006). BG News (Student Newspaper). 7626. https://scholarworks.bgsu.edu/bg-news/7626 This work is licensed under a Creative Commons Attribution-Noncommercial-No Derivative Works 4.0 License. This Article is brought to you for free and open access by the University Publications at ScholarWorks@BGSU. It has been accepted for inclusion in BG News (Student Newspaper) by an authorized administrator of ScholarWorks@BGSU. ESTABLISHED 1920 A daily independent student press serving THE BG NEWS the campus and surrounding community Tuesday Umbrella: Party of two August 29,2006 Volume 101. Issued 1 WWWBGNEWSCOM Tasteless? Or a No record? matter of bad timing? NBC regrets running plane crash skit after Just fine! passengers were killed on a flight in Misdemeanors may be replaced with fines for Kentucky. | Page 9 lesser crimes beginning early next month No. 1 for "24": By Kelly Day Drama wins its Senior Reporter "We like to know first Emmy that everyone is fair, "24" wins Emmy for Students may not have to worry about having a mis- best drama series but being a black demeanor on their criminal after being shutout in record after Sept. 5, when the male in today's soci- the past | Page 9 Civil Infractions Code goes into effect. ety, I know every- There may be a lesser pun- ishment for crimes like public thing is not fair." urination, said City Prosecutor Matt Reger, at last night's Bernard Little | USG President Undergraduate Student Government meeting "Whether we like it or not, The city Civil Infractions discrimination happens," Code, which was passed last Little said. -

Tesis Doctoral
(28-02-90) TESIS DOCTORAL TRADUCIENDO LA MIRADA: SOBRE LA PRÁCTICA DEL MONTAJE CINEMATOGRÁFICO EN LOS REMAKES NORTEAMERICANOS DE LOS PELÍCULAS DE TERROR ió Rgtre. Fund. Generalitat de Catalunya núm. 472 núm. de Catalunya Fund. Generalitat Rgtre. ió JAPONÉS CONTEMPORÁNEAS Realizada por Sandra Sánchez Lopera En el centro C.I.F. G: 59069740 Universitat Ramon Llull Fundac Llull Ramon 59069740 G: C.I.F. Universitat Universitat Ramon Llull. Facultat de Comunicació i Relacions Internacionals Blanquerna Doctorat en Comunicació Dirigida por Fernando de Felipe Allué 1 SUMARIO INTRODUCCIÓN………………………………………………………………………………………………………… 7 PARTE I: EL CINE DE TERROR JAPONÉS 1. El problema de la clasificación de géneros …..……………….…………………………………… 12 1.1. 1.1. El género como fórmula de producción …..…….………….……………………..…… 12 1.2. 1.2. El género como etiqueta …..…………………………..………………………………………. 15 2. El terror como género cinematográfico ..……………………………………………………………..17 2.1. El reto de los límites y la mezcla de géneros …………...………………………………19 2.2. Diversidad de rasgos dentro del mismo género….……………………………………20 3. El cine de terror japonés como fenómeno internacional (y puntual) ……………………..24 3.1. El terror como género cinematográfico en Japón ……………………………………24 3.1.1. Yotsuya Kaidan, el nacimiento del género de fantasmas en Japón ..…………………………..………………………………………………… 27 3.1.2. Kasane, el fantasma romántico …….………………….……………………… 29 3.1.3. Bakeneko, el gato fantasma …………………..…….…………………….…… 30 3.1.4. Okiku, la chica del pozo, y otras aportaciones al género ….……… 32 3.2. El cine japonés traspasa fronteras ……………..………………………………………… 34 3.3. El terror japonés contemporáneo frente al cine de terror norteamericano .………………….………….…………………………………… 38 3.4. El J-Horror ………………………………………………..………………………………………..… 44 3.4.1. La herencia de Ringu invade el terror made in Hollywood ………..47 PARTE 2: EL REMAKE 1. -
Download PDF of This Issue
chem@cam Chemistry at Cambridge Magazine SPRING 2021 ISSUE 62 www.ch.cam.ac.uk A new name for our Department ______________________________ Major gift secures our future 4 ______________________________ Lockdown eases 6 ______________________________ Women in Chemistry special 20 ______________________________ Contents MAJOR GIFT WOMEN IN CHEMISTRY Reisner group, Professor Sophie Major gift secures the Jackson and Department’s future 4 Fahmida Khan 20 ALUMNI RESEARCH Liquid-liquid phase Themes, teams and separation and the timing 12 origins of life 26 ________________________________________________________ _________________________________________________________ Major gift secures the Department’s future 4 Diversity in Chemistry webinar 19 _________________________________________________________ _________________________________________________________ Lockdown eases 6 Celebrating Women in Chemistry 20-25 _________________________________________________________ _________________________________________________________ Postgrad voices heard 8 Reisner group 20 _________________________________________________________ _________________________________________________________ Alumni correspondence 10 Constant learner 22 _________________________________________________________ _________________________________________________________ Tempus fugit 12 Renaissance woman 24 _________________________________________________________ _________________________________________________________ Alumni postcard 15 Liquid-liquid phase separation 26 -

The BG News September 19, 2011
Bowling Green State University ScholarWorks@BGSU BG News (Student Newspaper) University Publications 9-19-2011 The BG News September 19, 2011 Bowling Green State University Follow this and additional works at: https://scholarworks.bgsu.edu/bg-news Recommended Citation Bowling Green State University, "The BG News September 19, 2011" (2011). BG News (Student Newspaper). 8441. https://scholarworks.bgsu.edu/bg-news/8441 This work is licensed under a Creative Commons Attribution-Noncommercial-No Derivative Works 4.0 License. This Article is brought to you for free and open access by the University Publications at ScholarWorks@BGSU. It has been accepted for inclusion in BG News (Student Newspaper) by an authorized administrator of ScholarWorks@BGSU. Checkout _^ bgnews.com ^ for an exclusive THE BG NEWS video of ESTABLISHED 1920 I An independent student press serving the campus and surrounding community TEDx Volume 91. Issue 14 Monday, September 19 & Tuesday, September 20,2011 www.bgnews.com CAMPUS BRIEF Three members of the alcohol offense and open container June 5. Gates and Lynch's prior offenses are traffic BGSU football team were violations. cited by University police Both Gates and Lynch played in the t>|<8ff*W^ for being in Falcons' 28-27 loss to Wyoming Saturday a residence hall Thursday afternoon "We had a discipline issue, and the one Nicholas McKnight, Darryl Lynch and guy suspended before [McKnight] had a Jerry Gales were each 'issued misdemeanor fairly serious issue in our program before, citations (or criminal trespassing." according said football coach Dave Clawson following to a press release emailed by Dave Meyer, the game. -

'Twas St. Croix Crossing in Costa Mesa!
CHORD-INATOR FEBRUARY 2018 OFFICIAL BULLETIN OF THE MINNEAPOLIS, MINNESOTA, CHAPTER **** A CHAPTER WITH AN ENVIABLE PAST - AN UNBOUNDED FUTURE **** 10,000 LAKES DIVISION - LAND O’LAKES DISTRICT FEBRUARY 2018- VOL.74- NO. 2 ‘twas St. croix crossing in costa mesa! Poise … Polish … Perseverance The Scene: The Segerstrom Center for the Arts Con- ballad, the boys elected to go with two ballads, Smilin’ cert Hall in Costa Mesa, California. The Event: The Bar- Through and Auld Land Syne … and did they perform! bershop Harmony Society’s 2018 International Seniors The audience responded with a rousing ovation, many Quartet Contest. The standing to do so. Time: Late morning Four more quartets of Saturday, January and then the intermi- 20. The third quartet nable waiting and to perform, Easy finally the an- Street, had led off nouncements, 5th with A Chocolate Place, Spotlight, 4th Sundae On a Satur- Place, Renaissance, day Night, conclud- 3rd-Place, Unfin- ing with Always, ished Business, 2nd- both beautifully ren- place, Easy Street … dered in classic Bar- bershop style. Obvi- [Sidebar: Earlier ously the contest bar that morning Judy had then been set at a and I had attended lofty height. the Gold Medal Hour with Main St. Croix Crossing Street where Tony had drawn the 21st Four most happy fellas, St. Croix Crossing, from left: Tenor Randy Lieble, Lead Dan Heike, Bass Jared Hoke, and Baritone Steve Hardy. Staff Photo DeRosa reminisced slot (out of 25) and about some of his had to cool their pipes for three hours or so before taking quartet’s experiences including awaiting the results of the the stage. -

Liza Minnelli Results Mp3, Flac, Wma
Liza Minnelli Results mp3, flac, wma DOWNLOAD LINKS (Clickable) Genre: Electronic Album: Results Country: UK Released: 1989 Style: Synth-pop MP3 version RAR size: 1781 mb FLAC version RAR size: 1495 mb WMA version RAR size: 1180 mb Rating: 4.3 Votes: 916 Other Formats: VQF MP1 VOC AU APE MP2 MMF Tracklist Hide Credits I Want You Now Conductor, Arranged By [Orchestra] – Anne DudleyKeyboards – Pete Vitesse*Percussion – 1 4:41 Danny CummingsProgrammed By [Fairlight Programming] – Chris Lowe, Gary MaughanWritten-By – Tennant / Lowe Losing My Mind Keyboards – Andy Richards, Neil TennantPercussion – Danny CummingsProgrammed By 2 4:11 [Fairlight Programming] – Andy Richards, Chris LoweVocals [Additional] – Neil TennantWritten-By – Stephen Sondheim If There Was Love Keyboards – Chris Lowe, Neil Tennant, Pete Vitesse*Percussion – Danny CummingsPiano – 3 Pete Vitesse*Programmed By [Fairlight Programming] – Chris Lowe, Gary 6:47 MaughanSaxophone – Courtney PineVocals [Additional] – Neil TennantWritten-By – Tennant / LoweWritten-By [Poem] – William Shakespeare So Sorry, I Said 4 Drum Programming [Additional] – C.J. Macintosh*, Julian MendelsohnKeyboards – Neil 3:14 Tennant, Pete Vitesse*Percussion – Danny CummingsWritten-By – Tennant / Lowe Don't Drop Bombs Backing Vocals – Tessa NilesDrum Programming – C.J. Macintosh*Keyboards – Chris Lowe, 5 3:39 Neil Tennant, Pete Vitesse*Scratches – C.J. Macintosh*Vocals [Additional] – Neil TennantWritten-By – Tennant / Lowe Twist In My Sobriety Backing Vocals – Carol Kenyon, Katie Kasson*, Tessa NilesKeyboards – Chris Lowe, Julian Mendelsohn, Neil Tennant, Pete Vitesse*Programmed By [Fairlight Programming] – Chris 6 4:51 Lowe, Gary MaughanRap – Donald JohnsonScratches – C.J. Macintosh*Vocals [Additional] – Julian MendelsohnWritten-By – Tanita TikaramWritten-By [Liza With A Z] – J. Kander - F. Ebb* Rent 7 Arranged By [Orchestra] – Angelo Badalementi*Conductor – Anne DudleyKeyboards 3:54 [Fairlight] – Gary MaughanWritten-By – Tennant / Lowe Love Pains Backing Vocals – Carol Kenyon, Katie Kasson*, Tessa NilesGuitar – J.J. -

The BG News August 30, 2001
Bowling Green State University ScholarWorks@BGSU BG News (Student Newspaper) University Publications 8-30-2001 The BG News August 30, 2001 Bowling Green State University Follow this and additional works at: https://scholarworks.bgsu.edu/bg-news Recommended Citation Bowling Green State University, "The BG News August 30, 2001" (2001). BG News (Student Newspaper). 6826. https://scholarworks.bgsu.edu/bg-news/6826 This work is licensed under a Creative Commons Attribution-Noncommercial-No Derivative Works 4.0 License. This Article is brought to you for free and open access by the University Publications at ScholarWorks@BGSU. It has been accepted for inclusion in BG News (Student Newspaper) by an authorized administrator of ScholarWorks@BGSU. m M M Bowling Green State University THURSDAY August 30, 2001 WOMEN'S SOCCER: ^^^ % ' i 1/ 1/ I 1 PARTLY CLOUDY Andy Richards led the VL I I J W 1 L HIGH: 86 I LOW: 61 team to their first chain- I I ^ L. 1 _M__^ W ■ PV_V VOLUME 92 ISSUE 4 pionship; PAGE 6 1^1 A daily independent student press MM ^M www.bgnews.com Language (JRKKK LIFE dept. Fraternities, sororities celebrates pitch greek life on steps by lake Wasmjer Erin Fox, the adviser for the for the 2000-2001 academic THE BC NEWS Greek Affairs Marketing school year on display. 40 years The first Greek Carnival at the Committee and house director "Academics come first in our University was held yesterday or. for Kappa Delta. "Students don't fraternity," said Michael Sedlak, byYukaNapira the steps of Saddlemire Student have to make a commitment in director of scholarship for Alpha THE BC DEWS Services Building. -

Slap Magazine Issue 95 (September 2019)
Issue 95 Sep2019 FREE SLAP Supporting Local Arts & Performers WORCESTER’S NEW INDEPENDENT ITALIAN RESTAURANT Traditional Italian food, cooked the Italian way! We create all dishes in our kitchen, using only the finest quality fresh ingredients. f. t. i. SUGO at The Lamb & Flag SUGO at Friar St 30 The Tything 19-21 Friar Street, Worcester Worcester WR1 1JL WR1 2NA 01905 729415 01905 612211 [email protected] [email protected] Hello! How was August for you? Worn out yet? Well don’t relax to soon, the summer isn’t quite over yet... In this issue we take you back to a few of last months local festival highlights from Gloucester Blues, the Worcester Show, Lakefest, and Old Bush Blues. They may have suffered with inclement weather but it didn’t dampen the enthusiasm of the sell out crowds. We look forward to the month ahead with Bromyard Folk festival and if it’s something very different you’re looking for, check out Sep 2019 Cheltenham Paint Festival to which our front cover image alludes. Get along to this fabulous free outdoor gallery. Walk around and enjoy the incredible selection on display. And now down to business... With just a few acts still to confirm SLAP MAGAZINE the Worcester Music Festival is shaping up to be the best yet! Make sure you keep the 13th-15th of this month free, pick up a Unit 3a, Lowesmoor Wharf, festival guide and plan your weekend. Don’t forget to pop in to the Worcester WR1 2RS SLAP night at the Marrs Bar on the 14th where we have our usual Telephone: 01905 26660 eclectic mix of groovy indie, psychedelic rock, grunge punk and [email protected] quirky dance to whet the appetite, all with the wonderful Vinny Peculiar to chaperon us through the evening. -
The Malady Lingers On: the Abject and Contemporary Asian Horror Cinema. by Daniel Stephen Hey Submitted in Partial Fulfilment Of
The Malady Lingers On: The Abject and Contemporary Asian Horror Cinema. by Daniel Stephen Hey Submitted in partial fulfilment of the requirements for the degree of Doctor of Philosophy University of Salford School of Arts and Media 2018 Table of Contents List of Figures ........................................................................................................................ v Acknowledgements ............................................................................................................. vii Abstract .............................................................................................................................. viii Section 1: Introduction, Literature Reviews, Methodology .................................................. 1 Chapter I: Introduction .......................................................................................................... 2 1.1 Starting Point ............................................................................................................... 2 1.2 Kristeva: Philosophy, Politics, Post-structuralism, Psychoanalysis ............................ 3 1.3 Brief Introduction to Contemporary Asian Horror Cinema ........................................ 5 1.4 Combining the Two Elements: A Dialogue of Film and Theory ................................ 6 1.5 Structure of the Thesis ................................................................................................. 7 Chapter II: Julia Kristeva and the Abject .............................................................................