UHI Evaluation
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Eat – Stay – See – Fort William.Pdf
Eat | Stay | See | Fort William If you are visiting Fort William, here are some options for accommodation, with a range to suit every budget. All accommodations are located within central Fort William, or are just a short journey from the train station. Accommodation List | Fort William Inverlochy Castle Myrtle Bank Guest House 5 Star Country House Hotel. Inverlochy is one 4 Star Guest House in a 1890’s Victorian villa located of Scotland’s finest luxury hotels beside Loch Linhe on the South side of Fort William Address: Torlundy, Fort William PH33 6SN Address: Achintore Rd, Fort William PH33 6RQ Location: 3.6 miles to Tom-na-Faire Station Square Location: 1.1 miles to Tom-na-Faire Station Square Phone: +44 (0)1397 702177 Phone: +44 (0)1397 702034 Email: [email protected] Email: [email protected] Web: www.inverlochycastle.com Web: www.myrtlebankguesthouse.co.uk The Grange Huntingtower Lodge 5 Star Bed and Breakfast set high above Loch Linnhe with 4 Star Bed and Breakfast (Gold Green Tourism Award) superb views to the Ardgour hills Address: Druimarbin, Fort William, PH33 6RP Address: The Grange, Grange Road, Fort William, PH33 6JF Location: 2.7 miles to Tom-na-Faire Station Square Location: 1.3 miles to Tom-na-Faire Station Square Phone: +44 (0)1397 700 079 Phone: +44 (0)1397 705 516 Email: [email protected] Email: [email protected] Web: www.huntingtowerlodge.com Web: www.grangefortwilliam.com When making a reservation, please mention that Wilderness Scotland have recommended them as a place to stay within Fort William. -
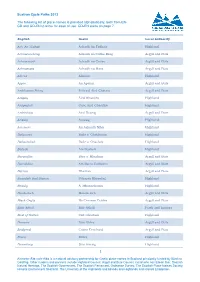
Sustran Cycle Paths 2013
Sustran Cycle Paths 2013 The following list of place-names is provided alphabetically, both from EN- GD and GD-EN to allow for ease of use. GD-EN starts on page 7. English Gaelic Local Authority Ach' An Todhair Achadh An Todhair Highland Achnacreebeag Achadh na Crithe Beag Argyll and Bute Achnacroish Achadh na Croise Argyll and Bute Achnamara Achadh na Mara Argyll and Bute Alness Alanais Highland Appin An Apainn Argyll and Bute Ardchattan Priory Priòraid Àird Chatain Argyll and Bute Ardgay Àird Ghaoithe Highland Ardgayhill Cnoc Àird Ghaoithe Highland Ardrishaig Àird Driseig Argyll and Bute Arisaig Àrasaig Highland Aviemore An Aghaidh Mhòr Highland Balgowan Baile a' Ghobhainn Highland Ballachulish Baile a' Chaolais Highland Balloch Am Bealach Highland Baravullin Bàrr a' Mhuilinn Argyll and Bute Barcaldine Am Barra Calltainn Argyll and Bute Barran Bharran Argyll and Bute Beasdale Rail Station Stèisean Bhiasdail Highland Beauly A' Mhanachainn Highland Benderloch Meadarloch Argyll and Bute Black Crofts Na Croitean Dubha Argyll and Bute Blair Atholl Blàr Athall Perth and kinross Boat of Garten Coit Ghartain Highland Bonawe Bun Obha Argyll and Bute Bridgend Ceann Drochaid Argyll and Bute Brora Brùra Highland Bunarkaig Bun Airceig Highland 1 Ainmean-Àite na h-Alba is a national advisory partnership for Gaelic place-names in Scotland principally funded by Bòrd na Gaidhlig. Other funders and partners include Highland Council, Argyll and Bute Council, Comhairle nan Eilean Siar, Scottish Natural Heritage, The Scottish Government, The Scottish Parliament, Ordnance Survey, The Scottish Place-Names Society, Historic Environment Scotland, The University of the Highlands and Islands and Highlands and Islands Enterprise. -

Kinneddar Lodges, Back of Keppoch
KINNEDDAR LODGES, BACK OF KEPPOCH £195,000 (GUIDE PRICE) Kinneddar Lodges are a collection of three well-presented holiday cottages: Loch Lomond, Loch Ness and Loch Morar. The lodges are located on a private site and situated at the Back of Keppoch, Arisaig. The site enjoys sea views towards Skye and close to local amenities in Arisaig and Mallaig. Property Summary Kinneddar Lodges boast a number of features such as:- • Exceptional sea views towards Skye • Ideal lifestyle / business opportunity • Private setting • Fort William (34 miles); Glasgow (142 miles) In addition to the lodges there is a storage shed. In all, the site extends to 0.34 acres (0.138 hectares) For Sale As a Whole KINNEDDAR LODGES BACK OF KEPPOCH ARISAIG, PH39 4NS £195,000 (GUIDE PRICE) Situation Accommodation Located close to Arisaig, a popular village on the West Coast Loch Morar of Scotland along the famous Road to the Isles. The Road • Open plan Kitchen, Dining and Living Room. to the Isles links Fort William and Mallaig (situated 35 and • One Double Bedroom. 8 miles from the site respectively). From Mallaig, there is a • One Twin Bedroom LIVING AREA BATHROOM BEDROOM daily ferry on to the Small Isles, Isle of Skye and the Knoydart • Showeroom with WC Peninsula. Kinneddar Lodges offer an ideal lifestyle Sunroom opportunity, being well placed for those looking to enjoy • living on the West Coast, an area renowned for outdoor Loch Ness and Loch Lomond activities such as walking, fishing, sailing, cycling, climbing • Open plan Kitchen, Dining and Living Room. - and all in stunning scenery that allows one to enjoy the • One Double Bedroom. -

1, Gillies Park, Mallaig Price Guide £68,000
1, GILLIES PARK, MALLAIG A beautifully presented and modern, groun d floor apartment situated above the fishing port of Mallaig. Within walking distance of the town centre. With ongoing upgrades this property forms an ideal buy to let or first-time buyer home. PRICE GUIDE £68,000 38 High Street Fort William PH33 6AT Home Report Valuation £72,000 Tel: 01397 703231 E-mail: [email protected] Website: www.solicitors-scotland.com KEY FEATURES: Ground floor apartment Great buy-to-let or first-time buyer home Recently decorated with modern finish and new carpet Modern Fitted Kitchen Bedroom with new built in wardrobes Modern shower room Double Glazing Energy Performance Rating E-49 LOCATION/AMENITIES: Mallaig is a community that has grown since the arrival of the world famous 'West Highland Railway line' and its thriving fishing industry. This picturesque fishing port provides a range of shops including 2 well- stocked supermarket, hotels, modern medical centre, primary and secondary schools, modern swimming pool and leisure facilities, railway connections via The West Highland Line to Fort William and is a major ferry terminal for ferry services to Knoydart, Skye, the Inner Isles and VIEWS TOWARD NEARBY MALLAIG HARBOUR South Uist in the Outer Isles. Mallaig Marina has excellent modern facilities, including pontoon berths and moorings. The nearest town is Fort William linked by the upgraded A830, 'Road to the Isles', a journey DESCRIPTION: which now takes under an hour. A lovely, modern ground floor, one bedroomed apartment situated above the fishing port of Mallaig Fort William’s is the main district town of Lochaber and is known as the and within walking distance of the town centre. -

Bayview, Camus Na Ha, Corpach, Fort William
BAYVIEW, CAMUS NA HA, CORPACH, FORT WILLIAM 2 5 1 11 D-65 PRICE GUIDE £385,000 T: 01397 703231 F: 01397 705070 E: [email protected] W: www.solicitors-scotland.com Situated in much sought after village location of Camus Na Ha, Corpach Set in a much sought after village location sits this fantastic family home that has been designed to take full advantage of the surroundings and fabulous views over Loch Eil and to Enjoys elevated position with fabulous views over Loch Eil and the surrounding hillsides the surrounding hillsides. There are just five substantial properties within the small and quiet Beautifully maintained and in immaculate order through-out community of Camus Na Ha which is primarily serviced by the village of Corpach. Build around 1987 the property spans 207m sq and enjoys an elevated position with arguably the best 5 Bedrooms with Master En-Suite views within the development. Landscaped Garden with Garage, Workshop and significant off road parking This five bedroom, detached family home provides spacious accommodation through-out and A Virtual Tour is available on request is maintained to an exceptionally high standard. The layout is set for family living with a Energy Performance Rating D-65 spacious kitchen-diner that has sliding doors providing access to the garden grounds and a beautiful living room with access to a patio terrace. Benefits include neutral décor, double glazing, oil fired heating supplemented by a wood burning stove, qualify fitted carpet has LOCATION/AMENITIES: been laid to each of the bedrooms, each of the four, front facing bedrooms enjoy fabulous The village of Corpach is located just 6 miles North of Fort William, it is a popular and vibrant loch and hillside views, underfloor heating to the en-suite bathroom and good storage through community with a full range of amenities to include a supermarket, museum, local bar and -out. -

The Seafood Restaurant & Café, Mallaig Offers in The
THE SEAFOOD RESTAURANT & CAFÉ, MALLAIG OFFERS IN THE REGION OF £62,000 INTRODUCTION MALLAIG BAY Available under leasehold Extremely popular Seafood Restaurant & Café business Excellent location, situated in the heart of Mallaig Seating over 2 floors, maximum capacity 64 Business expands to 138.89sq m Priced keenly for quick sale REASON FOR SALE ACCOMODATION The business would be ideally suited to an enthusiastic, hands-on owner-operator who would be The business is well known with a good base of repeat clientele within its community. The offered an excellent opportunity for a ready to work, walk-in business which has been keenly current leaseholder has been trading successfully for the last 15years. priced for a quick sale, due to our clients pending retirement. The Restaurant and Café is well branded with signage displayed across the frontage and SUMMARY operates over 2 floors. It is licensed and fully operational with all the cooking facilities and equipment, tills, coffee machines and much more. Maximum occupancy on the ground There is scope to develop the business further with the introduction of extending the season and floor of the Seafood Restaurant is 38. There is an attractive seating area that takes additional catering hours for the Café. Additionally, the business could actively promote a advantage of lovely views over Mallaig harbour. The Café on the first floor has a lunchtime take-away service. The Landlord has already agreed to assigning the lease and extending maximum occupancy of 26. There is currently free public parking a short walk from the the term time if required to do so. -

Download Trip Notes
Isle of Skye and The Small Isles - Scotland Trip Notes TRIP OVERVIEW Take part in a truly breathtaking expedition through some of the most stunning scenery in the British Isles; Scotland’s world-renowned Inner Hebrides. Basing ourselves around the Isles of Skye, Rum, Eigg and Muck and staying on board the 102-foot tall ship, the ‘Lady of Avenel’, this swimming adventure offers a unique opportunity to explore the dramatic landscapes of this picturesque corner of the world. From craggy mountain tops to spectacular volcanic features, this tour takes some of the most beautiful parts of this collection of islands, including the spectacular Cuillin Hills. Our trip sees us exploring the lochs, sounds, islands, coves and skerries of the Inner Hebrides, while also providing an opportunity to experience an abundance of local wildlife. This trip allows us to get to know the islands of the Inner Hebrides intimately, swimming in stunning lochs and enjoying wild coastal swims. We’ll journey to the islands on a more sustainable form of transport and enjoy freshly cooked meals in our downtime from our own onboard chef. From sunsets on the ships deck, to even trying your hand at crewing the Lady of Avenel, this truly is an epic expedition and an exciting opportunity for adventure swimming and sailing alike. WHO IS THIS TRIP FOR? This trip is made up largely of coastal, freshwater loch swimming, along with some crossings, including the crossing from Canna to Rum. Conditions will be challenging, yet extremely rewarding. Swimmers should have a sound understanding and experience of swimming in strong sea conditions and be capable of completing the average daily swim distance of around 4 km (split over a minimum of two swims) prior to the start of the trip. -
Mallaig High School Handbook
MALLAIG HIGH SCHOOL HANDBOOK HANDBOOK SESSION 2020-2021 Contents INTRODUCTION................................................................................................................................ 4 ETHOS .................................................................................................................................................. 4 STANDARDS AND QUALITY REPORT ........................................................................................ 5 PLANS FOR IMPROVEMENT ......................................................................................................... 6 PLACING REQUESTS – PARENTAL CHOICE .............................................................................. 6 SCHOOL CALENDAR ........................................................................................................................ 6 DAILY TIMETABLE .......................................................................................................................... 7 COMPLAINTS AND REQUESTS FOR SERVICE .......................................................................... 8 CODE OF POSITIVE BEHAVIOUR ................................................................................................. 8 PUPIL SUPPORT ............................................................................................................................... 9 HOUSE SYSTEM ............................................................................. Error! Bookmark not defined. ADDITIONAL SUPPORT NEEDS ................................................................................................ -

F7 Ferry Time Schedule & Line Route
F7 ferry time schedule & line map F7 Inverie View In Website Mode The F7 ferry line (Inverie) has 3 routes. For regular weekdays, their operation hours are: (1) Inverie: 7:30 AM - 6:15 PM (2) Mallaig: 8:15 AM - 6:45 PM (3) Tarbet: 2:15 PM Use the Moovit App to ƒnd the closest F7 ferry station near you and ƒnd out when is the next F7 ferry arriving. Direction: Inverie F7 ferry Time Schedule 2 stops Inverie Route Timetable: VIEW LINE SCHEDULE Sunday Not Operational Monday 7:15 AM - 6:15 PM Mallaig (For Knoydart) Ferry Terminal, Mallaig Tuesday 7:30 AM - 6:15 PM Inverie Ferry Landing, Inverie Wednesday 7:30 AM - 6:15 PM Thursday 7:30 AM - 6:15 PM Friday 7:30 AM - 6:15 PM Saturday 8:45 AM - 6:00 PM F7 ferry Info Direction: Inverie Stops: 2 Trip Duration: 30 min Line Summary: Mallaig (For Knoydart) Ferry Terminal, Mallaig, Inverie Ferry Landing, Inverie Direction: Mallaig F7 ferry Time Schedule 3 stops Mallaig Route Timetable: VIEW LINE SCHEDULE Sunday Not Operational Monday 8:00 AM - 6:45 PM Tarbet (Loch Nevis) Ferry Landing, Tarbet Tuesday 8:15 AM - 6:45 PM Inverie Ferry Landing, Inverie Wednesday 8:15 AM - 6:45 PM Mallaig (For Knoydart) Ferry Terminal, Mallaig Thursday 8:15 AM - 6:45 PM Friday 8:15 AM - 6:45 PM Saturday 9:15 AM - 6:30 PM F7 ferry Info Direction: Mallaig Stops: 3 Trip Duration: 30 min Line Summary: Tarbet (Loch Nevis) Ferry Landing, Tarbet, Inverie Ferry Landing, Inverie, Mallaig (For Knoydart) Ferry Terminal, Mallaig Direction: Tarbet F7 ferry Time Schedule 3 stops Tarbet Route Timetable: VIEW LINE SCHEDULE Sunday Not Operational Monday 2:15 PM Mallaig (For Knoydart) Ferry Terminal, Mallaig Tuesday 2:15 PM Inverie Ferry Landing, Inverie Wednesday 2:15 PM Tarbet (Loch Nevis) Ferry Landing, Tarbet Thursday 2:15 PM Friday 2:15 PM Saturday Not Operational F7 ferry Info Direction: Tarbet Stops: 3 Trip Duration: 75 min Line Summary: Mallaig (For Knoydart) Ferry Terminal, Mallaig, Inverie Ferry Landing, Inverie, Tarbet (Loch Nevis) Ferry Landing, Tarbet F7 ferry time schedules and route maps are available in an o«ine PDF at moovitapp.com. -

Corpach (Potentially Vulnerable Area 01/23)
Corpach (Potentially Vulnerable Area 01/23) Local Plan District Local authority Main catchment Highland and Argyll The Highland Council Ardgour coastal Summary of flooding impacts Summary of flooding impactsSummary At risk of flooding • <10 residential properties • <10 non-residential properties • £94,000 Annual Average Damages (damages by flood source shown left) Summary of objectives to manage flooding Objectives have been set by SEPA and agreed with flood risk management authorities. These are the aims for managing local flood risk. The objectives have been grouped in three main ways: by reducing risk, avoiding increasing risk or accepting risk by maintaining current levels of management. Objectives Many organisations, such as Scottish Water and energy companies, actively maintain and manage their own assets including their risk from flooding. Where known, these actions are described here. Scottish Natural Heritage and Historic Environment Scotland work with site owners to manage flooding where appropriate at designated environmental and/or cultural heritage sites. These actions are not detailed further in the Flood Risk Management Strategies. Summary of actions to manage flooding The actions below have been selected to manage flood risk. Flood Natural flood New flood Community Property level Site protection protection management warning flood action protection plans scheme/works works groups scheme Actions Flood Natural flood Maintain flood Awareness Surface water Emergency protection management warning raising plan/study plans/response study study Maintain flood Strategic Flood Planning Self help Maintenance protection mapping and forecasting policies scheme modelling Highland and Argyll Section 2 252 Local Plan District Corpach (Potentially Vulnerable Area 01/23) Local Plan District Local authority Main catchment Highland and Argyll The Highland Council Ardgour coastal Background This Potentially Vulnerable Area is The main river is the Allt Dogha. -

Masterplan for Mallaig Harbour FINAL V1.0 13-01-2017 CF Red.Pptx
MASTERPLAN FOR MALLAIG HARBOUR JANUARY 2017 Fisher Associates In association with: Wallace Stone and EnviroCentre Fisher Assoc. Ltd, April House, Rowes Lane, East End, Lymington, SO41 5SU, UK Tel: 01590 626 220 www.Misherassoc.co.uk Company Number: UK 7449155 C 1. Introduction 2 ONTENTS 2. Context for Mallaig Harbour 7 3. Market Assessment 21 4. Stakeholder Engagement 27 5. Masterplan 31 6. Implementation 39 Appendix A – Policy Review 45 Appendix B – Summary Assessment of Alternatives 49 Appendix C – Detailed Masterplan Proposals 53 Appendix D – Socio-Economic Impact 64 1 1. INTRODUCTION 2 1.1 O Overview of Mallaig Harbour Aerial Photos of the Harbour Mallaig Harbour is a key maritime hub for ferries, aquaculture, Qishing and marine leisure on the west coast of Scotland. Some VERVIEW of the key recent developments are summarised below. The harbour is run by Mallaig Harbour Authority (MHA), a Trust Port, with a Board contributing a range of skills and experience. MHA’s Board is committed to supporting activities that will beneQit the local community, both socially and OF economically. The harbour is a vital economic asset for the village of Mallaig M and its surrounding area, particularly in terms of the ALLAIG employment opportunities it affords, as well as enabling the development of Mallaig’s marine and wider tourism offer. H Key Developments in the Last Five Years ARBOUR All-year round Mallaig – Lochboisdale ferry service New marina and supporting landside facilities Securing Marine Harvest as anchor tenant Feed store to support aquaculture sector 3 1.2 M Masterplan Approach Approach The fundamental purpose of the masterplan is to provide a structured framework for the physical development and Analysis of problems and opportunities, informed by market assessment and stakeholder workshops, etc. -

From the Low Tide of the Sea to the Highest Mountain Tops Community Ownership of the Isle of Eigg Amanda Bryan: Chair IEHT Eigg
From the low tide of the sea to the highest mountain tops Community ownership of the Isle of Eigg Amanda Bryan: Chair IEHT Eigg Located off the West coast of Scotland Part of the Small Isles Size: 9km by 5km (31km2) Accessible by ferry from Mallaig 5 days a week in winter 6 days a week in summer (weather permitting) Services Primary School Secondary School (Mallaig) GP (Sleat, Skye) History 432:50 1997 56% The Buyout: 12th June 1997 Isle of Eigg Heritage Trust IEHT (IERA, SWT, HC) Company Secretary Eigg Eigg Trading Eigg Electric Eigg Tearoom Construction Achievements: IEHT An Laimhrig (Hub) o Shop o Tearoom o Craft Shop o Toilets/ Showers o IEHT Office Achievements: IEHT Housing: o Secure affordable tenancies o Refurbished Trust housing o Housing Policy: Affordable plots for self build o Sales: e.g. Lodge Achievements: IEHT Land Management: o Crofting: Created 4 new crofts o Restructured 3 Farms o Infrastructure improvements: Fencing, Dyking, Paths o Forest Management (250Ha) o Environmental improvements: Peatland, Native woodlands Achievements: IEHT Island Wide Electrification Scheme o Island Grid (11km cable) o 3 Hydro Schemes (1 * 100kW, 2 * 6kW) o 4 Wind Turbines (4 * 6kW) o PV (50kW) o Diesel Back Up o Energy Control Measures (5kW/ house, 10kW/ business) o Battery Storage Achievements: Partnerships o New Pier & Ferry: Highland Council & CalMac o GP Surgery: NHS Highland o Broadband: Hebnet o Volunteering: SNH & SWT o Eigg Lodge: Earth Connections o Community Hall: Eigg Community Association EU Support LEADER RDP Structural Funds