A New Telestroke Network System in Northern Area of Okayama Prefecture
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Recovering from Heavy Rain Damage Through Cooperation and Think-And
Our Starting Point Our Starting Point Strategy of Value Creation for Our Vision A Foundation Supporting Value Creation Data Status of operations and damage directly after the Heavy Rain Event of July 2018 Situation at 2:00pm, July 11, 2018 Recovering from heavy rain Operational Operations suspended Shinji Tottori Yonago Higashi- Kisuki Line Maizuru damage through cooperation San-in Line Nishi-Maizuru Izumo-Yokota Chizu Mochigase Kamiiwami Fukuchiyama ru Wadayama Hakubi Line Niimi Tsuyama Express Chizu Maizu Line Bingo-Ochiai Imbi Teramae Masuda Line Ayabe Higashi- San-in Line Hiroshima Bichu- Shiomachi Okayama ama Hagi Shin-Iwakuni Kojiro Tsuy Line Tokuyama ntan Line Aki- Kozuki Sayo Ba and think-and-act initiatives ine akubi Line Kameyama Fuchu H Geibi Line Higashi- Kishin Fukuen Line Line San-yō L Kannnabe Okayama Kamigori Kabe Soja Line Higashihiroshima Himeji Mihara Fukuyama The Heavy Rain Event of July 2018 resulted in large-scale damage throughout West Japan, including in areas where Shin-Yamaguchi Kaitaichi Kushigahama Yokogawa Kasaoka Gantoku Line JR-West operates, and many sections of track were rendered unusable. Iwakuni Kurashiki Kure Line Yanai Amid this unprecedented damage, we came together as a Group and by implementing many think-and-act initiatives and San-yō Line cooperating with local stakeholders, we were able to recover many damaged sections of track and restart operations.* Recovery work In order to get life back to normal as soon as possible, we mobilized Opening land around the capabilities of the entire Group and cooperated with affiliates An entire stations for and local stakeholders in various areas to advance recovery efforts. -

OKAYAMA, KURASHIKI and SETO-OHASHI BRIDGE PAGE 1/ 5
OKAYAMA, KURASHIKI and SETO-OHASHI BRIDGE PAGE 1/ 5 PG-602 OKAYAMA, KURASHIKI and SETO-OHASHI BRIDGE Okayama (岡山) is one of the major commercial, industrial and Kurashiki (倉敷) is an old merchants town near Okayama. In cultural cities in the Chugoku District in western Japan. It is feudal days, it thrived as a port for the shipment of rice; several nationally known for its celebrated Korakuen Garden. It also old rice granaries remain there. Its olden time atmosphere and a serves as a main gateway to Inland Sea National Park and variety of museums lure many visitors to Kurashiki. Shikoku Island. Okayama Airport Bizen- Shin- Soja Ichinomiya bus Kurashiki JR Kibi Line Aioi Kibitsu Okayama JR Shinkansen Line To Hiroshima JR Sanyo Line To Himeji, Kyoto Kurashiki Higashi- bus Okayama Imbe Ako Line Kojima Washuzan Hill Uno bus To Shikoku Is. Access: By Air from Tokyo (Haneda Airport) To Operated by Time required Daily Flights One-way fare Access airport – downtown 35 min. to Okayama Sta. by bus (¥680) ANA 45 min. to Kurashiki Sta. by Airport Okayama Toll free: 0120-029- 1 hr. 20 min. 5 ¥25,500 - ¥27,500 Limousine bus (¥1,000) 222 *Only 4 bus services per day. Please confirm the time table. By Train *Number of flights and fare may change by season. To From Type of Transportation Time required Daily runs One-way fare Okayama Tokyo JR Shinkansen (By Hikari) 3 hrs. 53 min. - 4 hrs. 10 min. 32 ¥16,360 JR Shinkansen (By Nozomi) 3 hrs. 12 min. - 3 hrs. 18 min. -

Miocene Shallow Marine Molluscs from the Hokutan Group in the Tajima Area, Hyôgo Prefecture, Southwest Japan
Bulletin of the Mizunami Fossil Museum, no. 37, p. 51–113, 9 pls., 2 fi gs., 1 table. © 2011, Mizunami Fossil Museum Miocene shallow marine molluscs from the Hokutan Group in the Tajima area, Hyôgo Prefecture, southwest Japan Takashi Matsubara Division of Natural History, Museum of Nature and Human Activities, Hyogo, 6 Yayoigaoka, Sanda 669-1546, Japan <[email protected]> Abstract A taxonomical study of molluscs from the Miocene Hokutan Group was carried out and their paleobiogeographic implication was discussed. A total of 100 species, including 45 species of Gastropoda, 54 species of Bivalvia, and one species of Scaphopoda, were discriminated. The fauna is referred to the Kadonosawa Fauna s.s. on the basis of the occurrences of the intertidal “Arcid-Potamid Fauna” and the upper sublittoral Dosinia-Anadara Assemblage. The upper sublittoral assemblages include Turritella (Turritella) kiiensis Yokoyama, Turritella (Hataiella) yoshidai Kotaka, T. (Kurosioia) neiensis Ida, Ostrea sunakozakaensis (Ogasawara), Cucullaea (Cucullaea) toyamaensis Tsuda, Siphonalia osawanoensis Tsuda, and Varicospira toyamaensis (Tsuda). These species are distributed as far north as the southernmost part of northeast Honshû at that time, and their geographic distributions are identical with the Miocene mangrove swamp element. The occurrences of these species strongly support the previous paleoclimatic reconstruction of the Japanese Islands during the latest Early–earliest Middle Miocene age on the basis of the intertidal molluscan assemblages, and show that central and southwest Honshû was under the warmer marine climate than in northeast Honshû and northwards. All the species including a new cardiid, Parvicardium? mikii sp. nov., are described and/or discussed taxonomically. -

An Analysis of Land-Use in Okayama Prefecture in Terms of Industrial Crops
Journal of the Faculty of Environmental Science and Technology, Okayama University Vol.23, No.1, pp.49-79, March 2018 An Analysis of Land-Use in Okayama Prefecture in terms of Industrial Crops Fumikazu ICHIMINAMI*, 0HOWHP2NXU'ø1ÇSOY** and Enver Erdinç 'ø1ÇSOY*** There are many limitations and difficulties in terms of expanding agricultural lands. Also, some other factors affect the agricultural lands that result in decreases such as climate change, erosion and misuse of the lands. It is clear that these developments in agricultural land use threaten the future of human welfare, social conditions, economic growth and food supply. In this study, we examined the land use and its significance that represent past agriculture and regional characteristics in the Chugoku region including Okayama prefecture and the Seto Inland Sea. Specifically, among the products called as industrial crops, such as cotton, pyrethrum, rush, tobacco, rapeseed, mulberry and tea, were adopted as the indicators. Currently, these landscapes can hardly be seen, only leaves of tobacco and tea can still be seen in mountainous areas. Even in agricultural land use which has almost disappeared now, it may have indirect influence as in the case of reclaimed land and rush products. Therefore, we reaffirmed in this study the reasons for their existence and their significance. Keywords: industrial crop, cultivated area, rural geography, agriculture, Okayama prefecture 1 INTRODUCTION tion not only to the temporal change of the indicator but also the spatial difference. Agriculture is a strategic sector for countries as well as In this research, we restrict the area of Okayama human being in the aspects of basic food supply, raw prefecture and deal with crops other than cereals, vegetables, materials for the industry, and employment. -

Musulim Guid English 1
Okayama Castle - Okayama City ENGLISH Japan Ukankei autumn leaves - Kibichuo Town Homestay experiences - KibichuoTown Hiruzen Sanza mountains in snow - Maniwa City here! WhereOKAYAMA? is Okayama is easily accessible from Tokyo and Osaka! With airplane, Shinkansen, JR train, bus, taxi or rent-a-car, the transportation infrastructure is well-organized and it is a great hub for western Japan. From Japanese Access from all over Japan traditional sightseeing spots to exciting outdoor experiences, you will be 100% satisfied with the attractions in Okayama. It is the perfect destination for your trip to Japan! ■From Hokkaido New Chitose Airport-(airplane)-Okayama Airport-(bus)-Okayama Station 1 hour 50 minutes 30 minutes ■From Tokyo(Haneda Airport) Haneda Airport-(airplane)-Okayama Airport-(bus)-Okayama Station Hokkaido 1 hour 5 minutes 30 minutes By airplane (New Chitose Airport) By Shinkansen 1 hour 50 minutes ■From Tokyo(Narita Airport) Narita Haneda Okayama Airport-(bus)-Airport-(airplane)-Airport-(bus)-Okayama Station Okayama 1 hour 10 minutes 1 hour 5 minutes 30 minutes Hiroshima Hakata Kyoto Nagoya ■From Tokyo Station Tokyo Station-(Shinkansen)-Okayama Station 3 hours 20 minutes Kansai Shin-Osaka International Okayama Airport ■From Yokohama Tokyo(Haneda Airport) 1 hour 5 minutes Shin-Yokohama Station-(Shinkansen)-Okayama Station 3 hours Kansai International Airport ■From Nagoya 1 hour 40 minutes ■From Kyoto 1 hour ■From Nagoya *Take bus for 30 minutes *Take Haruka Express (52 minutes) from Okayama Airport to ■From Shin-Osaka 45 minutes -
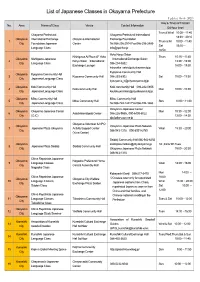
List of Japanese Classes in Okayama Prefecture (Updated March 2021) Day & Times of Classes No
List of Japanese Classes in Okayama Prefecture (Updated March 2021) Day & Times of Classes No. Area Name of Class Venue Contact Information (24-hour time) Tues & Wed 10:00~11:40 Okayama Prefectural Okayama Prefectural International 18:30~20:10 Okayama International Exchange Okayama International Exchange Foundation 1 Thurs & Fri 10:00~11:40 City Foundation Japanese Center Tel:086-256-2914 Fax:086-256-2489 Sat 15:10~ Language Class [email protected] 16:50 Yuko Koryu Salon NIshigawa Ai Plaza 4F Yuko Thurs 10:15~11:45 Okayama Nishigawa Japanese (International Exchange Salon) 2 Koryu Salon(International 13:30~15:00 City Language Class 086-234-5882 Exchange Lounge) 18:00~19:30 [email protected] Kyoyama Community Hall Okayama Kyoyama Community Hall 3 Kyoyama Community Hall 086-253-8302 Sat 10:00~11:30 City Japanese Language Class [email protected] Okayama Koki Community Hall Koki community Hall 086-222-0855 4 Koki community Hall Mon 10:00~11:30 City Japanese Language Class [email protected] Okayama Mitsu Community Hall Mitsu Community Hall 5 Mitsu Community Hall Sun 10:00~11:30 City Japanese Language Class Tel:086-724-1441 Fax:086-724-1666 Okayama Japanese Center Okayama Okayama Japanese Center Mon 10:30~12:00 6 Asia International Center 086-226-9555 , 090-6400-6022 City (OJC) 13:00~14:30 [email protected] Okayama Volunteer & NPO Okayama Okayama Japanese Plaza Network 7 Japanese Plaza Okayama Activity Support Center Wed 18:30~20:00 City 086-943-1318 090-8991-6759 (Yu-ai Center) Saidaiji Community -

Seibu Maruyama Co., Ltd
Company name Seibu Maruyama Co., Ltd. 150-2, Teramoto, Kagamino-Cho, Tomata District, Okayama Prefecture 708-0323 Japan Website: http://www.seibumaruyama.co.jp Tel: +81-868-54-3122 Fax: +81-868-54-3343 Email: [email protected] Products and Services Industrial machinery: Developed to make the most of environmentally friendly“water energy,” Our industrial pumps are used for pressure washing. Our pump technology, cultivated over many years, has been highly President valued and used not only in Japan but also in American and European countries. Devices for environmental hygiene: Kosuke Ōhira Our power sprayers are used to deodorize and disinfect livestock sheds (for chickens, pigs and Seibu Maruyama was established in 1986 as a cattle). They are also used in various environmental hygiene fields: for disinfecting Avian (bird) fully owned company of Maruyama Manufactur- influenza viruses, foot-and-mouth disease viruses, and other viruses and germs. A more daily use of ing. We constantly strive to anticipate customers’ the sprayers is cleaning of air conditioners in offices and homes. needs in advance, only to be able to hear from Fire extinguisher recycle (extinguishant recycle): them “We will place the next order, too, with Recycling a fire extinguisher means to take out the powder (extinguishant) from a collected fire you.” Our main products are agricultural extinguisher, then dry, refine and reuse it as if it is new. Up until now, used extinguishant has been pest-control sprayers, pressure cleaners and buried in a landfill site, but Seibu Maruyama recycles it for maintaining environment. We are one of industrial pumps. -

Tourism Inventory of Okayama Prefecture: an Analysis on Main Sightseeing Spots in Terms of the Number of Tourists
Journal of the Faculty of Environmental Science and Technology, Okayama University Vol.22, No.1, pp.1-28, March 2017 Tourism Inventory of Okayama Prefecture: An Analysis on Main Sightseeing Spots in terms of the Number of Tourists Fumikazu ICHIMINAMI*, Meltem Okur 'ø1d62< DQG(QYHU Erdinç 'ø1d62< At the early stage of this paper, Okayama prefecture was analyzed by the author focusing on the tendency of main sightseeing-areas based on the number of tourists for three decades (Ichiminami, 2002). In this study, the main sightseeing spots in Okayama pref. are also examined and the developments are explained in a more detailed and updated perspective by extending over current features and the number of tourists. One of the important reasons in a significant increase in tourists in Okayama is the opening of the highways, the bullet train and cross-linking of the Seto Ohashi Bridge. At the same time, there are some waves in the increase or decrease of the tourist trends appearing from several vital developments such as environmental, climatic, social, economic and spatial. In this regard, research objectives of the study are mainly based on investigating and making a comprehensive study on main sightseeing spots in Okayama pref. to find new tourism values and to provide a tourism inventory of Okayama pref. by means of information, data and clues from the field in/between the tourist destinations such as hotel guests, gardens and castles. Therefore, Okayama pref. has a rich potential of historical and cultural heritage in terms of spatial planning and growth. The important point is that the structural adaptation between historical and cultural assets and the city life should be provided and protected for domestic and foreign tourism as much as creating better futures in health tourism, gastronomy tourism, cultural tourism, belief tourism, congress tourism, thematic tourism and local tourism. -

Discover a Land Deeply Connected to Japanese Mythology Using Only
Mihonoseki Daisen-Oki National Park Miho Shrine Tottori Sand Dunes Conan Airport N rail map Activity 03 T Tottori Yonago Kitaro Airport Day Izumo Enmusubi Airport 7 Tottori Hinomisaki Matsue Station Prefecture Daisen-Oki National Park Area Daisen-Oki National Park Izumo Grand Shrine Activity 10 Explore Setonaikai National Park Area (Izumo Oyashiro) Izumoshi Station Goal Asago Izumo Grand Shrine Day Day Daisen-Oki National Park (Izumo Oyashiro) Area 5 Activity 16 6 National Odashi Station Omori Mt. Sanbe Day Iwami Ginzan 4 Hyogo Mt. Sanbe Parks Silver Mine Tsuyama Prefecture Nishi no Hara By Theme Mt. Sanbe Niimi Okayama Day Prefecture Shimane Prefecture 3 Miyoshi Okayama Momotaro Himeji Airport Masuda Okayama Discover a Land Deeply Connected Hiroshima Prefecture Kurashiki Hagi-Iwami Airport Setonaikai National Park Activity 06 Start to Japanese Mythology Using Only Hiroshima Hiroshima Airport Fukuyama Day Hiroshima Station Onomichi Hagi 2 Genbaku Dome (Atomic Bomb Dome) Takamatsu Yamaguchi Itsukushima Shrine Day Kagawa Prefecture Prefecture Itsukushima Public Transport Mt. Misen (Miyajima) 1 Takamatsu Airport Setonaikai National Park and Daisen-Oki National Park Sample Course Setonaikai National Park and Daisen-Oki National Park Route This itinerary will take you to a number of locations in Setonaikai National Park and Daisen-Oki National Park that are deeply connected with Japan's mythology. Visit multiple locations emanating tales of the gods, Depart from local airport Haneda Airport・Narita Airport (Kansai Airport) Tokyo Station (JR) 135min including World Heritage Site Itsukushima Shrine on Itsukushima (Miyajima), where gods and humankind Kyoto Station Golden Route Excursion 1:10p.m. Kyoto Station (JR) 100min are said to live side-by-side; Izumo Grand Shrine (Izumo Oyashiro), where countless gods congregate; and 2:50p.m. -

COVID-19 in Okayama Prefecture: Looking Back and Looking Forward
Global Health & Medicine. 2021; 3(2):102-106. Global Health & Medicine. 2021; 3(2):102-106. Communication DOI: 10.35772/ghm.2020.01104 COVID-19 in Okayama Prefecture: Looking back and looking forward Hirokazu Tsukahara1,2,*, Tsukasa Higashionna1,3, Mitsuru Tsuge2, Junko Miyamura1, Nobuchika Kusano1,4 1 Division of Infection Control and Prevention, Okayama University Hospital, Okayama, Japan; 2 Department of Pediatrics, Okayama University Hospital, Okayama, Japan; 3 Department of Pharmacy, Okayama University Hospital, Okayama, Japan; 4 Department of Infectious Diseases, Okayama University Hospital, Okayama, Japan. Abstract: In Japan, clinical and experimental studies addressing COVID-19 have been increasing in number since early February 2020, with many case reports being published. Concurrently, many notifications and guidelines have been issued from the government and academic societies. Taking optimal measures at the prefectural level as well as the national level is necessary to prevent the spread of COVID-19. Surveying and analyzing details of the incidences of infected persons in each prefecture is extremely important. This report describes the epidemiological characteristics of COVID-19 observed in Okayama Prefecture, followed by discussion of the direction of public health actions to be taken in the future. We reiterate the crucial importance of reinforcing and maintaining current public health measures, including rapid and detailed compilation of information related to infected persons and their surroundings, appropriate blocking of viral transmission, and early containment of infected persons, to minimize the spread of infection especially during the overlapping epidemic period of influenza in Okayama Prefecture. Keywords: coronavirus disease 2019 (COVID-19), epidemic period of influenza, epidemiological survey, novel coronavirus pneumonia, Okayama University Hospital, public health actions Introduction to the day of onset. -

Summary of Family Membership and Gender by Club MBR0018 As of December, 2009 Club Fam
Summary of Family Membership and Gender by Club MBR0018 as of December, 2009 Club Fam. Unit Fam. Unit Club Ttl. Club Ttl. District Number Club Name HH's 1/2 Dues Females Male TOTAL District 336 B 23851 AKAIWA L C 0 0 0 14 14 District 336 B 23856 BIZEN 0 0 0 30 30 District 336 B 23857 KURASHIKI HIGASHI 0 0 1 24 25 District 336 B 23858 DAISEN 0 0 2 11 13 District 336 B 23861 HINASE 0 0 0 16 16 District 336 B 23864 IBARA 0 0 5 52 57 District 336 B 23876 KASAOKA 1 1 4 32 36 District 336 B 23877 OKAYAMA KIBI 0 0 1 29 30 District 336 B 23884 KOJIMA WASHU 0 0 0 44 44 District 336 B 23886 KONKO 0 0 3 50 53 District 336 B 23887 KOJIMA 1 1 0 56 56 District 336 B 23888 KURASHIKI 1 1 5 44 49 District 336 B 23889 KURAYOSHI 0 0 4 29 33 District 336 B 23890 KURASHIKI MIZUSHIMA 0 0 2 40 42 District 336 B 23891 KURASHIKI CHUO 0 0 4 44 48 District 336 B 23892 KURASHIKI OHJI 0 0 1 28 29 District 336 B 23895 KURAYOSHI UTSUBUKI 0 0 6 42 48 District 336 B 23897 MANIWA L C 0 0 3 23 26 District 336 B 23905 MIMASAKA 0 0 0 17 17 District 336 B 23907 BIZEN MITSUISHI 7 7 7 8 15 District 336 B 23908 MITSU 0 0 0 27 27 District 336 B 23912 NADASAKI 1 1 0 24 24 District 336 B 23918 NIIMI 3 3 0 74 74 District 336 B 23922 OKAYAMA 0 0 0 48 48 District 336 B 23923 OKAYAMA ASAHI 0 0 4 21 25 District 336 B 23924 OKAYAMA HIGASHI 0 0 7 59 66 District 336 B 23925 OKAYAMA HIKARI 0 0 0 43 43 District 336 B 23926 OKAYAMA SOZAN 0 0 0 33 33 District 336 B 23927 OKAYAMA KORAKU 0 0 0 38 38 District 336 B 23928 OKAYAMA NISHI 0 0 5 44 49 District 336 B 23929 OKAYAMA UJO 0 0 2 29 31 District -

Summary of Family Membership and Gender by Club MBR0018 As of May, 2009
Summary of Family Membership and Gender by Club MBR0018 as of May, 2009 Club Fam. Unit Fam. Unit Club Ttl. Club Ttl. District Number Club Name HH's 1/2 Dues Females Male TOTAL District 336 B 23851 AKAIWA L C 0 0 0 20 20 District 336 B 23856 BIZEN 0 0 0 27 27 District 336 B 23857 KURASHIKI HIGASHI 0 0 1 27 28 District 336 B 23858 DAISEN 0 0 2 12 14 District 336 B 23861 HINASE 0 0 0 14 14 District 336 B 23864 IBARA 0 0 5 54 59 District 336 B 23876 KASAOKA 1 1 4 32 36 District 336 B 23877 OKAYAMA KIBI 0 0 1 29 30 District 336 B 23884 KOJIMA WASHU 0 0 0 46 46 District 336 B 23886 KONKO 0 0 3 54 57 District 336 B 23887 KOJIMA 1 1 0 61 61 District 336 B 23888 KURASHIKI 1 1 4 43 47 District 336 B 23889 KURAYOSHI 0 0 3 28 31 District 336 B 23890 KURASHIKI MIZUSHIMA 0 0 2 43 45 District 336 B 23891 KURASHIKI CHUO 0 0 4 46 50 District 336 B 23892 KURASHIKI OHJI 0 0 1 30 31 District 336 B 23895 KURAYOSHI UTSUBUKI 0 0 5 44 49 District 336 B 23896 KURASHIKI TSURUGATA 0 0 0 19 19 District 336 B 23897 MANIWA L C 0 0 2 23 25 District 336 B 23905 MIMASAKA 0 0 0 19 19 District 336 B 23907 BIZEN MITSUISHI 8 7 7 9 16 District 336 B 23908 MITSU 0 0 0 28 28 District 336 B 23912 NADASAKI 1 1 0 24 24 District 336 B 23918 NIIMI 3 3 0 74 74 District 336 B 23922 OKAYAMA 0 0 0 49 49 District 336 B 23923 OKAYAMA ASAHI 0 0 3 25 28 District 336 B 23924 OKAYAMA HIGASHI 0 0 7 58 65 District 336 B 23925 OKAYAMA HIKARI 0 0 0 49 49 District 336 B 23926 OKAYAMA SOZAN 0 0 0 34 34 District 336 B 23927 OKAYAMA KORAKU 0 0 0 45 45 District 336 B 23928 OKAYAMA NISHI 0 0 5 42 47