Integrated MRSA-Management (IMM) with Prolonged Decolonization
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Antiseptics and Disinfectants for the Treatment Of
Verstraelen et al. BMC Infectious Diseases 2012, 12:148 http://www.biomedcentral.com/1471-2334/12/148 RESEARCH ARTICLE Open Access Antiseptics and disinfectants for the treatment of bacterial vaginosis: A systematic review Hans Verstraelen1*, Rita Verhelst2, Kristien Roelens1 and Marleen Temmerman1,2 Abstract Background: The study objective was to assess the available data on efficacy and tolerability of antiseptics and disinfectants in treating bacterial vaginosis (BV). Methods: A systematic search was conducted by consulting PubMed (1966-2010), CINAHL (1982-2010), IPA (1970- 2010), and the Cochrane CENTRAL databases. Clinical trials were searched for by the generic names of all antiseptics and disinfectants listed in the Anatomical Therapeutic Chemical (ATC) Classification System under the code D08A. Clinical trials were considered eligible if the efficacy of antiseptics and disinfectants in the treatment of BV was assessed in comparison to placebo or standard antibiotic treatment with metronidazole or clindamycin and if diagnosis of BV relied on standard criteria such as Amsel’s and Nugent’s criteria. Results: A total of 262 articles were found, of which 15 reports on clinical trials were assessed. Of these, four randomised controlled trials (RCTs) were withheld from analysis. Reasons for exclusion were primarily the lack of standard criteria to diagnose BV or to assess cure, and control treatment not involving placebo or standard antibiotic treatment. Risk of bias for the included studies was assessed with the Cochrane Collaboration’s tool for assessing risk of bias. Three studies showed non-inferiority of chlorhexidine and polyhexamethylene biguanide compared to metronidazole or clindamycin. One RCT found that a single vaginal douche with hydrogen peroxide was slightly, though significantly less effective than a single oral dose of metronidazole. -

Effect of Polyhexamethylene Biguanide in Combination with Undecylenamidopropyl Betaine Or Pslg on Biofilm Clearance
International Journal of Molecular Sciences Article Effect of Polyhexamethylene Biguanide in Combination with Undecylenamidopropyl Betaine or PslG on Biofilm Clearance Yaqian Zheng 1,2,†, Di Wang 1,† and Luyan Z. Ma 1,3,* 1 State Key Laboratory of Microbial Resources, Institute of Microbiology, Chinese Academy of Sciences, Beijing 100101, China; [email protected] (Y.Z.); [email protected] (D.W.) 2 College of Life Sciences, University of Chinese Academy of Sciences, Beijing 100049, China 3 Savaid Medical School, University of Chinese Academy of Sciences, Beijing 100049, China * Correspondence: [email protected]; Tel.: +86-10-64807437 † These authors have contributed equally to this work. Abstract: Hospital-acquired infection is a great challenge for clinical treatment due to pathogens’ biofilm formation and their antibiotic resistance. Here, we investigate the effect of antiseptic agent polyhexamethylene biguanide (PHMB) and undecylenamidopropyl betaine (UB) against biofilms of four pathogens that are often found in hospitals, including Gram-negative bacteria Pseudomonas aeruginosa and Escherichia coli, Gram-positive bacteria Staphylococcus aureus, and pathogenic fungus, Candida albicans. We show that 0.02% PHMB, which is 10-fold lower than the concentration of commercial products, has a strong inhibitory effect on the growth, initial attachment, and biofilm formation of all tested pathogens. PHMB can also disrupt the preformed biofilms of these pathogens. In contrast, 0.1% UB exhibits a mild inhibitory effect on biofilm formation of the four pathogens. This concentration inhibits the growth of S. aureus and C. albicans yet has no growth effect on P. aeruginosa or E. coli. UB only slightly enhances the anti-biofilm efficacy of PHMB on P. -
Clincal Review(S)
CENTER FOR DRUG EVALUATION AND RESEARCH APPLICATION NUMBER: 208288Orig1s000 CLINICAL REVIEW(S) Division Director Review NDA 208288 Chlorhexidine gluconate/isopropyl alcohol Summary Review for Regulatory Action Date September 1, 2017 Theresa M. Michele, MD From Director, Division of Nonprescription Drug Products Subject Division Director Summary Review NDA/BLA # 208288 Applicant Name 3M Health Care Business Date of Submission March 3, 2017 PDUFA Goal Date September 3, 2017 SoluPrep™ Film-Forming Sterile Solution / 2%w/v Proprietary Name / chlorhexidine gluconate and 70% v/v isopropyl Established (USAN) Name alcohol Dosage Forms / Route of Surgical solution Administration / Strength Patient Preoperative Skin Preparation (adults and pediatric patients ≥ 2 months of age) Proposed Indication(s) • For preparation of the skin prior to surgery • Helps reduce bacteria that potentially can cause skin infection Recommended Regulatory Complete response Action Material Reviewed/Consulted OND Action Package, including: Names of discipline reviewers Medical Officer Review--DNDP Teresa Podruchny/Francis Becker Statistical Review Joo-Yeon Lee/Rima Izem Pharmacology Toxicology Review Charlie Thompson/Jane Sohn CMC Review/OBP Review Elise Luong/Maria Cruz-Fisher/Erika Pfeiler/ Swapan De Clinical Microbiology Review Michelle Jackson Clinical Pharmacology Review Sojeong Yi/Dennis Bashaw CDTL Review Francis Becker OSE/DMEPA Grace Jones/Chi-Ming Tu RPM DNDP Lara Akinsanya CDTL=Cross-Discipline Team Leader DMEPA=Division of Medication Error Prevention and Analysis -

In Vitro Evaluation of Polihexanide, Octenidine and Naclo/Hclo-Based Antiseptics Against Biofilm Formed by Wound Pathogens
membranes Article In Vitro Evaluation of Polihexanide, Octenidine and NaClO/HClO-Based Antiseptics against Biofilm Formed by Wound Pathogens Grzegorz Krasowski 1, Adam Junka 2,3,* , Justyna Paleczny 2, Joanna Czajkowska 3, Elzbieta˙ Makomaska-Szaroszyk 4, Grzegorz Chodaczek 5, Michał Majkowski 5, Paweł Migdał 6, Karol Fijałkowski 7 , Beata Kowalska-Krochmal 2 and Marzenna Bartoszewicz 2 1 Nutrikon, KCZ Surgical Ward, 47-300 Krapkowice, Poland; [email protected] 2 Department of Pharmaceutical Microbiology and Parasitology, Faculty of Pharmacy, Wrocław Medical University, 50-556 Wrocław, Poland; [email protected] (J.P.); [email protected] (B.K.-K.); [email protected] (M.B.) 3 Laboratory of Microbiology, Łukasiewicz Research Network—PORT Polish Center for Technology Development, 54-066 Wrocław, Poland; [email protected] 4 Faculty of Medicine, Lazarski University, 02-662 Warszawa, Poland; [email protected] 5 Bioimaging Laboratory, Łukasiewicz Research Network—PORT Polish Center for Technology Development, 54-066 Wrocław, Poland; [email protected] (G.C.); [email protected] (M.M.) 6 Department of Environment Hygiene and Animal Welfare, Wroclaw University of Environmental and Life Sciences, 51-630 Wrocław, Poland; [email protected] 7 Department of Microbiology and Biotechnology, Faculty of Biotechnology and Animal Husbandry, West Pomeranian University of Technology, 70-311 Szczecin, Poland; karol.fi[email protected] * Correspondence: [email protected]; Tel.: +48-71-784-06-75 Citation: Krasowski, G.; Junka, A.; Paleczny, J.; Czajkowska, J.; Makomaska-Szaroszyk, E.; Abstract: Chronic wounds complicated with biofilm formed by pathogens remain one of the most Chodaczek, G.; Majkowski, M.; significant challenges of contemporary medicine. -

Polyhexamethylene Biguanide (Mn = 1600; PDI =1.8) (PHMB)
Regulation (EU) No 528/2012 concerning the making available on the market and use of biocidal products Evaluation of active substances Assessment Report Polyhexamethylene biguanide (Mn = 1600; PDI =1.8) (PHMB) Product-type 2: Disinfectants and algaecides not intended for direct application to humans or animals June 2015 France Polyhexamethylene biguanide Product-type 2 June 2015 (Mn = 1600; PDI =1.8) (PHMB) TABLE OF CONTENTS 1 STATEMENT OF SUBJECT MATTER AND PURPOSE .................................... 4 1.1 Procedure followed ------------------------------------------------------- 4 1.2 Purpose of the assessment ---------------------------------------------- 4 2 OVERALL SUMMARY AND CONCLUSIONS ................................................. 6 2.1 General substance information / General product information ----- 6 2.1.1 Identity, Physico-chemical properties & Methods of analysis of the active substance ---------------------------------------------------------------------------------------------------------------------- 6 2.1.1.1 Identity .................................................................................... 6 2.1.1.2 Physico-chemical properties ........................................................ 9 2.1.1.3 Methods of analysis .................................................................... 9 2.1.2 Identity, Physico-chemical properties & Methods of analysis of the biocidal product 10 2.1.2.1 Identity ................................................................................... 10 2.1.2.2 Physico-chemical properties -
Chronic Venous Ulcers: a Comparative Effectiveness Review of Treatment Modalities Comparative Effectiveness Review Number 127
Comparative Effectiveness Review Number 127 Chronic Venous Ulcers: A Comparative Effectiveness Review of Treatment Modalities Comparative Effectiveness Review Number 127 Chronic Venous Ulcers: A Comparative Effectiveness Review of Treatment Modalities Prepared for: Agency for Healthcare Research and Quality U.S. Department of Health and Human Services 540 Gaither Road Rockville, MD 20850 www.ahrq.gov Contract No. 290-2007-10061-I Prepared by: Johns Hopkins University Evidence-based Practice Center Baltimore, MD Investigators Jonathan Zenilman, M.D. M. Frances Valle, D.N.P., M.S. Mahmoud B. Malas, M.D., M.H.S. Nisa Maruthur, M.D., M.H.S. Umair Qazi, M.P.H. Yong Suh, M.B.A., M.Sc. Lisa M. Wilson, Sc.M. Elisabeth B. Haberl, B.A. Eric B. Bass, M.D., M.P.H. Gerald Lazarus, M.D. AHRQ Publication No. 13(14)-EHC121-EF December 2013 Erratum January 2014 This report is based on research conducted by the Johns Hopkins University Evidence-based Practice Center (EPC) under contract to the Agency for Healthcare Research and Quality (AHRQ), Rockville, MD (Contract No. 290-2007-10061-I). The findings and conclusions in this document are those of the author(s), who are responsible for its contents; the findings and conclusions do not necessarily represent the views of AHRQ. Therefore, no statement in this report should be construed as an official position of AHRQ or of the U.S. Department of Health and Human Services. The information in this report is intended to help health care decisionmakers—patients and clinicians, health system leaders, and policymakers, among others—make well-informed decisions and thereby improve the quality of health care services. -

Pdfamf Product Recommendations
PRODUCT RECOMMENDATIONS Mineral ceilings Wood wool ceilings Soft board ceiling Metal ceiling Grid construction THERMATEX® THERMATEX® THERMATEX® THERMATEX® THERMATEX® HERADESIGN® HERADESIGN® TOPIQ® MONDENA® VENTATEC® Thermaclean S Aquatec Hygena Acoustic Hygena Alpha Hygena Schlicht Hygena superfine micro Efficient pro Hygena plain white System System C System C System C System C System C System B and System C System B and System C System C - - Material Mineral fibre Mineral fibre Mineral fibre Mineral fibre Mineral fibre Wood wool Wood wool Mineral wool Steel, galvanised Steel, galvanised Wood wool Wood wool Product type Surface Vinyl film laminated Fleece laminated Fleece laminated Fleece laminated Paint coated Fleece laminated Steel, galvanised Steel, galvanised surface texture with Pore sealant Clean room classification ISO 3 ISO 3 ISO 4 ISO 4 ISO 4 - - ISO 4 ISO 3 - ISO 14644-1 Room classification as Zone 1 - Zone 4 Zone 1 - Zone 4 Zone 1 - Zone 4 Zone 1 - Zone 4 Zone 1 - Zone 4 Zone 1 Zone 1 Zone 1 - Zone 4 Zone 1 - per NF S 90-351 Decontamination class CP 5 CP 5 CP 5 CP 5 CP 5 CP 5 - - as per NF S 90-351 (0,5) (0,5) (0,5) (0,5) (0,5) - - (0,5) Bacteriological cleanliness M1 M1 M1 M1 M1 - - M1 - - class as per NF S 90-351 Biocidal or fungicidal effect Escherichia coli Escherichia coli Escherichia coli Escherichia coli Escherichia coli Aspergillus niger Escherichia coli Aspergillus niger Aspergillus niger Aspergillus niger Aspergillus niger as per NF S 90-351 - - - - Special hygiene properties Stahpylococcus aureus MRSA Aspergillus -

Current Topics in Medicinal Chemistry, 2017, 17, 305-318 REVIEW ARTICLE
Send Orders for Reprints to [email protected] 305 Current Topics in Medicinal Chemistry, 2017, 17, 305-318 REVIEW ARTICLE ISSN: 1568-0266 Volume 17, Number 3 eISSN: 1873-5294 Impact Factor: Polymeric Quaternary Ammonium Compounds: Versatile Antimicrobial 2.9 The international journal for in-depth Materials reviews on Current Topics in Medicinal Chemistry BENTHAM SCIENCE Deanna L. Zubris1,*, Kevin P.C. Minbiole1,* and William M. Wuest2,* 1Department of Chemistry, Villanova University, Villanova, PA 19085, USA; 2Department of Chemistry, Temple Univer- sity, Philadelphia, PA 19122, USA Abstract: Polymeric Quaternary Ammonium Compounds (polyQACs) comprise a broad class of ma- terials with applications in medical implants, food processing, and surface sanitizing, amongst many A R T I C L E H I S T O R Y others. These polymeric substances are especially promising due to their potent antibacterial activity Received: May 13, 2015 and limited hemolytic toxicity. In particular, many polyQACs have superior therapeutic indices and a Revised: June 10, 2016 Accepted: August 10, 2016 lower likelihood of developing antibacterial resistance in comparison to their monomers, making them ideal materials for wound dressings, catheters, and other biomedical applications. This review DOI: 10.2174/15680266166661608291 55805 outlines the history and development, previous successes, current state of the research, and future di- rections of polyQACs in society. Keywords: Antimicrobial activity, Biofilm, Cationic polymers, Copolymer, Homopolymer, Hydrogel, Polyquaternium, Qua- ternary ammonium compound. A. BACKGROUND ON POLYQACS Another approach to QAC development has been in the field of polymeric QAC structures (polyQACs), which show 1. Introduction promise to address two limitations of monomeric QAC struc- The pathogenic capabilities of bacteria have been known tures – the need for removal from surfaces to minimize tox- for centuries; addressing this scourge has led to some of the icity [9], and well as the need for reapplication to maintain greatest advances in human health. -
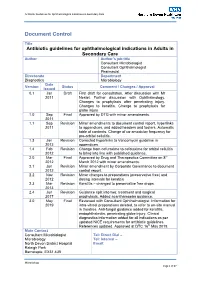
Antibiotic Guidelines for Ophthalmology V1.8 290413 Issue Date Review Date Review Cycle May 2019 May 2022 Three Years Consulted with the Following Stakeholders
Antibiotic Guidelines for Ophthalmological Indications in Secondary Care Document Control Title Antibiotic guidelines for ophthalmological indications in Adults in Secondary Care Author Author’s job title Consultant Microbiologist Consultant Ophthalmologist Pharmacist Directorate Department Diagnostics Microbiology Date Version Status Comment / Changes / Approval Issued 0.1 Jan Draft First draft for consultation. After discussion with Mr 2011 Nestel. Further discussion with Ophthalmology. Changes to prophylaxis after penetrating injury. Changes to keratitis. Change to prophylaxis for globe injury 1.0 Sep Final Approved by DTG with minor amendments. 2011 1.1 Sep Revision Minor amendments to document control report, hyperlinks 2011 to appendices, and added headers and footers. Automatic table of contents. Change of co-amoxiclav frequency for pre-orbital cellulitis. 1.3 Jan Revision Corrected hyperlinks to Vancomycin guideline in 2012 appendices. 1.4 Feb Revision Change from cefuroxime to cefotaxime for orbital cellulitis 2012 to bring into line with published guidance. 2.0 Mar Final Approved by Drug and Therapeutics Committee on 8th 2012 March 2012 with minor amendments. 2.1 Jun Revision Minor amendment by Corporate Governance to document 2012 control report. 2.2 Nov Revision Minor changes to preparations (preservative free) and 2012 dosing intervals for keratitis 2.3 Mar Revision Keratitis – changed to preservative free drops. 2013 2.4 Jun Revision Guidance split into two: treatment and surgical 2017 prophylaxis. Added acanthamoeba guidance. 3.0 May Final Reviewed with Consultant Ophthalmologist. Information for 2019 intra-vitreal preparations deleted, to refer to on-site manual in theatres. Anti-fungal guidance added for keratitis, endophthalmitis, penetrating globe injury. Clinical diagnostics information added for all indications as per updated NICE requirements for antibiotic guidelines. -

Disinfectant and Antiseptics Pdf
Disinfectant and antiseptics pdf Continue Antiseptics and disinfectants are very similar in that they are both used to kill microorganisms. They differ from each other, albeit in the composition of them, as well as their use. Antiseptics are used on living organisms, such as human skin, to kill any microorganisms living on the surface of the body. Disinfectants are used on non-living things such as countertops and handrails to kill microorganisms living on this inanimate surface. Antiseptics tend to have a lower concentration of a particular biocide, which is used in this product to clean the surface than that of a disinfectant. Since disinfectants are not intended for use on living tissues, but rather inanimate surfaces, they can use a higher concentration of biocide in the product, since there is no skin or tissue to worry about irritants. Antiseptics require a lower concentration of biocides, as too high concentrations of some biocides can cause a large amount of skin irritation. Some examples of antiseptics are mouthwash or hand sanitizer, both of which are safe for contact with your skin and also capable of being extremely effective in killing large numbers of microorganisms. Alcohol, bleach and formaldehyde are examples of various types of disinfectants used to kill microorganisms on the surface of any non-living objects. It is important that people know the difference between antiseptics and disinfectants, as they are both used for similar things, but in different ways. The use of disinfectant as an antiseptic is likely to irritate this tissue. In addition, the use of antiseptic as a disinfectant may result in less sufficient work to clean this surface due to the lower concentration of the biocide. -

Polyhexanide – Safety and Efficacy As an Antiseptic 707 – 11
REVIEW ARTICLE Review article Polyhexanide – safety and efficacy as an antiseptic 707 – 11 BACKGROUND Polyhexamethylene biguanide hydrochloride/polyhexanide/polyaminopropyl Hilde Fjeld biguanide (PHMB) is used as a disinfectant and antiseptic. This article discusses the use of [email protected] Department of Infection Prevention the substance as an antiseptic. We summarise published data on its antimicrobial efficacy Oslo University Hospital in vitro and its clinical efficacy and safety when used on skin, wounds and mucosa. and RELIS South-East MATERIAL AND METHOD A literature search was conducted in PubMed for articles published Oslo University Hospital in the last five years. Articles available as of June 2014 were considered. Egil Lingaas RESULTS Of 332 articles identified, 27 were included. In vitro studies have demonstrated anti- Department of Infection Prevention Oslo University Hospital microbial efficacy on gram-negative bacteria, gram-positive bacteria and Candida albicans. The clinical trials are small-scale, not well controlled and frequently sponsored by industry. Few adverse effects from the substance were reported. INTERPRETATION Better designed, larger-scale clinical trials of efficacy and safety are MAIN MESSAGE needed in order to give recommendations on the use of polyhexanide on skin, wounds and The clinical efficacy and safety of poly- mucosa. hexanide is poorly documented. In vitro studies have shown antimicrobial In all hospital departments one comes into ment process is underway in the EU for efficacy on gram-negative bacteria, gram- contact with disinfectants (used for techni- approval of PHMB products as biocides positive bacteria and Candida albicans. cal disinfection) and antiseptics (used on (substances for combatting unwanted orga- skin and mucosa) on a daily basis. -

Polyhexamethylene Biguanide:Polyurethane Blend Nanofibrous Membranes for Wound Infection Control
polymers Article Polyhexamethylene Biguanide:Polyurethane Blend Nanofibrous Membranes for Wound Infection Control Anna Worsley 1,2,* , Kristin Vassileva 1,2, Janice Tsui 2 , Wenhui Song 2 and Liam Good 1 1 Royal Veterinary College, Department of Pathobiology and Population Sciences, 4 Royal College Street, London NW1 0TU, UK; [email protected] (K.V.); [email protected] (L.G.) 2 University College London, Centre for Biomaterials in Surgical Reconstruction and Regeneration, Division of Surgery & Interventional Science, 9th floor, Royal Free Hospital, Pond Street, London NW3 2QG, UK; [email protected] (J.T.); [email protected] (W.S.) * Correspondence: [email protected] Received: 20 March 2019; Accepted: 20 May 2019; Published: 22 May 2019 Abstract: Polyhexamethylene biguanide (PHMB) is a broad-spectrum antiseptic which avoids many efficacy and toxicity problems associated with antimicrobials, in particular, it has a low risk of loss of susceptibility due to acquired antimicrobial resistance. Despite such advantages, PHMB is not widely used in wound care, suggesting more research is required to take full advantage of PHMB’s properties. We hypothesised that a nanofibre morphology would provide a gradual release of PHMB, prolonging the antimicrobial effects within the therapeutic window. PHMB:polyurethane (PU) electrospun nanofibre membranes were prepared with increasing PHMB concentrations, and the effects on antimicrobial activities, mechanical properties and host cell toxicity were compared. Overall, PHMB:PU membranes displayed a burst release of PHMB during the first hour following PBS immersion (50.5–95.9% of total released), followed by a gradual release over 120 h ( 25 wt % ≤ PHMB).