Download-PDF
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Magazine Can Be Printed in Whole Or Part Without the Written Permission of the Publisher
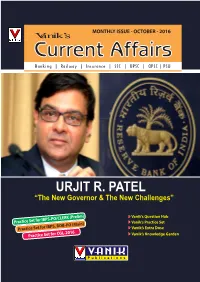
MONTHLY ISSUE - OCTOBER - 2016 CurrVanik’s ent Affairs Banking | Railway | Insurance | SSC | UPSC | OPSC | PSU URJIT R. PATEL “The New Governor & The New Challenges” Vanik’s Question Hub -PO/CLERK (Prelim) Practice Set for IBPS Vanik’s Practice Set -PO (Main) Practice Set for IBPS, BOB Vanik’s Extra Dose GL-2016 Practice Set for C Vanik’s Knowledge Garden P u b l i c a t i o n s VANIK'S PAGE INTERNATIONAL AIRPORTS OF INDIA NAME OF THE AIRPORT CITY STATE Rajiv Gandhi International Airport Hyderabad Telangana Sri Guru Ram Dass Jee International Airport Amristar Punjab Lokpriya Gopinath Bordoloi International Airport Guwaha ti Assam Biju Patnaik International Airport Bhubaneshwar Odisha Gaya Airport Gaya Bihar Indira Gandhi International Airport New Delhi Delhi Andaman and Nicobar Veer Savarkar International Airport Port Blair Islands Sardar Vallabhbhai Patel International Airport Ahmedabad Gujarat Kempegowda International Airport Bengaluru Karnatak a Mangalore Airport Mangalore Karnatak a Cochin International Airport Kochi Kerala Calicut International Airport Kozhikode Kerala Trivandrum International Airport Thiruvananthapuram Kerala Raja Bhoj Airport Bhopal Madhya Pradesh Devi Ahilyabai Holkar Airport Indore Madhya Pradesh Chhatrapati Shivaji International Airport Mumbai Maharashtr a Dr. Babasaheb Ambedkar International Airport Nagpur Maharashtr a Pune Airport Pune Maharashtra Zaruki International Airport Shillong Meghalay a Jaipur International Airport Jaipur Rajasthan Chennai International Airport Chennai Tamil Nadu Civil Aerodrome Coimbator e Tamil Nadu Tiruchirapalli International Airport Tiruchirappalli Tamil Nadu Chaudhary Charan Singh Airport Lucknow Uttar Pradesh Lal Bahadur Shastri International Airport Varanasi Uttar Pradesh Netaji Subhash Chandra Bose International Airport Kolkata West Bengal Message from Director Vanik Publications EDITOR Dear Students, Mr. -

The Journey of Atheist Centre & Its Founders
The Journey of Atheist Centre & its Founders Key Milestones Compiled by VIKAS GORA, Atheist Centre 1902-1912: Birth of Atheist social reformers 1902 November 15: Gora, born in Chatrapur, Ganjam District, Orissa. 1912 September 28: Saraswathi Gora, born in Vijayanagaram, Andhra Pradesh, India 1913-1923: Early Life, Marriage & Education May 7: Marriage of Gora & Saraswathi Gora. 1922 Gora travels to Madras to study M.A. Botany at Presidency College. 1923 Gora volunteers in All India Congress organized in Kakinada, Andhra Pradesh. 1924-1934: Employment & Dismissals in India & Sri Lanka, becoming atheists, challenging blind beliefs, demonstration for social equality and social reform activities. 1924 Gora studies science and religion and human behavior and gives lectures on Atheism across India. 1925 Gora becomes a Lecturer in American College in Madurai, Tamil Nadu Gora lives in a haunted house in Madurai, to prove that ghosts are unreal. 1926 Gora serves as a Lecturer at Agricultural College, Coimbatore and Saraswathi joins him in August. Gora joins Ananda College, Colombo as a Lecturer. 1927 Saraswathi joins Gora on September 26, defying the taboo that pregnant women should not see eclipse and views the solar eclipse in Colombo. Saraswathi views lunar eclipse at Vijayanagaram, Andhra Pradesh. September: Gora joins his alma mater P.R. College, Kakinada as Lecturer and Head. Gora removes his so-called sacred thread which is a caste symbol and has differences with his father on this. 1928 Eldest daughter Manorama (b. July 29) without any deformity even after Saraswathi views the eclipse. Gora is ex-communicated from his caste. Saraswathi Gora follows him. -

Kaloji Narayana Rao University of Health Sciences Act, 1986
KALOJI NARAYANA RAO UNIVERSITY OF HEALTH SCIENCES ACT, 1986. (ACT NO. 6 OF 1986) ARRANGEMENT OF SECTIONS Sections CHAPTER-I PRELIMINARY. 1. Short title, extent and commencement. 2. Definitions. CHAPTER-II THE UNIVERSITY 3. The University. 4. Objects of the University. 5. Powers and functions of the University. 6. Jurisdiction and admission to privileges. 7. Admission to the University. 8. Transfer of affiliation of certain colleges and institutions to the University. 9. Inspection and control. CHAPTER-III OFFICERS OF THE UNIVERSITY 10. Officers of the University. 11. The Chancellor. 12. The Vice- Chancellor. 13. Rector. 14. The Registrar. 15. The Finance Officer. 2 [Act No. 6 of 1986] 16. Deans of Faculties. 17. Conditions of service of the officers. CHAPTER-IV AUTHORITIES OF THE UNIVERSITY 18. Authorities of the University. 19. The Executive Council and its powers and functions. 20. Academic Senate and its powers and functions. 21. Planning Board. 22. Finance Committee. 23. The Boards of Studies. 24. Term of office of members of the Executive Council, the Academic Senate and the Planning Board. 25. The Faculties. CHAPTER-V UNIVERSITY FUNDS, ETC. 26. General Fund. 27. Constitution of other funds. 28. Borrowing of Money. 29. Certain restrictions in respect of financial matters. CHAPTER-VI STATUTES, ORDINANCES AND REGULATIONS 30. Statutes. 31. Statutes how made. 32. Ordinances. 33. Regulations. 34. Annual Report. [Act No. 6 of 1986] 3 35. Annual Accounts. 36. Financial Estimates. 37. Power to incur unforeseen Expenditure. CHAPTER-VII GENERAL 38. Filling of casual vacancies. 39. Protection of action taken in good faith. 40. Proceedings of the University authorities and bodies not invalidated by vacancies. -

Kaloji Narayana Rao University of Health Sciences, Telangana State, Warangal
KALOJI NARAYANA RAO UNIVERSITY OF HEALTH SCIENCES, TELANGANA STATE, WARANGAL NOTE : 1) NEET-PG-2019 QUALIFIED CANDIDATES DATA, RANK WISE AS UP-LOADED TO NBE AS HAVING COMPLETED MBBS IN THE STATE OF TELANGANA, RECEIVED FROM MINISTRY OF HEALTH GOVERNMENT OF INDIA. THIS IS ONLY FOR INFORMATION OF STUDENTS AND IS NOT A FINAL MERIT LIST FOR ADMISSION INTO P.G. COURSES IN THE STATE OF TELANGANA. NOTE:2) Final merit list will be prepared after submission of on-line applications to KNRUHS after Notification and after completion of verification of Original Certificates, as per eligibility, in accordance with presidential order and other government orders Sl.No. NEET RANK ROLL NO NAME CAT PH SCORE GENDER 1 3 1966050275 LALIT CHANDRA KUMMETHA General NO 982 MALE 2 146 1966056660 YERRAGUNTLA VENKATA NARAYANA General NO 885 MALE 3 152 1966053215 SAI SHIVANI RANGA General NO 884 FEMALE 4 223 1966056454 VOJJALA NIKHIL General NO 871 MALE 5 240 1966047242 CHOPPA VINAY KUMAR OBC NO 870 MALE 6 328 1966046722 BOBBILI KRISHNA CHAITHANYA OBC NO 860 MALE 7 360 1966045804 BOLLIPALLI KRISHNA CHAITHANYA REDDY General NO 857 MALE 8 362 1966048555 THOGALLA SURYA OBC NO 857 MALE 9 391 1966052881 PIPPIRI SAIKUMAR General NO 853 MALE 10 436 1966148483 KOTTE VARSHA General NO 850 FEMALE 11 452 1966051429 BAIRY THEJASREE OBC NO 848 FEMALE 12 558 1966148482 ASRA NOUREEN General NO 840 FEMALE 13 626 1966050815 M BHAVANA OBC NO 834 FEMALE 14 635 1966053488 NAVEEN KUMAR LANKA OBC NO 833 MALE 15 656 1966047317 D AMULYA REDDY General NO 832 FEMALE 16 667 1966055738 VIVEK -

Kaloji Narayana Rao University of Health
KALOJI NARAYANA RAO UNIVERSITY OF HEALTH SCIENCES, TELANGANA STATE WARANGAL NEET PG-2018 EXAM RESULT DATA OF CANDIDATES WHO HAVE REGISTERED AS COMPLETING MBBS FROM TELANGANA STATE AS RECEIVED FROM MINISTRY OF HEALTH, GOVT. OF INDIA. THE MERIT LIST OF ELIGIBLE CANDIDATES FOR ADMISSION INTO PG COURSES IN TELANGANA STATE WILL BE DISPLAYED ON WEBSITE AFTER SUBMISSION OF ONLINE APPLICATIONS BY NEEG PG-2018 QUALIFIED CANDIDATES AFTER NOTIFICATION BY KNRUHS AND AFTER VERIFICATION OF CERTIFICATES TOTAL SCORE ALL INDIA NEET S.No. ROLLNO NAME OF THE CANDIDATE PERCENTILE (OUT OF PG 2018 RANK 1200) 1 1805039828 KAVYA RAMINENI 840 47.00 99.9674 2 1805068277 S YAKSHITH 830 67.00 99.9519 3 1805055502 PURUSHOTHAM REDDY RAMIREDDY GARI 812 123.00 99.9061 4 1805108630 USHA MANASWINI RAMESH 796 204.00 99.8433 5 1805050256 KOSINIPALLI NAVEEN KUMAR 795 223.00 99.8317 6 1805050213 SUNKANNA K 794 233.00 99.8239 7 1805054416 SRIGADHA VIVEK KUMAR 794 229.00 99.8239 8 1805127993 KAZA KAVYA 785 313.00 99.7642 9 1805053299 PATLORI SAMANVITH 780 348.00 99.7293 10 1805132748 KONDA ROHITH 763 530.00 99.5912 11 1805050808 KONA KIRAN KUMAR REDDY 762 548.00 99.5772 12 1805052135 MANISHA SREERAMDASS 762 555.00 99.5772 13 1805108137 KAMANI NARESH BABU 761 566.00 99.5656 14 1805067938 CHIGURUPATI VEDA SAMHITHA 759 593.00 99.5462 15 1805054765 MACHA NIKHIL 756 631.00 99.516 16 1805051354 M SHIVA KUMAR 749 746.00 99.4229 17 1805052033 MEENUGU SUSHMA 749 753.00 99.4229 18 1805067961 EEGI VIDYA SREE 749 749.00 99.4229 19 1805107759 B SRAVYA 749 752.00 99.4229 20 1805048492 DONKANTI -

Supreme Court of India
SUPREME COURT OF INDIA LIST OF BUSINESS PUBLISHED UNDER THE AUTHORITY OF THE CHIEF JUSTICE OF INDIA FOR MONDAY 01ST MAY 2017 [Website : http://sci.nic.in] FINAL LIST SUPREME COURT OF INDIA Page 2 of 122 MONDAY 01ST MAY 2017 FINAL LIST SUPREME COURT OF INDIA Page 3 of 122 MONDAY 01ST MAY 2017 TABLE OF CONTENTS LIST OF BUSINESS MONDAY 01ST MAY 2017 COURT NO CORAM 1 [SPECIAL BENCH AT 10.30 A.M.] BEFORE : HON'BLE THE CHIEF JUSTICE HON'BLE MR. JUSTICE DIPAK MISRA HON'BLE MR. JUSTICE J. CHELAMESWAR HON'BLE MR. JUSTICE RANJAN GOGOI HON'BLE MR. JUSTICE MADAN B. LOKUR HON'BLE MR. JUSTICE PINAKI CHANDRA GHOSE HON'BLE MR. JUSTICE KURIAN JOSEPH HON'BLE THE CHIEF JUSTICE........................................................................................................................ 6 HON'BLE DR. JUSTICE D.Y. CHANDRACHUD HON'BLE MR. JUSTICE SANJAY KISHAN KAUL 2 HON'BLE MR. JUSTICE DIPAK MISRA........................................................................................................ 14 HON'BLE MR. JUSTICE A.M. KHANWILKAR HON'BLE MR. JUSTICE MOHAN M. SHANTANAGOUDAR BEFORE : HON'BLE MR. JUSTICE A.M. KHANWILKAR . [CHAMBER MATTERS] 3 HON'BLE MR. JUSTICE J. CHELAMESWAR............................................................................................... 23 HON'BLE MR. JUSTICE S. ABDUL NAZEER [SPECIAL BENCH AT 2. 00 P.M.] BEFORE : HON'BLE MR. JUSTICE J. CHELAMESWAR HON'BLE MR. JUSTICE ABHAY MANOHAR SAPRE 4 HON'BLE MR. JUSTICE RANJAN GOGOI.................................................................................................... 31 HON'BLE MR. JUSTICE NAVIN SINHA BEFORE : HON'BLE MR. JUSTICE NAVIN SINHA . [IN-CHAMBER MATTERS] 5 HON'BLE MR. JUSTICE MADAN B. LOKUR................................................................................................41 HON'BLE MR. JUSTICE DEEPAK GUPTA [SPECIAL BENCH AT 2. 00 P.M.] BEFORE : HON'BLE MR. JUSTICE MADAN B. -

Annual Report 2018-19
Annual Report 2018-19 Public Health Foundation of India Working towards a healthier India TABLE OF CONTENTS Chairman’s Message 03 From the President’s Pen 05 The Year Gone By 11 Academic Programmes 17 Research 41 Centres of Excellence 71 Health Technologies at PHFI 85 Health Promotion 93 Training & Capacity Building 99 Programmes Health System Support 113 and Technical Assistance Research Publications 125 2 Annual Report 2018-19 Public Health Foundation of India Working towards a healthier India CHAIRMAN’S MESSAGE “It is Health that is real Wealth and not pieces of gold and silver” – Mahatma Gandhi The Public Health Foundation of India (PHFI) has been playing a seminal role in improving public health by living up to its motto—“Knowledge to action”—as it replicates the virtuous cycle from research to impact. As our nation commemorates the 150th birth anniversary of Mahatma Gandhi this year, I am proud to state that PHFI has followed the path shown by the Mahatma, as its work in public health ameliorates the lives of individuals, households and communities, the faceless, nameless and marginalized amongst them. Over a decade of its existence, PHFI as a public-private initiative has rendered yeoman’s service in strengthening India’s public health institutional and systems capability, augmenting public health workforce and developing healthcare technologies. With its demonstrated track record in education, research, training and capacity building, its programmes have been adopted not only in our neighbourhood by South Asian countries but also by African countries. In line with Gandhi’s spirit, PHFI collaborates with, provides assistance to and works in tandem with a multitude of stakeholders ranging from academia, state governments, civil society, NGOs and communities at large. -

Padma Vibhushan * * the Padma Vibhushan Is the Second-Highest Civilian Award of the Republic of India , Proceeded by Bharat Ratna and Followed by Padma Bhushan
TRY -- TRUE -- TRUST NUMBER ONE SITE FOR COMPETITIVE EXAM SELF LEARNING AT ANY TIME ANY WHERE * * Padma Vibhushan * * The Padma Vibhushan is the second-highest civilian award of the Republic of India , proceeded by Bharat Ratna and followed by Padma Bhushan . Instituted on 2 January 1954, the award is given for "exceptional and distinguished service", without distinction of race, occupation & position. Year Recipient Field State / Country Satyendra Nath Bose Literature & Education West Bengal Nandalal Bose Arts West Bengal Zakir Husain Public Affairs Andhra Pradesh 1954 Balasaheb Gangadhar Kher Public Affairs Maharashtra V. K. Krishna Menon Public Affairs Kerala Jigme Dorji Wangchuck Public Affairs Bhutan Dhondo Keshav Karve Literature & Education Maharashtra 1955 J. R. D. Tata Trade & Industry Maharashtra Fazal Ali Public Affairs Bihar 1956 Jankibai Bajaj Social Work Madhya Pradesh Chandulal Madhavlal Trivedi Public Affairs Madhya Pradesh Ghanshyam Das Birla Trade & Industry Rajashtan 1957 Sri Prakasa Public Affairs Andhra Pradesh M. C. Setalvad Public Affairs Maharashtra John Mathai Literature & Education Kerala 1959 Gaganvihari Lallubhai Mehta Social Work Maharashtra Radhabinod Pal Public Affairs West Bengal 1960 Naryana Raghvan Pillai Public Affairs Tamil Nadu H. V. R. Iyengar Civil Service Tamil Nadu 1962 Padmaja Naidu Public Affairs Andhra Pradesh Vijaya Lakshmi Pandit Civil Service Uttar Pradesh A. Lakshmanaswami Mudaliar Medicine Tamil Nadu 1963 Hari Vinayak Pataskar Public Affairs Maharashtra Suniti Kumar Chatterji Literature -

South India to North America Journey of Journalist
South India to North America Journey of Journalist South India to North America Journey of Journalist Narisetti Innaiah South India to North America Journey of Journalist Page 1 Contents 1. Childhood - Sweet and Sour 4 2. Twists and turns at college level 11 3. College life is not that smooth (1953-58) 15 4. University Education 28 5. Taste of Politics 32 6. Untrained teacher 38 7. Entered Married Life 43 8. Encounter Different Personalities 47 9. Beyond Religion 49 10. A.B.Shah - Leader of Secular Movement 52 11. Joyful Life - Naveena, Raju 56 12. Can Reason Appeal 58 13. Komala Unique Person 60 14. Meandering into Research 63 15. Facing New Phase 66 16. Friendship with Chief Justice 68 17. A Decade of Experience 71 18. Reporting Legislative discussions 74 19. Helping Elected Representatives 78 20. Joyful Humanism 80 19. Bureau chief of Telugu daily 82 20. V.R. Narla dedicates his last play 89 21. Writer with human face 92 22. Chief Minister with difference 95 23. A friend in deed 98 South India to North America Journey of Journalist Page 2 24. Facing hardships 104 25. Encounter with academic cheats 107 26. At last owned a house 113 27. Unscientific alternatives 116 28. Playing with blind believers 119 29. Widening humanist horizon 128 30. Friendship with Rationalist, Skeptics 135 31. Feeling the Cosmos 141 32. India once again 145 33. Regional Associations in America 154 34. Thinkers groups 157 36. A story of Thesis 160 37. Pictures to remember South India to North America Journey of Journalist Page 3 111.1.. -

Annual Report Cover 2018 B
PUBLIC HEALTH FOUNDATION OF INDIA ANNUAL REPORT 2017-18 Presented at the PHFI Board Meeting on October 30-31, 2018 CONTENTS Chairman’s Message 3 From the President’s Pen 5 Who are we 9 The Year Gone By 20 Academic Programmes 27 Training Programmes 37 Research 49 Health System Support 73 Community Engagement 77 Peer Reviewed Publications (1st April 2017 onwards) 81 Annual Report 2017-18 1 2 Chairman’s Message Nation building involves dedicated efforts by many organisations and individuals who continually strive to better the country’s performance in every field of development. While each contribution in the many diverse areas of human welfare and societal advancement is of great value, efforts to protect, preserve and promote the health of our citizens is of utmost importance. This is not only because health is the best summative indicator of development in several sectors but also because health is a vital ingredient for achieving success in all other areas of human development and is pivotal for sustained economic growth. For that reason, I have gladly taken up the role of guiding the Public Health Foundation of India (PHFI) as its Chairman since July 2018. It was actually in 2016, that I came to appreciate and admire the intellectual rigour, careful planning and meticulous execution that researchers from PHFI brought to the design and implementation of the projects of the Centre for Environmental Health (CEH). I was also aware of the wide array of educational, training, research and health system strengthening activities that PHFI was undertaking across the country. Since I assumed the position of Chairman, I am gaining a greater understanding of the scope and impact of these initiatives. -

Kaloji Narayana Rao University of Health Sciences, Warangal, Telangana State
KALOJI NARAYANA RAO UNIVERSITY OF HEALTH SCIENCES, WARANGAL, TELANGANA STATE AYUSH UG ADMISSIONS 2017-18 FINAL ALLOTMENTS LIST OF ALL PHASES FOR BAMS/BHMS/BNYS COURSES COLLEGE - WISE. COLL :: BRKR(001) - DR. B.R.K.R. GOVT. AYURVEDIC COLLEGE, HYDERABAD. CRS :: BAMS(001) - BACHELOR OF AYURVEDA MEDICINE AND SURGERY ----------------------------------------------------------------------------------------------------- RANK NEET Roll STUDENT_NAME LOC CAT SX MIN PH NCC CAP Adm Details ------------------------------------------------------------------------------------------------------ 26602 909123798 DANDA ANKUSH REDDY OU OC M REG-UNR-OPEN-GEN-P1 44284 909120859 K P B SAI MRUDULA OU OC F REG-UNR-OPEN-FEM-P1 46179 909206720 KUSUMA SHASHANK BABU OU BCB M REG-UNR-OPEN-GEN-P1 46222 909200508 SAMMOI NAVYA SREE OU BCB F REG-UNR-OPEN-FEM-P1 48958 909120165 G AKHIL KUMAR OU BCD M REG-UNR-OPEN-GEN-P1 49994 909103561 OMDAS MAMATHA OU BCB F REG-LOC-OPEN-FEM-P1 51629 909109110 T SHIVA KUMAR OU BCD M REG-LOC-OPEN-GEN-P1 53787 909139775 KODURI SAI VYSHNAVI OU BCB F REG-LOC-OPEN-FEM-P1 59037 909112057 PALADUGU NIKHIL OU OC M REG-LOC-OPEN-GEN-P1 60970 909110652 S MYTHILI OU OC F REG-LOC-OPEN-FEM-P1 66589 909105903 DUDDU SRIKANTH OU BCD M REG-LOC-OPEN-GEN-P1 67803 909120304 K PREETHI REDDY OU OC F REG-LOC-OPEN-FEM-P1 68436 909207229 GADDAM NIKITHA OU BCB F REG-LOC-OPEN-FEM-P1 68756 909131019 RANABOTHU SUSHMA OU OC F REG-LOC-OPEN-FEM-P1 70466 900405966 KOTHAPALLY SAILASYA OU OC F REG-LOC-OPEN-GEN-P1 71072 909121214 RUKSANA BEGUM OU BCE F REG-LOC-OPEN-GEN-P1 73840 -

SC Paves Way for Disqualified Mlas to Contest Dec 5 Bypolls
Follow us on: RNI No. TELENG/2018/76469 @TheDailyPioneer facebook.com/dailypioneer Established 1864 Published From OPINION 6 MONEY 8 SPORTS 12 HYDERABAD DELHI LUCKNOW GUARANTORS VS NITA ON THE BOARD OF RED BHOPAL RAIPUR CHANDIGARH ENFORCERS METROPOLITAN MUSEUM OF ART ALERT BHUBANESWAR RANCHI DEHRADUN VIJAYAWADA *LATE CITY VOL. 2 ISSUE 35 HYDERABAD, THURSDAY NOVEMBER 14, 2019; PAGES 12 `3 *Air Surcharge Extra if Applicable GOT MORE THAN WHAT I ASKED FOR: HANSIKA ON HER CAREER { Page 11 } www.dailypioneer.com CJI is public CASH SEIZURES DURING TS ASSEMBLY POLLS 2018 authority, falls SC paves way for disqualified under RTI: SC Big politicos have the PNS n NEW DELHI MLAs to contest Dec 5 bypolls The Supreme Court on Wednesday held that the last laugh in poll cases office of the Chief Justice of PNS n NEW DELHI India is a public authority and SCdecisionhasexposed L VENKAT RAM REDDY falls within the ambit of the The Supreme Court on n HYDERABAD Right to Information Act. Wednesday upheld the dis- 'OpKamal:Congress A five-judge Constitution qualification of 17 Congress- NEW DELHI: Congress It is an open secret that the bench headed by Chief JD(S) MLAs in Karnataka by the spokesperson Randeep Singh flow of money and liquor dur- Justice Ranjan Gogoi upheld then Assembly Speaker but Surjewala on Wednesday said ing elections cannot be pre- the 2010 Delhi High Court paved the way for them to con- the Supreme Court's decision vented altogether. The reasons verdict and dismissed three test the December 5 by-polls on on the disqualification of 17 are obvious.