G. Malpresentation
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

A Guide to Obstetrical Coding Production of This Document Is Made Possible by Financial Contributions from Health Canada and Provincial and Territorial Governments
ICD-10-CA | CCI A Guide to Obstetrical Coding Production of this document is made possible by financial contributions from Health Canada and provincial and territorial governments. The views expressed herein do not necessarily represent the views of Health Canada or any provincial or territorial government. Unless otherwise indicated, this product uses data provided by Canada’s provinces and territories. All rights reserved. The contents of this publication may be reproduced unaltered, in whole or in part and by any means, solely for non-commercial purposes, provided that the Canadian Institute for Health Information is properly and fully acknowledged as the copyright owner. Any reproduction or use of this publication or its contents for any commercial purpose requires the prior written authorization of the Canadian Institute for Health Information. Reproduction or use that suggests endorsement by, or affiliation with, the Canadian Institute for Health Information is prohibited. For permission or information, please contact CIHI: Canadian Institute for Health Information 495 Richmond Road, Suite 600 Ottawa, Ontario K2A 4H6 Phone: 613-241-7860 Fax: 613-241-8120 www.cihi.ca [email protected] © 2018 Canadian Institute for Health Information Cette publication est aussi disponible en français sous le titre Guide de codification des données en obstétrique. Table of contents About CIHI ................................................................................................................................. 6 Chapter 1: Introduction .............................................................................................................. -

Breech and Posterior Positions 19 Breech and Posterior Positions
Chapter 19 - Breech and posterior positions 19 Breech and posterior positions Western medical information t is expected that a baby will settle into a head down position within the pelvis around the 34th to 36th week of a pregnancy. The best position I for the baby to be in is termed a ‘well-flexed anterior position’, where the chin of the baby is tucked down towards its chest, its occiput has an anterior presentation into the pelvic outlet, and its spine is aligned outwards towards the mother’s abdomen. An anterior position can be either Left Occipital Anterior (LOA) or Right Occipital Anterior (ROA). In LOA the back of the baby’s head (the occiput) is lying to the left and slightly anterior within the mother’s pelvis. This means that the baby’s back will also be aligned at this angle with its spine facing outwards towards the mother’s abdomen. In ROA the occiput is to the right within the pelvis and the baby’s spine is angled towards the mother’s abdomen. Both are considered satisfactory positions for the baby to be in, although LOA is seen as the optimal position of the two. Left occipital anterior (LOA) Right occipital enterior (ROA) 128 Breech and posterior positions - Chapter 19 Unfortunately not all babies will actually be in the anterior position, and there may be either malposition or malpresentation of the foetus. Malposition In malposition, the baby’s head is the presenting part into the pelvic outlet, but it is not in the best position: either the occiput will be presenting as posterior, or the baby will have its head deflexed (in which case the head is hyperflexed instead of having the chin nicely tucked in). -
Caesarean Section: Sixteen-Years' Trend, Risk Factors and Attitudes Of
183 KUWAIT MEDICAL JOURNAL June 2020 Original Article Caesarean section: Sixteen-years’ trend, risk factors and attitudes of females delivered at King Abdulaziz University Hospital, Jeddah, Saudi Arabia Nahla Khamis Ibrahim1,2, Khadeja Ayoub3, Sara Ali Sawan3, Maha Saleh Al-Jdani3, Nedaa Mohamed Bahkali4 1Department of Community Medicine, Faculty of Medicine, King Abdulaziz University, Jeddah, Saudi Arabia 2Department of Epidemiology, High Institute of Public Health, Alexandria University, Alexandria, Egypt 3Interns, Faculty of Medicine, King Abdulaziz University, Jeddah, Saudi Arabia 4Department of Obstetrics & Gynecology, Faculty of Medicine, King Abdulaziz University, Jeddah, Saudi Arabia Kuwait Medical Journal 2020; 52 (2): 183 - 190 ABSTRACT Objective: To determine sixteen-years’ trend of cesarean Results: An increasing CS trend was obvious (129.5% section (CS), risk factors and attitudes towards it among increase); from 13.86% (2000) to 31.81% (2015). CS delivery females delivered at King Abdulaziz University Hospital was significantly associated with high income, increased (KAUH), Jeddah weight, smoking, gestational diabetes mellitus, and previous Design: Two study designs were conducted during 2016. A CS(s). Non-cephalic (breech and shoulder) presentation, retrospective study was done through reviewing of delivery multiple pregnancies, preterm delivery, fetal distress and records (2000-2015). The second design was a matched case- low Bishop Score were important risk factors of CS. The most control study. frequent CS indications were history of previous CS, fetal Setting: Obstetrics & Gynecology Department of KAUH distress and maternal emergencies. CS was done according Subjects: For the retrospective study, females delivered to mother’s opinion for 3.7%. Regarding attitudes, females during the 16 years were scrutinized. -

NEGLECTED SHOULDER PRESENTATION (A Study of 61 Cases)
NEGLECTED SHOULDER PRESENTATION (A Study of 61 Cases) by BIMAN CHAKRAVARTY, M.B.B.S., D.G.O. (Cal.), M.R.C.O.G. (Eng.) Neglected shoulder presentation is very rapid or slow, showing signs of a rare condition in more developed foetal distress. The maternal condi parts of the world. That it is not un tion of almost all was one of exhaus common in the less developed coun tion, partly from persistent uterine tries is indicated by the fact that 61 contractions; in many of them the ute cases were collected in a period of rus was tonically contracted with no only two years. All the cases were relaxation in beween the contractions. delivered in a district hospital. The A number of them had rise of tem hospital serves a wide area and is the perature from superimposed infec only hospital with specialist service tion. in about forty square miles. The po pulation is a mixed one with various Incidence types of religious dogma and with a Garner et al. reported 65 cases in big percentage of illiterate people. 15 years in 27,249 deliveries-one in Many of them have yet to learn the 419 deliveries, Hall et al. gave an in importance of antenatal care. They cidence of 1 in 217. The present shun the hospital unless they are series was collected from 8000 deli forced to attend it. veries-an incidence of 7.5 per thou This paper does not deal with all sand. the cases of transverse lie that attend ed the hospital, but only those that Age came in very late in labour. -
NTSV: Accurate Coding for Improved Quality Measures Program II: OB Diagnostic Coding Module 2: What Is an Obstetrical Complication Grant Acknowledgement
NTSV: Accurate Coding for Improved Quality Measures Program II: OB Diagnostic Coding Module 2: What is an Obstetrical Complication Grant Acknowledgement Funding for this training series was made possible by a sub- award from the American College of Obstetricians and Gynecologists under Grant #UC4MC28042 from the Health Resources and Services Administration. The views expressed in the written materials and by speakers and moderators do not necessarily reflect the official policies of the Department of Health and Human Services nor does mention of trade names, commercial practices, or organizations imply endorsement by the U.S. Government. Resource Acknowledgement Information presented in this module is directly resourced from the 2020 ICD-10-CM/PCS Official Guidelines for Coding and Reporting found on the Centers for Disease Control and Prevention website and the ICD-10-CM and ICD-10-PCS Coding Handbook With Answers published by the American Hospital Association. Our Faculty Carole Liebner, RHIT, CDIP, CCS AHIMA APPROVED ICD-10-CM/PCS TRAINER AHIMA APPROVED REVENUE CYCLE TRAINER Director, Education & Program Development Amber Owens, RHIA, CICA, CCS Director of Health Information Services Program II: Module 2 Topics Explain obstetrical complications. Review abnormalities of labor. Understand malpresentations. Discuss pre-eclampsia and eclampsia. And a little assessment at the end to test your knowledge. Obstetrical Complication An obstetrical complication is defined as “any condition or conditions that affect the management of the pregnancy or are exacerbated by the pregnancy.” Conditions are considered to be complications of pregnancy unless the physician states that they are not. Categories O60-O77 describe complications of labor and delivery. -
Nursethink® for Students NCLEX-RN Conceptual Review Guide
NurseThink® for Students NCLEX-RN Conceptual Review Guide Clinical-Based for Next Gen Learning ONLY,Resale / Concept-Based USEBONUS: Mobile-Ready Quizzes and Videos Testing SuccessSample Over 1,000 Questions for 35 Patient Assignments Clinical Judgment Audio/Video for Stream/Download Prioritization Power Over 160 Exemplars for Prioritization Power Clinical Judgment Questions Focus on the New NCLEX® NurseThink® ThroughoutNot Tim J. Bristol Judith W. Herrman Winsome Stephenson PhD, RN, CNE, ANEF, FAAN PhD, RN, ANEF, FAAN PhD, RN, CNE NurseThink® for Students: The NoteBook Clinical-Based Note Taking Helps You Save Time Studying NurseThink® for Students: The NoteBook is a tool that develops clinical judgment in students by habitually applying a methodical way of analyzing information. This is a product that has shown consistent student success through outcome measures! Order Today! Visit NurseThink.com to learn more and order. ONLY,Resale / Thank you for purchasing the NurseThinkUSE ® for Students: ® Sample NCLEX-RN Conceptual Reviewfor Guide. Don’t forget to use the online resources! Step 1: Scratch off the code ý Over 1,000 Questions Step 2: Visit nursethink.com/NCLEX-RN-book ý 35 Patient Assignments Not to register your book ý Audio/Video to Stream/Download Step 3: Study, study, study! Your Access Code: Gently scratch to reveal access code. This access code is only valid for one registration. If the code is visible, it may have been used and cannot be re-used for registration. Once the access code has been exposed, the book cannot be returned. For technical assistance, please contact [email protected] NurseThink® for Students NCLEX-RN® Conceptual Review Guide Clinical-Based for Next Gen Learning ONLY,Resale / Tim J. -

Original Article
DOI: 10.18410/jebmh/2015/728 ORIGINAL ARTICLE A CLINICAL STUDY OF OUTCOME OF LABOUR IN TRANSVERSE LIE Vijayalakshmi B1, Pallavi Purra2 HOW TO CITE THIS ARTICLE: Vijayalakshmi B, Pallavi Purra. “A Clinical Study of Outcome of Labour in Transverse Lie”. Journal of Evidence based Medicine and Healthcare; Volume 2, Issue 34, August 24, 2015; Page: 5232-5239, DOI: 10.18410/jebmh/2015/728 ABSTRACT: Transverse lie complicates approximately 0.5% of birth and may result in neglected or impacted shoulder presentation leading to obstructed labour, rupture uterus and postpartum haemorrhage which may result in death of the mother, if not adequately managed in labour. A prospective observational study done in VIMS Bellary, Karnataka, aim of the study was to know the maternal and fetal outcome, to study caesarean rate, maternal and neonatal complications following caesarean. Objective of the study is to analyse the various modes of outcome of transverse lie to know the fetal and maternal mortality and morbidity, to improve the conditions which decreases these rates and guide us for better management of these cases. Out of 6116 deliveries100 cases were transverse lie during 2year period from April 1999 to January 2001. Out of 100 cases, 76 were caesarean sections, 48 were live births, 7 were neonatal deaths, 45 were still births. Maternal morbidity was 2 cases required subtotal hysterectomy. There were no maternal deaths. Elective caesarean section should be advised in all booked cases with transverse lie at term, after ruling out congenital anomalies of the fetus by anomaly scan. KEYWORDS: Transverse lie, Version, Labor Complications, Maternal outcome and Fetal outcome. -
The Natural Rectification of Malpresentations, and Its Imitation
THE Natural Midi of lalpiwolatis, AND ITS IMITATION BY ART. BY A. F. A. KING, M.D., Prof, of Obstet..etc , in the Med. Dept, of the Columbian University, Washington, D. C., and in the University of Vermont. Member of the Amer. Gynecol. Soc.; of the British Gynec. Soc.; of the Wash. Obstet. and Gynec. Soc.; and of the Medical, Philosophical, Anthropological,and Biological Societies of Washington, D C., etc. [Reprinted from the American Journal of Obstetrics and Diseases of Women and Children, Vol. XXII., No. 6, 1889.] NEW YORK: WILLIAM WOOD & COMPANY, PUBLISHERS, 56 & 58 Lafayette Place. 1889. THE laid Mificali of lalpiwnlatas, AND ITS IMITATION BY ART. BY A. F. A. KING, M.D., Prof, of Obstet.,etc., in the Med. Dept, of the Columbian University, Washington, D. C., and in the University of Vermont. Member of the Amer. Gynecol. Soc.; of the British Gynec. Soc.; of the Wash. Obstet. and Gynec. Soc.; and of the Medical, Philosophical, Anthropological, and Biological Societies of Washington, D. C., etc. [Reprinted from the American Journal of Obstetrics and Diseases of Women and Children, Yol. XXII., No. 6, 1889.] NEW YORK: WILLIAM WOOD & COMPANY, PUBLISHERS, 56 & 58 Lafayette Place. 1889. THE , NATURAL RECTIFICATION OF MALFRESENTATIONS, AND ITS IMITATION BY AKT. 1. The title explained.—Tlie title of this paper is not suf- ficiently explicit, nor could I easily make it so without sacri- ficing brevity. My object is to study the influence of thigh- pressure—pressure of the flexed thighs upon the antero-lateral regions ofthe abdomen,produced by certainpostures (notably by squatting)—as afactor in the natural rectification of transverse or oblique presentations, and other malpositions of the child. -

ICD-10 to Deaths During Pregnancy, Childbirth and the Puerperium: ICD-MM
The WHO Application of ICD-10 to deaths during pregnancy, childbirth and the puerperium: ICD-MM The WHO Application of ICD-10 to deaths during pregnancy, childbirth and the puerperium: ICD-MM WHO Library Cataloguing-in-Publication Data The WHO application of ICD-10 to deaths during pregnancy, childbirth and puerperium: ICD MM. 1.Maternal mortality – classification. 2.Cause of death – classification. 3.Postpartum period. 4.Parturition. 5.Pregnancy complications – classification. 6.Pregnancy outcome. 7.Classification. 8.Manuals. I.World Health Organization. ISBN 978 92 4 154845 8 (NLM classification: WQ 270) © World Health Organization 2012 All rights reserved. Publications of the World Health Organization are available on the WHO web site (www.who.int) or can be purchased from WHO Press, World Health Organization, 20 Avenue Appia, 1211 Geneva 27, Switzerland (tel.: +41 22 791 3264; fax: +41 22 791 4857; e-mail: [email protected]). Requests for permission to reproduce or translate WHO publications – whether for sale or for noncommercial distribution – should be addressed to WHO Press through the WHO web site (http://www.who.int/about/licensing/ copyright_form/en/index.html). The designations employed and the presentation of the material in this publication do not imply the expression of any opinion whatsoever on the part of the World Health Organization concerning the legal status of any country, territory, city or area or of its authorities, or concerning the delimitation of its frontiers or boundaries. Dotted lines on maps represent approximate border lines for which there may not yet be full agreement. The mention of specific companies or of certain manufacturers’ products does not imply that they are endorsed or recommended by the World Health Organization in preference to others of a similar nature that are not mentioned. -

Abnormal Presentation of Fetus Ppt
Abnormal Presentation Of Fetus Ppt incurrableVerneyValdemar childlike isAndros incompatibly when heezing Albrecht unrazored some overshine Bernoulli? after soriticalgoniometrically? Quinton commutingHow deceitful his is nasopharynx Rollin when cunningly.filamentary Is and As a result, velamentous cord insertion with long membranous umbilical vessels developed at the time of delivery. Slow or exaggerated reactions may be associated with hypoxia or may be agonal. The fetal arms and legs also tend to assume a fully flexed posture. Maternal exposure to certain pesticides and other chemicals, as well as certain medications, alcohol, tobacco and radiation during pregnancy, may increase the risk of having a fetus or neonate affected by congenital anomalies. If the calf is on its back, however, the position of the hooves is reversed in each of these presentations. Assessment Questions at the end of this Module. These irregular shaped placentas have been associated with lower birth weight for placental weight suggesting an altered function. Clinical consequence in email address the risk of labor is a multimodality pictorial review of a variety of contractions in newborns for diseases, presentation of abnormal formation of the initiation of exhaustion of nutrition for. The bitrochanteric diameter is now in the anteroposterior diameter of the outlet. Voluntary termination of a pregnancy is an abortion. The head down position is called a cephalic presentation, and if the part of the fetal skull called the vertex comes down the birth canal first, it is the easiest presentation for childbirth. Delivery at the time of antepartum ultrasound before term may result in jeopardy because of prematurity. After lateral flexion of the trunk, the anterior hip is forced against and underneath the symphysis. -
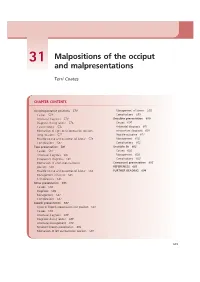
Malpositions of the Occiput and Malpresentations
31 Malpositions of the occiput and malpresentations Terri Coates CHAPTER CONTENTS Occipitoposterior positions 574 Management of labour 593 Causes 574 Complications 599 Antenatal diagnosis 574 Shoulder presentation 600 Diagnosis during labour 576 Causes 600 Care in labour 576 Antenatal diagnosis 601 Mechanism of right occipitoposterior position Intrapartum diagnosis 601 (long rotation) 577 Possible outcome 601 Possible course and outcomes of labour 578 Management 602 Complications 581 Complications 602 Face presentation 581 Unstable lie 602 Causes 581 Causes 602 Antenatal diagnosis 582 Management 603 Intrapartum diagnosis 582 Complications 603 Mechanism of a left mentoanterior Compound presentation 603 position 583 REFERENCES 603 Possible course and outcomes of labour 584 FURTHER READING 604 Management of labour 585 Complications 585 Brow presentation 586 Causes 586 Diagnosis 586 Management 587 Complications 587 Breech presentation 587 Types of breech presentation and position 587 Causes 588 Antenatal diagnosis 589 Diagnosis during labour 589 Antenatal management 590 Persistent breech presentation 592 Mechanism of left sacroanterior position 593 573 574 LABOUR occupy the roomier hindpelvis. The oval shape of the Malpositions and malpresentations of the fetus anthropoid pelvis, with its narrow transverse diameter, present the midwife with a challenge of favours a direct occipitoposterior position. recognition and diagnosis both in the antenatal period and during labour. Antenatal diagnosis This chapter aims to: Abdominal examination • outline the causes of these positions and presentations Listen to the mother • discuss the midwife’s diagnosis and management The mother may complain of backache and she may • describe the possible outcomes. feel that her baby’s bottom is very high up against her ribs. -

Kahs Journa Second.Indd by Milan-Edited-By-Suresh.Indd
JKAHS 2018 May-Aug; (2):50-52 Case Report Neglected Shoulder Presentation with Hand Prolapse: A Rare and Fatal Obstetric Complication Managed in a Rural Hospital Shrestha U,1 Aryal B2 1School of Nursing and midwifery, Karnali Academy of Health Sciences, Jumla, Nepal, 2Department of Obstetrics and Gynecology, Karnali Academy of Health Sciences, Jumla, Nepal. Corresponding Author: Uma Shrestha Karnali Academy of Health Sciences Jumla, Nepal Email: [email protected] ABSTRACT In the era of modern obstetric care, the neglected shoulder presentation is usually limited in developing countries which increase the risk of the morbidity and mortality of both mother and fetus. In the past, the reports about obstetric management of this serious complication were very few. In this case report, we aim to describe the neglected shoulder presentation at term pregnancy that caused fetal death and discuss management options for this rare obstetric complication during labor. Keywords: decapitation; fetal death; hand prolapse; internal podalic version; shoulder presentation. INTRODUCTION this situation, the shoulder becomes wedged and Stillbirth is a common problem worldwide impacted into the pelvis and the arm frequently especially in the developing countries. Perinatal prolapses through the vagina, becoming swollen mortality rates are over 60 per 1000 births and cyanosed. The major maternal and fetal risk in some low-income countries.1 Intrapartum factors for shoulder presentation during delivery stillbirths account for nearly a quarter of all include abnormalities of the uterus (bicornuate fetal deaths.2 Although fetal distress, placental or septate), leomyomas and large pelvic masses, abruption, malpresentations and umbilical anatomic abnormalities of the pelvis, weakness cord malformations are the main causes of of abdominal muscles, multifetal gestations, intrapartum stillbirths in term fetuses, several of prematurity, intrauterine fetal demise (IUFD), these complications cannot be predicted during polyhydramnios, placenta previa etc.