Acne Vulgaris, II: Treatment
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Herb Lotions to Regrow Hair in Patients with Intractable Alopecia Areata Hideo Nakayama*, Ko-Ron Chen Meguro Chen Dermatology Clinic, Tokyo, Japan
Clinical and Medical Investigations Research Article ISSN: 2398-5763 Herb lotions to regrow hair in patients with intractable alopecia areata Hideo Nakayama*, Ko-Ron Chen Meguro Chen Dermatology Clinic, Tokyo, Japan Abstract The history of herbal medicine in China goes back more than 1,000 years. Many kinds of mixtures of herbs that are effective to diseases or symptoms have been transmitted from the middle ages to today under names such as Traditional Chinese Medicine (TCM) in China and Kampo in Japan. For the treatment of severe and intractable alopecia areata, such as alopecia universalis, totalis, diffusa etc., herb lotions are known to be effective in hair regrowth. Laiso®, Fukisin® in Japan and 101® in China are such effective examples. As to treat such cases, systemic usage of corticosteroid hormones are surely effective, however, considering their side effects, long term usage should be refrained. There are also these who should refrain such as small children, and patients with peptic ulcers, chronic infections and osteoporosis. AL-8 and AL-4 were the prescriptions removing herbs which are not allowed in Japanese Pharmacological regulations from 101, and salvia miltiorrhiza radix (SMR) is the most effective herb for hair growth, also the causation to produce contact sensitization. Therefore, the mechanism of hair growth of these herb lotions in which the rate of effectiveness was in average 64.8% on 54 severe intractable cases of alopecia areata, was very similar to DNCB and SADBE. The most recommended way of developing herb lotion with high ability of hairgrowth is to use SMR but its concentration should not exceed 2%, and when sensitization occurs, the lotion should be changed to Laiso® or Fukisin®, which do not contain SMR. -

Acne in Childhood: an Update Wendy Kim, DO; and Anthony J
FEATURE Acne in Childhood: An Update Wendy Kim, DO; and Anthony J. Mancini, MD cne is the most common chron- ic skin disease affecting chil- A dren and adolescents, with an 85% prevalence rate among those aged 12 to 24 years.1 However, recent data suggest a younger age of onset is com- mon and that teenagers only comprise 36.5% of patients with acne.2,3 This ar- ticle provides an overview of acne, its pathophysiology, and contemporary classification; reviews treatment op- tions; and reviews recently published algorithms for treating acne of differing levels of severity. Acne can be classified based on le- sion type (morphology) and the age All images courtesy of Anthony J. Mancini, MD. group affected.4 The contemporary Figure 1. Comedonal acne. This patient has numerous closed comedones (ie, “whiteheads”). classification of acne based on sev- eral recent reviews is addressed below. Acne lesions (see Table 1, page 419) can be divided into noninflammatory lesions (open and closed comedones, see Figure 1) and inflammatory lesions (papules, pustules, and nodules, see Figure 2). The comedone begins with Wendy Kim, DO, is Assistant Professor of In- ternal Medicine and Pediatrics, Division of Der- matology, Loyola University Medical Center, Chicago. Anthony J. Mancini, MD, is Professor of Pediatrics and Dermatology, Northwestern University Feinberg School of Medicine, Ann and Robert H. Lurie Children’s Hospital of Chi- cago. Address correspondence to: Anthony J. Man- Figure 2. Moderate mixed acne. In this patient, a combination of closed comedones, inflammatory pap- ules, and pustules can be seen. cini, MD, Division of Dermatology Box #107, Ann and Robert H. -

Table S1. Checklist for Documentation of Google Trends Research
Table S1. Checklist for Documentation of Google Trends research. Modified from Nuti et al. Section/Topic Checklist item Search Variables Access Date 11 February 2021 Time Period From January 2004 to 31 December 2019. Query Category All query categories were used Region Worldwide Countries with Low Search Excluded Volume Search Input Non-adjusted „Abrasion”, „Blister”, „Cafe au lait spots”, „Cellulite”, „Comedo”, „Dandruff”, „Eczema”, „Erythema”, „Eschar”, „Freckle”, „Hair loss”, „Hair loss pattern”, „Hiperpigmentation”, „Hives”, „Itch”, „Liver spots”, „Melanocytic nevus”, „Melasma”, „Nevus”, „Nodule”, „Papilloma”, „Papule”, „Perspiration”, „Petechia”, „Pustule”, „Scar”, „Skin fissure”, „Skin rash”, „Skin tag”, „Skin ulcer”, „Stretch marks”, „Telangiectasia”, „Vesicle”, „Wart”, „Xeroderma” Adjusted Topics: "Scar" + „Abrasion” / „Blister” / „Cafe au lait spots” / „Cellulite” / „Comedo” / „Dandruff” / „Eczema” / „Erythema” / „Eschar” / „Freckle” / „Hair loss” / „Hair loss pattern” / „Hiperpigmentation” / „Hives” / „Itch” / „Liver spots” / „Melanocytic nevus” / „Melasma” / „Nevus” / „Nodule” / „Papilloma” / „Papule” / „Perspiration” / „Petechia” / „Pustule” / „Skin fissure” / „Skin rash” / „Skin tag” / „Skin ulcer” / „Stretch marks” / „Telangiectasia” / „Vesicle” / „Wart” / „Xeroderma” Rationale for Search Strategy For Search Input The searched topics are related to dermatologic complaints. Because Google Trends enables to compare only five inputs at once we compared relative search volume of all topics with topic „Scar” (adjusted data). Therefore, -

Acne and Rosacea in Skin of Color Heather Woolery-Lloyd, MD; Erica Good, BA
Editorial Acne and Rosacea in Skin of Color Heather Woolery-Lloyd, MD; Erica Good, BA reatment of acne in skin of color poses unique of ethnicities, including African Americans, Asians, challenges. Postinflammatory hyperpigmentation Hispanics/Latinos, Pacific Islanders, Middle Easterners, T is a common complaint and must be addressed in and Native Americans, patients with skin of color cur- this patient population. Although less common in skin rently represent 34% of the US population. As it is of color, rosacea can often be more severe in this patient estimated that this figure will rise to 47% by 2050, it is population. We will review acne and rosacea in patients important to have a thorough understanding of how acne with skin of color and will focus on management of the presents in this patient population in order to optimize concerns unique to this patient population. their treatment.3 Regardless of skin color, acne remains the most com- monly diagnosed dermatologic condition. Studies have Clinical Characteristics reported an overall incidence as high as 29% in black Papules are the most frequent presentation of acne in patients, with similar figures for white patients in com- skin of color, occurring in 70.7% of African American parative studies.1 In adult women alone, the prevalence patients and 74.5% of Hispanics/Latinos. Acne hyperpig- may exceedCOS 50%.2 DERMmented maculae are also a common presenting feature, Postinflammatory hyperpigmentation presents a occurring in 65% of African Americans and in 48% of unique but common challenge when treating acne in skin Hispanic/Latino women with acne, according to a recent of color, and can often become a greater source of distress study (Figure 1).4,5 Among African Americans, other com- to the patient than the acne itself. -
Acne and Related Conditions
Rosanne Paul, DO Madeline Tarrillion, DO Miesha Merati, DO Gregory Delost, DO Emily Shelley, DO Jenifer R. Lloyd, DO, FAAD American Osteopathic College of Dermatology Disclosures • We do not have any relevant disclosures. Cleveland before June 2016 Cleveland after June 2016 Overview • Acne Vulgaris • Folliculitis & other – Pathogenesis follicular disorders – Clinical Features • Variants – Treatments • Rosacea – Pathogenesis – Classification & clinical features • Rosacea-like disorders – Treatment Acne vulgaris • Pathogenesis • Multifactorial • Genetics – role remains uncertain • Sebum – hormonal stimulation • Comedo • Inflammatory response • Propionibacterium acnes • Hormonal influences • Diet Bolognia et al. Dermatology. 2012. Acne vulgaris • Clinical Features • Face & upper trunk • Non-inflammatory lesions • Open & closed comedones • Inflammatory lesions • Pustules, nodules & cysts • Post-inflammatory hyperpigmentation • Scarring • Pitted or hypertrophic Bolognia et al. Dermatology. 2012. Bolognia et al. Dermatology. 2012. Acne variants • Acne fulminans • Acne conglobata • PAPA syndrome • Solid facial edema • Acne mechanica • Acne excoriée • Drug-induced Bolognia et al. Dermatology. 2012. Bolognia et al. Dermatology. 2012. Bolognia et al. Dermatology. 2012. Bolognia et al. Dermatology. 2012. Acne variants • Occupational • Chloracne • Neonatal acne (neonatal cephalic pustulosis) • Infantile acne • Endocrinological abnormalities • Apert syndrome Bolognia et al. Dermatology. 2012. Bolognia et al. Dermatology. 2012. Acne variants • Acneiform -

Acneiform Dermatoses
Dermatology 1998;196:102–107 G. Plewig T. Jansen Acneiform Dermatoses Department of Dermatology, Ludwig Maximilians University of Munich, Germany Key Words Abstract Acneiform dermatoses Acneiform dermatoses are follicular eruptions. The initial lesion is inflamma- Drug-induced acne tory, usually a papule or pustule. Comedones are later secondary lesions, a Bodybuilding acne sequel to encapsulation and healing of the primary abscess. The earliest histo- Gram-negative folliculitis logical event is spongiosis, followed by a break in the follicular epithelium. The Acne necrotica spilled follicular contents provokes a nonspecific lymphocytic and neutrophilic Acne aestivalis infiltrate. Acneiform eruptions are almost always drug induced. Important clues are sudden onset within days, widespread involvement, unusual locations (fore- arm, buttocks), occurrence beyond acne age, monomorphous lesions, sometimes signs of systemic drug toxicity with fever and malaise, clearing of inflammatory lesions after the drug is stopped, sometimes leaving secondary comedones. Other cutaneous eruptions that may superficially resemble acne vulgaris but that are not thought to be related to it etiologically are due to infection (e.g. gram- negative folliculitis) or unknown causes (e.g. acne necrotica or acne aestivalis). oooooooooooooooooooo Introduction matory (acne medicamentosa) [1]. The diagnosis of an ac- neiform eruption should be considered if the lesions are The term ‘acneiform’ refers to conditions which super- seen in an unusual localization for acne, e.g. involvement of ficially resemble acne vulgaris but are not thought to be re- distal parts of the extremities (table 1). In contrast to acne lated to it etiologically. vulgaris, which always begins with faulty keratinization Acneiform eruptions are follicular reactions beginning in the infundibula (microcomedones), comedones are usu- with an inflammatory lesion, usually a papule or pustule. -

Hidradenitis Suppurativa (Acne Inversa): Management of a Recalcitrant Disease
STATE-OF-THE-ART REVIEW Editor: Bernard A. Cohen, M.D. Pediatric Dermatology Vol. 24 No. 5 465–473, 2007 Hidradenitis Suppurativa (Acne inversa): Management of a Recalcitrant Disease Joseph Lam, M.D.,* Andrew C. Krakowski, M.D.,* and Sheila F. Friedlander, M.D. *Rady Children’s Hospital, University of California, Departments of Pediatrics and Medicine (Dermatology), San Diego School of Medicine, University of California, San Diego, California Abstract: Hidradenitis suppurativa is a chronic relapsing disorder of follicular occlusion that is often recalcitrant to therapy. Topical and systemic antibiotics, hormonal therapies, oral retinoids, immunosuppressant agents, and surgical treatment are some of the therapeutic alternatives used for this often recalcitrant and frequently troublesome disorder. This article reviews the pathophysiology of hidradenitis suppurativa, an evidence-based analy- sis of standard treatments, and recent advances in the therapy of this disorder. Hidradenitis suppurativa (HS) is a disease of the (2,3), with the inflammation of apocrine glands that oc- apocrine gland-bearing areas of the body that commonly curs likely representing a secondary phenomenon affects the intertriginous areas. Although it may initially resulting from follicular plugging (3). It is now believed present in a mild form, recurrent abscesses with the that HS is primarily an inflammatory disorder of the hair development of sinus tracts and scarring generally en- follicle and, therefore, is included in the follicular occlu- sues. Rather than a distinct disease entity, it may repre- sion tetrad along with acne conglobata, dissecting cellu- sent the severe end of a spectrum of disease that includes litis, and pilonidal sinuses (4) (Table 1). -
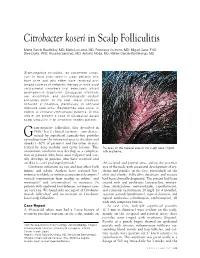
Citrobacter Koseri in Scalp Folliculitis
Citrobacter koseri in Scalp Folliculitis Marta Garcia-Bustinduy, MD; Maria Lecuona, MD; Francisco Guimera, MD; Miguel Saez, PhD; Sara Dorta, PhD; Rosalba Sanchez, MD; Antonio Noda, MD; Rafael Garcia-Montelongo, MD Gram-negative folliculitis, an uncommon condi- tion, is most often seen in older patients who have acne and who either have received pro- longed courses of antibiotic therapy or have used antibacterial cleansers that selectively inhibit gram-positive organisms. Citrobacter infections are uncommon, and dermatologists seldom encounter them. In the past, these infections occurred in hospitals, particularly in neonatal intensive care units. Bacteremias also occur in elderly or immunocompromised patients. In this article, we present a case of Citrobacter koseri scalp folliculitis in an otherwise healthy patient. ram-negative folliculitis, first described in 1968,1 has 2 clinical varieties—one charac- G terized by superficial comedo-free pustules extending from the infranasal area to the chin and cheeks (~80% of patients) and the other charac- terized by deep nodular and cystic lesions. This Pustules on the parietal area of the scalp were ringed uncommon condition may develop as a complica- with erythema. tion in patients who have acne vulgaris2 and usu- ally develops in patients who have received oral antibiotics over prolonged periods.3 the occipital and parietal areas, and on the posterior Citrobacter infections are rare and may affect both area of the neck, with occasional development of ery- infants and adults. Authors have reported bac- thema and papules on the face, particularly on the teremias in elderly or immunocompromised patients,4 chin and cheeks. Folliculitis decalvans and rosacea vertical transmission from mother to infant,5 and had been clinically diagnosed. -

Pyoderma Gangrenosum and Suppurative Hidradenitis Association, Overlap Or Spectrum of the Same Disease? Case Report and Discussion
38 EXPERIMENTAL AND THERAPEUTIC MEDICINE 20: 38-41, 2020 Pyoderma gangrenosum and suppurative hidradenitis association, overlap or spectrum of the same disease? Case report and discussion GABRIELA TURCU1-3, ROXANA IOANA NEDELCU2,4, IULIA TEODORA NEDELCU3, Anastasia HODOROGEA3,4, MIHAELA BALABAN2,5, ALICE BRINZEA4,6, LUCIANA Nichita7, CRISTIANA GABRIELA POPP7, SABINA ANDRADA ZURAC7 and RAZVAN THEODOR ANDREI7 1Department of Dermatology, Faculty of Medicine, Carol Davila University of Medicine and Pharmacy, 050474 Bucharest; 2Department of Dermatology, Derma 360° Clinic, 011273 Bucharest; 3Department of Dermatology, Colentina Clinical Hospital, 020125 Bucharest; 4Department of Pathophysiology, Faculty of Medicine, Carol Davila University of Medicine and Pharmacy, 020105 Bucharest; 5Department of Biochemistry, Faculty of Medicine, Carol Davila University of Medicine and Pharmacy, 050474 Bucharest; 6Department of Ambulatory, National Institute for Infectious Diseases Prof. Dr. Matei Balș, 020105 Bucharest; 7Department of Pathology, Colentina Clinical Hospital, 020125 Bucharest, Romania Received September 5, 2019; Accepted October 7, 2019 DOI: 10.3892/etm.2019.8150 Abstract. Suppurative hidradenitis and pyoderma gangrenosum gangrenosum, the healing aspect is more commonly seen are rare disorders that can be seen isolated or even more rare, in suppurative hidradenitis. Commonly seen in acne, in the as part of different autoinflammatory syndromes: Pyoderma healing phase of suppurative hidradenitis but more rarely in gangrenosum, acne, and hidradenitis suppurativa (PASH), pyoderma gangrenosum, the formation of comedones seem pyoderma gangrenosum, acne, pyogenic arthritis, and hidrad- to be a complex process and raise the question if these enti- enitis suppurativa (PAPASH) or psoriatic arthritis, pyoderma ties represent in our patient an association, an overlap or the gangrenosum, acne, and hidradenitis suppurativa (PsAPASH). -

Nevus Lipomatosus Superficialis on the Neck: an Unusual Location
CASE REPORT Nevus lipomatosus superficialis on the neck: an unusual location Farhad Malekzad, MD 1 Nevus lipomatosus superficialis (NLS) is a hamartomatous skin Farahnaz Bidari Zerehpoosh, MD 2 lesion defined by the presence of mature adipose tissues among Fahimeh Abdollahimajd, MD 1 the collagen bundles of the dermis. It is classified into two forms: the classical form and the solitary form. The classical NLS most Samira Salajeghe 1 commonly involves the pelvic or gluteal region. In this paper, we 1 Armaghan Kazeminejad, MD report a case of classical NLS over the neck because of its atypical site. In addition, our patient had some uncommon features of 1. Skin Research Center, Shahid NLS such as the presence of comedo-like lesions on the plaque Beheshti University of Medical and a foul-smelling discharge. Sciences, Tehran, Iran 2. Department of Pathology, Shahid Keywords: hamartoma, neck, nevus lipomatosus superficialis, skin tumor Beheshti University of Medical Science, Tehran, Iran Iran J Dermatol 2014; 17: 104-106 Corresponding Author: Fahimeh Abdollahimajd, MD Skin Research Center, Shohada-e- Tajrish Hospital, Shahid Beheshti University of Medical Science, Tehran, Iran Email: [email protected] Conflict of interest: none to declare Received: 20 May 2014 Accepted: 28 July 2014 INTRODUCTION classical NLS on the neck because of its unusual location and the presence of some uncommon Nevus lipomatosus superficialis (NLS) is an features of NLS. uncommon, benign hamartomatous skin tumor defined by dermal deposition of mature adipose CASE REPORT tissue that was first reported by Hoffamn and Zurhelle in 1921 1. It is classified into the solitary A 17-year-old boy presented to the Department form and the classical Hoffmann-Zurhelle from. -

HSVMA Guide to Congenital and Heritable Disorders in Dogs
GUIDE TO CONGENITAL AND HERITABLE DISORDERS IN DOGS Includes Genetic Predisposition to Diseases Special thanks to W. Jean Dodds, D.V.M. for researching and compiling the information contained in this guide. Dr. Dodds is a world-renowned vaccine research scientist with expertise in hematology, immunology, endocrinology and nutrition. Published by The Humane Society Veterinary Medical Association P.O. Box 208, Davis, CA 95617, Phone: 530-759-8106; Fax: 530-759-8116 First printing: August 1994, revised August 1997, November 2000, January 2004, March 2006, and May 2011. Introduction: Purebred dogs of many breeds and even mixed breed dogs are prone to specific abnormalities which may be familial or genetic in nature. Often, these health problems are unapparent to the average person and can only be detected with veterinary medical screening. This booklet is intended to provide information about the potential health problems associated with various purebred dogs. Directory Section I A list of 182 more commonly known purebred dog breeds, each of which is accompanied by a number or series of numbers that correspond to the congenital and heritable diseases identified and described in Section II. Section II An alphabetical listing of congenital and genetically transmitted diseases that occur in purebred dogs. Each disease is assigned an identification number, and some diseases are followed by the names of the breeds known to be subject to those diseases. How to use this book: Refer to Section I to find the congenital and genetically transmitted diseases associated with a breed or breeds in which you are interested. Refer to Section II to find the names and definitions of those diseases. -

Intense Pulsed Light for the Treatment of Rosacea and Telangiectasias
Journal of Cosmetic and Laser Therapy, 2011; 13: 216–222 ORIGINAL RESEARCH REPORT Intense pulsed light for the treatment of Rosacea and Telangiectasias RAMTIN KASSIR 1,2 , APARANJITA KOLLURU 3 & MARTIN KASSIR 4 1 Otolaryngology, St. Joseph’s Hospital, Wayne, United States, 2 Otolaryngology, NY/NJ Snoring and Sinus, New York, United States, 3 New York Medical College, New York, United States, and 4 Dermatology, Ste 140, 8335 Walnut Hill Lane, Dallas, TX, United States Abstract Background: Rosacea is a chronic disease that affects the aesthetic appearance of skin. The use of intense pulsed light (IPL) has shown signifi cant clearing in erythema, telangiectasia, and papules in rosacea. We seek parameters for IPL that will achieve optimal reduction in the appearance of rosacea with minimal adverse effects. Objective: To investigate the use of IPL on 102 patients at various parameters (fl uence and pulse duration) in the treatment of rosacea. Methods: 102 patients with mild to severe rosacea were treated with IPL treatment using the NaturaLight IPL system (Focus Medical, Bethel, CT). Patients received treatments at 1 – 3 week intervals, with an average of 7.2 treatments. The Reveal Imager (Canfi eld Scientifi c, Fairfi eld, NJ) was used for photodocumentation and analyses. Results: Treatments were given at 2.5/5 ms double, triple, or quadruple pulsed with 20 – 30 ms delay time. A 530 nm fi lter was used with fl uences varying from 10 – 30 J/cm 2 , or 10 – 20 J/cm 2 with a 420 nm fi lter for those patients with acneiform breakouts in addition to telangiectasias.