Clinical UM Guideline Description Clinical Indications
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Research Article Behavior of Elastic Therapeutic Tapes Under Dynamic and Static Conditions
Hindawi Advances in Materials Science and Engineering Volume 2021, Article ID 6671712, 9 pages https://doi.org/10.1155/2021/6671712 Research Article Behavior of Elastic Therapeutic Tapes under Dynamic and Static Conditions Hermela Ejegu ,1 Bipin Kumar ,2 and Priyanka Gupta 2 1Department of Textile Engineering, Dire Dawa Institute of Technology, Dire Dawa, Ethiopia 2Department of Textile Technology, Indian Institute of Technology Delhi, Hauz Khas 110016, New Delhi, India Correspondence should be addressed to Hermela Ejegu; [email protected] Received 13 November 2020; Revised 13 July 2021; Accepted 29 July 2021; Published 10 August 2021 Academic Editor: Ivan Giorgio Copyright © 2021 Hermela Ejegu et al. (is is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited. (e aim of this paper is to determine the relaxation behavior of the therapeutic tape under different thermomechanical conditions over different time spans and to analyze the physical and mechanical properties of selected kinesiology tapes. (e relaxation test was conducted under a static condition with two extended levels (25% and 50%) for one hour and a dynamic condition for 300 cycles with different loading-unloading values, strain rates, and temperatures. For both static and dynamic conditions, at a lower strain rate and higher load and temperature, the therapeutic tapes showed higher loss of internal stress and faster losses of efficiency. Under all selected conditions, the tape’s stress has decreased rapidly. 1. Introduction (e previous study on the Kinesio taping method is devoted to examining its therapeutic effects, or its effect on Elastic therapeutic tape (ET), also known as Kinesio tape, clinical treatment like athletic performance, lymphatic was developed by Japanese Chiropractor Dr. -

The Effect of Elastic Therapeutic Taping on Lumbar Extensor Isokinetic Performance
The effect of elastic therapeutic taping on lumbar extensor isokinetic performance Harry J Knapman1, Tom Fallon1, Matthew O’Connor1, Lee A Titmus1, Sherrie T Choy2, Claire Hornsby1, Jon F Marsden1 and Gary L Shum3 1 School of Health Professions, Plymouth University, United Kingdom 2 Livewell Southwest, NHS, Plymouth, United Kingdom 3 Faculty of Sport & Health Sciences, University of St Mark & St John, United Kingdom Corresponding author: Dr Gary Shum PhD, MCSP Faculty Director of Research & Associate Professor Faculty of Sport & Health Sciences University of St Mark & St John Derriford Road, Plymouth PL6 8BH United Kingdom Email: [email protected] Tel: 01752 636700 (Ext. 5310) 1 The effect of elastic therapeutic taping on lumbar extensor isokinetic performance Abstract Objective: To investigate the effects of elastic therapeutic tape when applied overlaying the lumbar extensors on different measures of muscle performance, compared to a placebo taping technique and a no-tape control. Relevance: Elastic therapeutic tape is frequently used as an adjunct to enhance athletic performance amongst athletes. However, limited research exists supporting its application on isokinetic performance of the lumbar extensor muscles. Methods: A cross-sectional experimental study. 21 participants received three taping conditions in a randomised order: elastic therapeutic tape, a placebo tape and a no- tape control. Peak torque, the time taken to reach peak torque and peak velocity were measured using an isokinetic dynamometer. Analysis: Friedman’s test and post-hoc Wilcoxon signed-rank test were used to determine the statistical differences between the three taping conditions. Level of significance was set at 0.05. Results: A statistically significant improvement in peak lumbar extensor torque was observed when comparing elastic therapeutic tape with the no-tape control (p < 0.05). -

Downloaded for Free from the Chief Editor’S the Involvement of Acupuncture Meridians (As in Website (
JOURNAL OF THE ACUPUNCTURE ASSOCIATION OF CHARTERED PHYSIOTHERAPISTS OF CHARTERED ASSOCIATION ACUPUNCTURE THE JOURNAL OF )5(( 6$03/(6 $9$,/$%/( $'$37$707DSH :LWKHODVWLFLW\VLPLODUWRKXPDQVNLQLWSURYLGHV VXSSRUWZLWKQRPRWLRQUHVWULFWLRQVDQGH[WHQGVWR ([FHOOHQFHDW HQKDQFHWKHUDQJHRIPRWLRQ([FHOOHQWVNLQEUHDWKDELOLW\ DOORZVVZHDWKHDWDQGDLUWRSHQHWUDWHWKHWDSHDQGEH 6HQVLEOH3ULFHV GLVSHUVHG:DWHUUHVLVWDQWDQGHDV\WRGU\ $FXSXQFWXUH1HHGOHV $FXSXQFWXUH1HHGOHV 6XUJLFDOVWDLQOHVVVWHHODQGHDV\ &RORXUFRGHGSODVWLFKDQGOHVIRU JOLGLQJLQVHUWLRQ0DGHLQ6RXWK.RUHD HDV\ JDXJH LGHQWL¿FDWLRQ 5RXQGHG WXEHHQGHQDEOHVFRPIRUWDEOHWDSSLQJ RQ QHHGOHLQVHUWLRQDQGDOVRIRU SDWLHQWFRPIRUW 0R[D 6WLFNRQPR[DVPRNHOHVVDQGRGRXUOHVV &XSSLQJ6HW 9HUVDWLOHVKDSHVDFFRPPRGDWHERG\ Journal of the FRQWRXUV'HWDFKDEOHVLOLFRQHYDOYHV DOORZHDV\FOHDQLQJRUVWHULOLVDWLRQ Acupuncture Association of Chartered Physiotherapists LQIR#DFXSULPHFRP ZZZDFXSULPHFRP Autumn Autumn 2014 )RUUHVW8QLWV+HQQRFN5RDG(DVW 0DUVK%DUWRQ,QGXVWULDO(VWDWH $OHDGLQJEUDQGIURP ([HWHU(;588QLWHG.LQJGRP 2014 ISSN 1748-8656 IRU \HDUV &HOHEUDWLQJ\HDUV RIRXUVWDQGDUG &ODVVLF3OXV DFXSXQFWXUHQHHGOH 6HLULQQHHGOHV (OHFWURWKHUDS\ 6SRUWVWKHUDS\ 3HUPHQDQWO\ 1HZ ORZSULFHV 7KHPRVWSRSXODUQHHGOHVXLWDEOHIRU 3UHPLR/DVHU'XRDQG3UHPLR/DVHU 1HZ UDQJHV RI VSRUWV WKHUDS\ FRVPHWLFDFXSXQFWXUHDQGDYDLODEOHLQ $*3URJUDP SURGXFWVLQFOXGHHOHFWURWKHUDS\ XOWUDVRXQG DQG PDJQHWLF ÀHOG SODVWLFKDQGOHDQGDOOPHWDOKDQGOH 6RIWODVHUIRUSK\VLRWKHUDS\ODVHUWKHUDS\ WKHUDS\ JRRGV 2XU YHU\ RZQ VSRUWVPHGLFLQHDQGORFDODSSOLFDWLRQ NLQHVLRORJ\VSRUWVWDSH&ODVVLF3UR LV DOVR QRZ DYDLODEOH 0R[LEXVWLRQIRU -

Student Research and Creativity Spotlighting the Best of Student Work at 2013 CELEBRATION of STUDENT RESEARCH and CREATIVITY | 1
celebration of student research and creativity Spotlighting the best of student work at 2013 CELEBRATION OF STUDENT RESEARCH AND CREATIVITY | 1 celebration of student research and creativity Spotlighting the best of student work at This publication was prepared by Northern Kentucky University and printed with state funds (KRS 57.375). It is Northern Kentucky University’s policy to ensure equal employment opportunity for all persons and to take the necessary actions needed to recruit, employ, train, promote, and retain qualified faculty and staff, including members of protected groups. Discrimination against any individual based upon protected status, which is defined as age, color, disability, gender, national origin, race, religion, sexual orientation, genetic, or veteran status, is prohibited. 00000 TABLE OF CONTENTS Contents Letter from the President ............................................................................................................................................2 Letter from the Provost ................................................................................................................................................3 Schedule of Events .......................................................................................................................................................4 Celebrate NKU All Around Campus Events ..............................................................................................................5 Artistic Presentations ...................................................................................................................................................6 -

Professional Provider Office Manual
July 2008 Provider Network News 3 Professional Provider Office Manual www.bcbsla.com/providers www.bcbsla.com/ilinkblue 3 News Network Provider 2008 July 23XX6767 R12/16 Blue Cross and Blue Shield of Louisiana is an independent licensee of the Blue Cross and Blue Shield Association and incorporated as Louisiana Health Service & Indemnity Company. Blue Cross and Blue Shield of Louisiana PROFESSIONAL PROVIDER OFFICE MANUAL This manual is designed to provide information you will need as a participant in the Blue Cross and Blue Shield of Louisiana Professional Provider Network—it is an extension of your Professional Provider Agreement. To use your manual, first familiarize yourself with the Network Overview and Definitions sections. From that point on, the Table of Contents should direct you to the information you need. Periodically, we send newsletters and informational notices to providers. Please keep this information and a copy of your respective provider agreement(s) along with your manual for your reference. Updated office manuals and provider newsletters may be found on the Provider page of our website at www.bcbsla.com/ providers. If you have questions about the information in your manual or your participation as a network provider, please call Network Administration at 1-800-716-2299, option 1 or (225) 297-2758. Please Note: This manual contains a general description of Benefits that are available subject to the terms of a Member’s contract and our corporate medical policies. The Member Contract/Certificate contains information on Benefits, limitations and exclusions and managed care benefit requirements. It also may limit the number of days, visits or dollar amounts to be reimbursed. -

Effect of Kinesio Taping on the Walking Ability of Patients with Foot Drop After Stroke
Hindawi Evidence-Based Complementary and Alternative Medicine Volume 2019, Article ID 2459852, 7 pages https://doi.org/10.1155/2019/2459852 Research Article Effect of Kinesio Taping on the Walking Ability of Patients with Foot Drop after Stroke Yilan Sheng,1,2 Shifeng Kan,2,3 Zixing Wen,2 Wenhua Chen,1,2 Qi Qi,4 Qiang Qu,2 and Bo Yu 1,2 Department of Rehabilitation, Shanghai General Hospital, Shanghai Jiao Tong University, No. , Haining Road, Shanghai , China Department of Rehabilitation, School of International Medical Technology, Sanda University, No. , Jinhai Road, Shanghai , China Department of Rehabilitation, Shanghai Fi h Rehabilitation Hospital, No. , Ledu Road, Shanghai , China Department of Rehabilitation, Shanghai Sunshine Rehabilitation Center, Yangzhi Affiliated Hospital of Tongji University, No. , Guangxing Road, Shanghai , China Correspondence should be addressed to Bo Yu; [email protected] Received 15 February 2019; Accepted 15 April 2019; Published 15 May 2019 Academic Editor: Manel Santafe Copyright © 2019 Yilan Sheng et al. Tis is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited. Objective. Te purpose of this study was to investigate the efect of kinesio taping on the walking ability in patients with foot drop afer stroke. Methods. Sixty patients were randomly divided into the experimental group (with kinesio taping) and the control group (without kinesio taping). Te 10-Meter Walking Test (10MWT), Timed Up and Go Test (TUGT), stride length, stance phase, swing phase, and foot rotation of the involved side were measured with the German ZEBRIS gait running platform analysis system and were used to evaluate and compare the immediate efects of kinesio taping. -

“Kinesiology” Taping?
3/20/2019 Presenter: Deepesh Dani PT, DPT, MS, CKTI Physical Therapist & Advanced Credentialed Clinical Instructor Presenter: Deepesh Dani PT, DPT, MS, CKTI Physical Therapist & Advanced Credentialed Clinical Instructor Disclaimer: I am a certified instructor for the Kinesio Taping® Association International (KTAI) and act as an independent contractor teaching courses in the KTAI program. Although I receive compensation for KTAI teaching assignments, I offer this workshop as a pro bono educational outreach. What is Elastic Therapeutic Taping or “Kinesiology” Taping? Used during rehabilitative and chronic phases of injury – Acute – Sub acute – Rehabilitative Preventative Return body to Homeostasis Presenter: Deepesh Dani PT, DPT, MS, CKTI Physical Therapist & Advanced Credentialed Clinical Instructor © All images and text are copyrighted and private property 1 3/20/2019 What is Elastic Therapeutic Taping or “Kinesiology” Taping? © All images and text are copyrighted and private property Taping Benefits Integrate Kinesiology Taping to enhance and prolong the benefits of treatment for: • Overworked Muscles & Joints • Headaches • Achilles Tendonitis • Hallux Valgus • Frozen Shoulder • Brachial Plexus Syndrome • Whiplash • Chronic Neck and back Discomfort • Discomfort from Arthritis • Edema… and Much More! © All images and text are copyrighted and private property Five Major physiological effects of Kinesiology Taping 1. Skin 2. Circulatory/Lymphatic Systems 3. Fascia 4. Muscle 5. Joint © All images and text are copyrighted and private property -

Sports & Athletes
YOUR PRACTICE PARTNER Issue 12: July 30, 2019 chiroeco.com SPORTS & ATHLETES Keeping pros and weekend warriors on their games U.S. national Orthotics and The water-soluble soccer’s DC MLB players CBD difference It’s about time. Time spent enjoying life’s little moments. Introducing Olprima™ Three new concentrated omega-3 oils that support the unique needs of your patients, from cardiovascular^ to brain health.* Rigorously Sustainably Tested Sourced Pure Find out more at standardprocess.com/ce-olprimas We focus on achieving wholistic health through nutrition. From our organic, *These statements have not been evaluated by the Food and Drug Administration. These products are not intended to diagnose, treat, cure, or prevent any disease. regenerative farming practices to our Nutrition Innovation Center, we are ^As part of a diet low in saturated fat and cholesterol. ©2019 Standard Process Inc. All rights reserved. LN00067 04/19 committed to clinical science that advances health and changes lives. LN00067 Olprimas Chiro Econ Spread.indd 1 5/2/19 4:04 PM It’s about time. Time spent enjoying life’s little moments. Introducing Olprima™ Three new concentrated omega-3 oils that support the unique needs of your patients, from cardiovascular^ to brain health.* Rigorously Sustainably Tested Sourced Pure Find out more at standardprocess.com/ce-olprimas We focus on achieving wholistic health through nutrition. From our organic, *These statements have not been evaluated by the Food and Drug Administration. These products are not intended to diagnose, treat, cure, or prevent any disease. regenerative farming practices to our Nutrition Innovation Center, we are ^As part of a diet low in saturated fat and cholesterol. -

What's Inside
Complimentary http://www.deserthealthnews.com/ May/June 2014 what’s inside Medical News 3 May is Stroke Awareness Month Terry Wahls, MD, is an Assistant Chief of Staff at Iowa lacking in those with autoimmune diseases such as MS. City VA Health Care and clinical professor of medicine at She added electrical stimulation therapy (e-stim) after the University of Iowa. She has practiced medicine for researching this protocol as used on paralysis due to over 30 years and is board-certified in internal medicine. acute spinal injury, and eliminated Like most physicians, Dr. Wahls toxins from her environment. Natural Options treated her patients’ ailments with Her decline slowed, and in 11 drugs and surgical procedures, November of 2007, her online Gluten-Free with Tiffany until she herself was diagnosed research led her to the Institute for with primary progressive multiple Functional Medicine. Functional sclerosis in 2000, and conventional medicine differs from mainstream medicine began to fail her. medicine in its willingness to employ Even though she was working treatments which may not be well Integrated Practices with top specialists in the field at evidenced by clinical research.1 Its goal 15 the Cleveland Clinic and had tried is to provide clinicians with a better numerous medications, by 2007 way to care for people with complex Is Testosterone Therapy she was confined to a recliner or chronic disease by looking at the in Men Harmful? bed and could walk only a few interaction between genetics, diet, steps with two canes. hormone balance, toxin exposure, As a decorated athlete in her infections and psychological factors youth, Dr. -
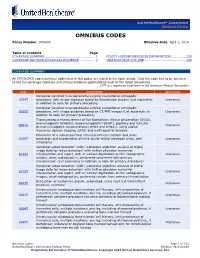
OMNIBUS CODES Policy Number: OTH037 Effective Date: April 1, 2019
UnitedHealthcare® Commercial Medical Policy OMNIBUS CODES Policy Number: OTH037 Effective Date: April 1, 2019 Table of Contents Page COVERAGE SUMMARY............................................... 1 POLICY HISTORY/REVISION INFORMATION .............. 122 COVERAGE RATIONALE/CLINICAL EVIDENCE ............... 7 INSTRUCTIONS FOR USE ....................................... 122 COVERAGE SUMMARY All CPT/HCPCS codes/services addressed in this policy are noted in the table below. Click the code link to be directed to the full coverage rationale and clinical evidence applicable to each of the listed procedures. CPT® is a registered trademark of the American Medical Association Code Description Conclusion Computer-assisted musculoskeletal surgical navigational orthopedic 0054T procedure, with image-guidance based on fluoroscopic images (List separately Unproven in addition to code for primary procedure) Computer-assisted musculoskeletal surgical navigational orthopedic 0055T procedure, with image-guidance based on CT/MRI images (List separately in Unproven addition to code for primary procedure) Transcutaneous measurement of five biomarkers (tissue oxygenation [StO2], oxyhemoglobin [ctHbO2], deoxyhemoglobin [ctHbR], papillary and reticular 0061U Unproven dermal hemoglobin concentrations [ctHb1 and ctHb2]), using spatial frequency domain imaging (SFDI) and multi-spectral analysis Placement of a subconjunctival retinal prosthesis receiver and pulse 0100T generator, and implantation of intra-ocular retinal electrode array, with Unproven vitrectomy Computer-aided -

Omnibus Codes – Commercial Medical Policy
UnitedHealthcare® Commercial Medical Policy Omnibus Codes Policy Number: 2021T0535III Effective Date: May 1, 2021 Instructions for Use Table of Contents Page Community Plan Policy Coverage Summary........................................................................... 1 • Omnibus Codes Coverage Rationale/Clinical Evidence .........................................12 Policy History/Revision Information........................................... 171 Instructions for Use ...................................................................... 174 Coverage Summary All CPT/HCPCS codes/services addressed in this policy are noted in the table below. Click the code link to be directed to the full coverage rationale and clinical evidence applicable to each of the listed procedures. CPT® is a registered trademark of the American Medical Association Code Description Conclusion 0042T Cerebral perfusion analysis using computed tomography with contrast Proven in certain administration, including post-processing of parametric maps with circumstances determination of cerebral blood flow, cerebral blood volume, and mean transit time 0061U Transcutaneous measurement of five biomarkers (tissue oxygenation [StO2], Unproven oxyhemoglobin [ctHbO2], deoxyhemoglobin [ctHbR], papillary and reticular dermal hemoglobin concentrations [ctHb1 and ctHb2]), using spatial frequency domain imaging (SFDI) and multi-spectral analysis 0100T Placement of a subconjunctival retinal prosthesis receiver and pulse Unproven generator, and implantation of intra-ocular retinal -

Adhesion of Three Brands of Elastic Therapeutic Tape Robert Topp University of San Diego
View metadata, citation and similar papers at core.ac.uk brought to you by CORE provided by University of San Diego University of San Diego Digital USD Nursing and Health Science Faculty Publications Hahn School of Nursing and Health Science 2017 Adhesion of Three Brands of Elastic Therapeutic Tape Robert Topp University of San Diego Jena L. Slaski Sport and Spine Rehab Clinical Research Foundation Barton N. Bishop Sport and Spine Rehab Clinical Research Foundation Phil Page Performance Health Follow this and additional works at: http://digital.sandiego.edu/nursing_facpub Part of the Nursing Commons Digital USD Citation Topp, Robert; Slaski, Jena L.; Bishop, Barton N.; and Page, Phil, "Adhesion of Three Brands of Elastic Therapeutic Tape" (2017). Nursing and Health Science Faculty Publications. 18. http://digital.sandiego.edu/nursing_facpub/18 This Article is brought to you for free and open access by the Hahn School of Nursing and Health Science at Digital USD. It has been accepted for inclusion in Nursing and Health Science Faculty Publications by an authorized administrator of Digital USD. For more information, please contact [email protected]. Journal of Performance Health Research Original Research Volume 1, Issue 2. Pages 16–22 DOI: 10.25036/jphr.2017.1.2.topp OPEN ACCESS © 2017 Performance Health www.performancehealthresearch.com ISSN 2573-5136 OBSERVATIONAL COHORT Adhesion of Three Brands of Elastic Therapeutic Tape Robert Topp,1* Jena L. Slaski,2 Barton N. Bishop,2 and Phil Page3 Purpose: The purpose of this study was to compare, over a period of 5 days, the rate of adhesion of TheraBand® Kinesiology Tape (TKT) with either KT Tape® (KT) or Kinesio® Tex Gold (KTEX) under 25% elongation among healthy adults.