Thesis Title Goes Here
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
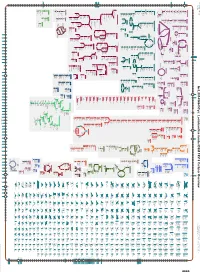
Generated by SRI International Pathway Tools Version 25.0, Authors S
Authors: Pallavi Subhraveti Ron Caspi Quang Ong Peter D Karp An online version of this diagram is available at BioCyc.org. Biosynthetic pathways are positioned in the left of the cytoplasm, degradative pathways on the right, and reactions not assigned to any pathway are in the far right of the cytoplasm. Transporters and membrane proteins are shown on the membrane. Ingrid Keseler Periplasmic (where appropriate) and extracellular reactions and proteins may also be shown. Pathways are colored according to their cellular function. Gcf_001434845Cyc: Lactobacillus hordei DSM 19519 Cellular Overview Connections between pathways are omitted for legibility. -
Effects of Nitrogen Level During Seed Production on Wheat Seed Vigor and Seedling Establishment at the Transcriptome Level
International Journal of Molecular Sciences Article Effects of Nitrogen Level during Seed Production on Wheat Seed Vigor and Seedling Establishment at the Transcriptome Level Daxing Wen, Haicheng Xu †, Liuyong Xie, Mingrong He, Hongcun Hou, Chenglai Wu, Yan Li and Chunqing Zhang * State Key Laboratory of Crop Biology, Agronomy College, Shandong Agricultural University, Tai’an 271018, China; [email protected] (D.W.); [email protected] (H.X.); [email protected] (L.X.); [email protected] (M.H.); [email protected] (H.H.); [email protected] (C.W.); [email protected] (Y.L.) * Correspondence: [email protected] † Current address: Yellow River Delta Agricultural Hi-Tech Industrial Demonstration Zone, Dongying 257347, China. Received: 26 September 2018; Accepted: 29 October 2018; Published: 31 October 2018 Abstract: Nitrogen fertilizer is a critical determinant of grain yield and seed quality in wheat. However, the mechanism of nitrogen level during seed production affecting wheat seed vigor and seedling establishment at the transcriptome level remains unknown. Here, we report that wheat seeds produced under different nitrogen levels (N0, N168, N240, and N300) showed significant differences in seed vigor and seedling establishment. In grain yield and seed vigor, N0 and N240 treatments showed the minimum and maximum, respectively. Subsequently, we used RNA-seq to analyze the transcriptomes of seeds and seedlings under N0 and N240 at the early stage of seedling establishment. Gene Ontology (GO) term enrichment analysis revealed that dioxygenase-activity-related genes were dramatically upregulated in faster growing seedlings. Among these genes, the top three involved linoleate 9S-lipoxygenase (Traes_2DL_D4BCDAA76, Traes_2DL_CE85DC5C0, and Traes_2DL_B5B62EE11). -

Journal of Proteomics 211 (2020) 103530
Journal of Proteomics 211 (2020) 103530 Contents lists available at ScienceDirect Journal of Proteomics journal homepage: www.elsevier.com/locate/jprot Qualitative proteomic comparison of metabolic and CM-like protein fractions in old and modern wheat Italian genotypes by a shotgun approach T ⁎ Antonella Di Francescoa, Rosaria Salettia, , Vincenzo Cunsoloa, Birte Svenssonb, Vera Muccillia, Pasquale De Vitac, Salvatore Fotia a Laboratory of Organic Mass Spectrometry, Department of Chemical Sciences, University of Catania, Viale A. Doria 6, 95125 Catania, Italy b Department of Biotechnology and Bioengineering, Technical University of Denmark, Søltofts Plads, Building 224, Kgs. Lyngby DK-2800, Denmark c CREA Research Centre for Cereal and Industrial Crops (CREA-CI), S.S. 673 km 25.200, 71122 Foggia, Italy ARTICLE INFO ABSTRACT Keywords: The close relationship between diet and health is generally recognized and the growing wellness and con- Old and modern wheat genotypes sciousness, especially in developed countries, have led to increasing interest for old wheat genotypes, based on High resolution mass spectrometry perceived health benefits. Although nutritional comparison between old and modern wheat varieties is still Proteome analysis controversial, it is generally accepted that old wheat genotypes remained unchanged over the last hundred years. Proteins By contrast, modern wheat genotypes are derived by modification of old wheats during the so-called “Green- Allergens Revolution” in the second half of the 20th century focusing on obtaining properties in terms of higher grain Food and nutrition yield. The present work reports the first comprehensive proteomic profiling and qualitative comparison at the molecular level of metabolic and Chloroform-Methanol (CM)-like protein fractions extracted from mature ker- nels of two old Sicilian durum wheat landraces, Russello and Timilia Reste Bianche, and Simeto, an improved durum wheat variety widespread in Italy and other Mediterranean countries and chosen as representative of the most widely commercial cultivars. -

Untersuchung Des Metabolismus Nicht-Kanonischer DNA-Basen In
Dissertation zur Erlangung des Doktorgrades der Fakultät für Chemie und Pharmazie der Ludwig-Maximilians-Universität München Untersuchung des Metabolismus nicht-kanonischer DNA-Basen in embryonalen Stammzellen Angie Gabriele Kirchner aus Ulm, Deutschland 2020 Erklärung Diese Dissertation wurde im Sinne von § 7 der Promotionsordnung vom 28. November 2011 von Herrn Prof. Dr. Thomas Carell betreut. Eidesstattliche Versicherung Diese Dissertation wurde selbstständig und ohne unerlaubte Hilfe erarbeitet. München, den 09.01.2020 ......................................... Angie G. Kirchner Dissertation eingereicht am: 09.01.2020 1. Gutachter: Prof. Dr. Thomas Carell 2. Gutachterin: Dr. Stefanie Kellner Mündliche Prüfung am: 31.01.2020 „I am just a child who has never grown up. I still keep asking these ‘how’ and ‘why’ questions. Occasionally, I find an answer.” Stephen Hawking Teile dieser Arbeit wurden in folgenden Journalen oder auf Fachkonferenzen publiziert: Publikationen F. Spada, S. Schiffers, A. Kirchner, Y. Zhang, O. Kosmatchev, E. Korytiakova, R. Rahimoff, C. Ebert, T. Carell, Oxidative and non-oxidative active turnover of genomic methylcytosine in distinct pluripotent states, bioRxiv 2019, 846584, 10.1101/846584. K. Iwan*, R. Rahimoff*, A. Kirchner*, F. Spada*, A. S. Schröder, O. Kosmatchev, S. Ferizaj, J. Steinbacher, E. Parsa, M. Müller, T. Carell, 5-Formylcytosine to cytosine conversion by C-C bond cleavage in vivo, Nat. Chem. Biol. 2018, 14, 72-78, 10.1038/nchembio.2531. R. Rahimoff*, O. Kosmatchev*, A. Kirchner*, T. Pfaffeneder, F. Spada, V. Brantl, M. Müller, T. Carell, 5-Formyl- and 5-carboxydeoxycytidines do not cause accumulation of harmful repair intermediates in stem cells, J. Am. Chem. Soc. 2017, 139, 10359-10364, 10.1021/jacs.7b04131. -
Pathogen and Drought Stress Affect Cell Wall and Phytohormone Signaling to Shape Host Responses in a Sorghum COMT Bmr12 Mutant Maya Khasin1,2, Lois F
Khasin et al. BMC Plant Biology (2021) 21:391 https://doi.org/10.1186/s12870-021-03149-5 RESEARCH ARTICLE Open Access Pathogen and drought stress affect cell wall and phytohormone signaling to shape host responses in a sorghum COMT bmr12 mutant Maya Khasin1,2, Lois F. Bernhardson1,2, Patrick M. O’Neill1,2, Nathan A. Palmer1,3, Erin D. Scully4,5, Scott E. Sattler1,3 and Deanna L. Funnell-Harris1,2* Abstract Background: As effects of global climate change intensify, the interaction of biotic and abiotic stresses increasingly threatens current agricultural practices. The secondary cell wall is a vanguard of resistance to these stresses. Fusarium thapsinum (Fusarium stalk rot) and Macrophomina phaseolina (charcoal rot) cause internal damage to the stalks of the drought tolerant C4 grass, sorghum (Sorghum bicolor (L.) Moench), resulting in reduced transpiration, reduced photosynthesis, and increased lodging, severely reducing yields. Drought can magnify these losses. Two null alleles in monolignol biosynthesis of sorghum (brown midrib 6-ref, bmr6-ref; cinnamyl alcohol dehydrogenase, CAD; and bmr12-ref; caffeic acid O-methyltransferase, COMT) were used to investigate the interaction of water limitation with F. thapsinum or M. phaseolina infection. Results: The bmr12 plants inoculated with either of these pathogens had increased levels of salicylic acid (SA) and jasmonic acid (JA) across both watering conditions and significantly reduced lesion sizes under water limitation compared to adequate watering, which suggested that drought may prime induction of pathogen resistance. RNA- Seq analysis revealed coexpressed genes associated with pathogen infection. The defense response included phytohormone signal transduction pathways, primary and secondary cell wall biosynthetic genes, and genes encoding components of the spliceosome and proteasome. -

SUPPLEMENTARY INFORMATION APPENDIX the Draft
SUPPLEMENTARY INFORMATION APPENDIX The draft genome of Tibetan hulless barley reveals adaptive patterns to the high stressful Tibetan Plateau Xingquan Zenga,b,1, Hai Longc,1, Zhuo Wangd,1, Shancen Zhaod,1, Yawei Tanga,b,1, Zhiyong Huangd,1, Yulin Wanga,b,1, Qijun Xua,b, Likai Maod, Guangbing Dengc, Xiaoming Yaod, Xiangfeng Lid,e, Lijun Baid, Hongjun Yuana,b, Zhifen Panc, Renjian Liua,b, Xin Chenc, QiMei WangMua,b, Ming Chend, Lili Yud, Junjun Liangc, DaWa DunZhua,b, Yuan Zhengd, Shuiyang Yuc, ZhaXi LuoBua,b, Xuanmin Guangd, Jiang Lid, Cao Dengd, Wushu Hud, Chunhai Chend, XiongNu TaBaa,b, Liyun Gaoa,b, Xiaodan Lvd, Yuval Ben Abuf, Xiaodong Fangd, Eviatar Nevog,2, Maoqun Yuc,2, Jun Wangh,i,j,2, Nyima Tashia,b,2 aTibet Academy of Agricultural and Animal Husbandry Sciences, Lhasa, Tibet 850002, China; bBarley Improvement and Yak Breeding Key Laboratory of Tibet Autonomous Region, Lhasa 850002, China; cChengdu Institute of Biology, Chinese Academy of Sciences, Chengdu 610041, P. R. China; dBGI-Tech, BGI-Shenzhen, Shenzhen 518083, China; eCollege of Life Science, University of Chinese Academy of Sciences, Beijing 100049, China; fProjects and Physics Section, Sapir Academic College, D.N. Hof Ashkelon 79165, Israel; gInstitute of Evolution, University of Haifa, Mount Carmel, Haifa 31905, Israel; hBGI-Shenzhen, Shenzhen 518083, China; iDepartment of Biology, University of Copenhagen, Copenhagen 2200, Denmark; jPrincess Al Jawhara Center of Excellence in the Research of Hereditary Disorders, King Abdulaziz University, Jeddah 21441, Saudi Arabia 1These authors contributed equally to this work. 2To whom correspondence should be addressed. Email: Nyima Tashi, [email protected]; Jun Wang, [email protected]; Maoqun Yu, [email protected]; or Eviatar Nevo, [email protected]. -

9<HTMERB=Ehdjgb> 9<HTTBOC=Cbcigh>
Life Sciences springer.com/NEWSonline R. A. Adams, University of Northern Colorado, N. K. Arora, School of Environmental Sciences, Uttar J. F. Brinkworth, City College of New York, NY, USA; Greeley, CO, USA; S. C. Pedersen, South Dakota State Pradesh, India (Ed) K. Pechenkina, City University of New York, NY. USA University, Brookings, SD, USA (Eds) Plant Microbe Symbiosis- (Eds) Bat Evolution, Ecology, and Fundamentals and Advances Primates, Pathogens, and Conservation Evolution Contents Contents Transactions amongst microorganisms and plant Contents Part 1. Evolutionary Patterns.- 1. How to Grow a in the composite rhizosphere habitat.- Plant- Acknowledgements.- 1. Primates, pathogens and Bat Wing.- 2. Time’s Arrow in the Evolutionary Microbe Interactions for Sustainable Agriculture: evolution.- Section I Immunity and Primate Evo- Development of Bat Flight.- 3. Evolution of Echo- Fundamentals and Recent Advances.- Plant- lution.- 2. Vertebrate Immune system evolution location.- 4. Nasal Emission and Noseleaves.- 5. microbe partnerships: implications for growth and comparative primate immunity.- 3. Genetic Bat Facial and Lip Projections: Unique Integu- and plant health.- Plant Microbe Symbiosis: variation in the immune system of Old World mentary Morphology.- 6. Bat Molecular Phylo- Perspectives and Applications.- Soil rhizobacteria monkeys: functional and selective effects.- 4. Toll- genetics: Past, Present, and Future Directions.- 7. can regulate the uptake of nutrients and undesir- like receptor function and evolution in primates.- Of Bats and Molecules: Chromosomal Characters able elements by plants.- The complex molecular 5. Impact of natural selection due to malarial for Judging Phylogenetic Relationships.- Part signaling network in microbe-plant interaction.- disease on human genetic variation.- 6. Parasitic 2. Ecology and Behaviour.- 8. -

Review Article Polyphenols in Colorectal Cancer: Current State of Knowledge Including Clinical Trials and Molecular Mechanism of Action
Hindawi BioMed Research International Volume 2018, Article ID 4154185, 29 pages https://doi.org/10.1155/2018/4154185 Review Article Polyphenols in Colorectal Cancer: Current State of Knowledge including Clinical Trials and Molecular Mechanism of Action Md Nur Alam, Muhammad Almoyad, and Fazlul Huq Discipline of Biomedical Sciences, Sydney Medical School, Te University of Sydney, Cumberland Campus C42, East Street, Lidcombe, NSW 1825, Australia Correspondence should be addressed to Fazlul Huq; [email protected] Received 1 August 2017; Revised 8 November 2017; Accepted 17 December 2017; Published 15 January 2018 Academic Editor: Michael Linnebacher Copyright © 2018 Md Nur Alam et al. Tis is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited. Polyphenols have been reported to have wide spectrum of biological activities including major impact on initiation, promotion, and progression of cancer by modulating diferent signalling pathways. Colorectal cancer is the second most major cause of mortality and morbidity among females and the third among males. Te objective of this review is to describe the activity of a variety of polyphenols in colorectal cancer in clinical trials, preclinical studies, and primary research. Te molecular mechanisms of major polyphenols related to their benefcial efects on colorectal cancer are also addressed. Synthetic modifcations and other future directions towards exploiting of natural polyphenols against colorectal cancer are discussed in the last section. 1. Introduction far, clearly identifed types or causes of CRC are hereditary nonpolyposis colorectal cancer, familial adenomatous poly- Epidemiological studies exhibiting protective efect of diets posis, infammatory bowel diseases, human papillomavirus, rich in fruits and vegetables against diferent types of cancer and acquired immunodefciency syndrome [4]. -
Root Proteome of Rice Studied by Itraq Provides Integrated Insight Into Aluminum Stress Tolerance Mechanisms in Plants
中国科技论文在线 http://www.paper.edu.cn JOURNAL OF PROTEOMICS 98 (2014) 189– 205 Available online at www.sciencedirect.com ScienceDirect www.elsevier.com/locate/jprot Root proteome of rice studied by iTRAQ provides integrated insight into aluminum stress tolerance mechanisms in plants Zhan Qi Wanga, Xiao Yan Xua, Qiao Qiao Gonga, Chen Xieb, Wei Fana, Jian Li Yanga, Qi Shan Linc, Shao Jian Zhenga,⁎ aState Key Laboratory of Plant Physiology and Biochemistry, College of Life Sciences, Zhejiang University, Hangzhou 310058, China bCenter for Bioinformatics, State Key Laboratory of Protein and Plant Gene Research, College of Life Sciences, Peking University, Beijing 100101, China cUAlbany Proteomics Facility, Center for Functional Genomics, University at Albany, Rensselaer, NY 12144, USA ARTICLE INFO ABSTRACT Article history: One of the major limitations to crop growth on acid soils is the prevalence of soluble Received 31 August 2013 aluminum ions (Al3+). Rice (Oryza sativa L.) has been reported to be highly Al tolerant; however, Accepted 27 December 2013 large-scale proteomic data of rice in response to Al3+ are still very scanty. Here, we used an Available online 9 January 2014 iTRAQ-based quantitative proteomics approach for comparative analysis of the expression profiles of proteins in rice roots in response to Al3+ at an early phase. A total of 700 distinct Keywords: proteins (homologous proteins grouped together) with >95% confidence were identified. Aluminum stress Among them, 106 proteins were differentially expressed upon Al3+ toxicity in -

Proteomic Dissection of the Rice-Fusarium Fujikuroi Interaction
Ji et al. BMC Genomics (2019) 20:91 https://doi.org/10.1186/s12864-019-5435-5 RESEARCHARTICLE Open Access Proteomic dissection of the rice-Fusarium fujikuroi interaction and the correlation between the proteome and transcriptome under disease stress Zhijuan Ji, Yuxiang Zeng, Yan Liang, Qian Qian* and Changdeng Yang* Abstract Background: Bakanae disease, caused by the fungus Fusarium fujikuroi, occurs widely throughout Asia and Europe and sporadically in other rice production areas. Recent changes in climate and cropping patterns have aggravated this disease. To gain a better understanding of the molecular mechanisms of rice bakanae disease resistance, we employed a 6-plex tandem mass tag approach for relative quantitative proteomic comparison of infected and uninfected rice seedlings 7 days post-inoculation with two genotypes: the resistant genotype 93–11 and the susceptible genotype Nipponbare. Results: In total, 123 (77.2% up-regulated, 22.8% down-regulated) and 91 (94.5% up-regulated, 5.5% down-regulated) differentially expressed proteins (DEPs) accumulated in 93–11 and Nipponbare, respectively. Only 11 DEPs were both shared by the two genotypes. Clustering results showed that the protein regulation trends for the two genotypes were highly contrasting, which suggested obviously different interaction mechanisms of the host and the pathogen between 93 and 11 and Nipponbare. Further analysis showed that a noticeable aquaporin, PIP2–2, was sharply upregulated with a fold change (FC) of 109.2 in 93–11, which might be related to pathogen defense and the execution of bakanae disease resistance. Certain antifungal proteins were regulated in both 93–11 and Nipponbare with moderate FCs. -
Generate Metabolic Map Poster
An online version of this diagram is available at BioCyc.org. Biosynthetic pathways are positioned in the left of the cytoplasm, degradative pathways on the right, and reactions not assigned to any pathway are in the far right of the cytoplasm. Transporters and membrane proteins are shown on the membrane. Periplasmic (where appropriate) and extracellular reactions and proteins may also be shown. Pathways are colored according to their cellular function. NisylCyc: Nicotiana sylvestris Cellular Overview Connections between pathways are omitted for legibility. Author: Aureliano Bombarely, Virginia Tech Clathrin Sec-independent heavy chain 2/ protein /Phytozome: Chloride translocase Bradi4g25570.1; AP-2 complex subunit conductance AP-2 complex protein TATA, Symbols: NDH- non-specific serine/ sigma//Phytozome: Clathrin regulatory protein subunit sigma/ Symbols: | chloroplastic/ O | NAD(P) threonine protein GRMZM2G139624_P01; light chain 1/ ICln//Symbols: /Symbols: | Major facilitator Plasma /Symbols: | H:plastoquinone kinase; Species: phenylalanine ammonia- /Symbols: | | nucleotide- SNARE-like superfamily membrane- Sulfate Sodium/ Sodium/ Bacterial sec- dehydrogenase Sodium/ Brachypodium Sulfate Sulfate Proton lyase; Species: Zea Clathrin light sensitive chloride superfamily protein | associated ORF transporter ORF ORF hydrogen hydrogen independent complex subunit O hydrogen distachyon; Gene: transporter transporter ORF pump- mays mays; Gene: chain protein | conductance protein | chr2:7383194- cation- 1.3 exchanger 2 exchanger 2 translocation -

Itraq-Based Proteome Profile Analysis of Superior and Inferior
You et al. BMC Plant Biology (2017) 17:100 DOI 10.1186/s12870-017-1050-2 RESEARCH ARTICLE Open Access iTRAQ-based proteome profile analysis of superior and inferior Spikelets at early grain filling stage in japonica Rice Cuicui You1,2, Lin Chen2, Haibing He1, Liquan Wu1*, Shaohua Wang2,3*, Yanfeng Ding2,3 and Chuanxi Ma1 Abstract Background: Large-panicle rice varieties often fail to achieve their yield potential due to poor grain filling of late- flowering inferior spikelets (IS). The physiological and molecular mechanisms of poor IS grain filling, and whether an increase in assimilate supply could regulate protein abundance and consequently improve IS grain filling for japonica rice with large panicles is still partially understood. Results: A field experiment was performed with two spikelet removal treatments at anthesis in the large-panicle japonica rice line W1844, including removal of the top 1/3 of spikelets (T1) and removal of the top 2/3 of spikelets (T2), with no spikelet removal as a control (T0). The size, weight, setting rate, and grain filling rate of IS were significantly increased after spikelet removing. The biological functions of the differentially expressed proteins (DEPs) between superior and inferior spikelets as well as the response of IS to the removal of superior spikelets (SS) were investigated by using iTRAQ at 10 days post anthesis. A total of 159, 87, and 28 DEPs were identified from group A (T0-SS/T0-IS), group B (T0-SS/T2-IS), and group C (T2-IS/T0-IS), respectively. Among these, 104, 63, and 22 proteins were up-regulated, and 55, 24, and 6 proteins were down-regulated, respectively.