Since 1972, James A. Haley Veterans' Hospital (JAHVH) Has Been Improving
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

APPENDIX of DICTATION TEMPLATES Undergraduate Medical Education Approved By: Clerkship & Electives Commi
APPENDIX OF DICTATION TEMPLATES Undergraduate Medical Education Approved by: Clerkship & Electives Committee Date of original approval: August, 2013 Date of last review: N/A Date of next scheduled review: August, 2014 I. PURPOSE The following dictation samples are included to provide clinical clerks with guidance. II. DEFINITIONS CTU Clinical Teaching Unit MRP Most Responsible Physician PCCU Paediatric Critical Care Unit III. APPENDIX CTU - Discharge Summary Dictation Template All patients who 1) were admitted for seven or more days, and/or 2) had been admitted to the PCCU (Paediatric Critical Care Unit), and/or 3) had a complex condition or complicated course in hospital require a dictated (or typed) discharge summary. 1. Required initial information: Your name and position, most responsible physician (MRP) on the day of discharge, patient’s first and last name, PIN, who should receive this discharge summary (the MRP, the referring physician if one is known, the paediatrician or family physician of the patient (if not the referring physician), and other consultants who are going to see the patient in follow-up. Example: “This is John Smith, clinical clerk for Dr. X, dictating on patient Getme Outofhere, PIN 00000000. Please forward copies to Dr. X, Victoria Hospital, Dr. Y, family physician in London, Dr. Z, Paediatrician in London.” 2. Most responsible diagnosis: Diagnosis primarily responsible for the patient’s current admission. 3. History of present illness: Essential history of chief complaint as given by patient and/or care providers. It should include a concise summary of the relevant information from the time the symptoms started and up to the arrival at the Emergency Department. -
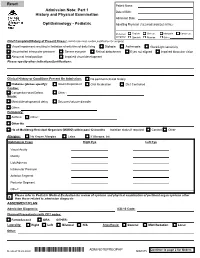
Adm Notepreophp
Patient Name: Admission Note: Part 1 Date of Birth: History and Physical Examination Admission Date: Ophthalmology - Pediatric Admitting Physician (FULL NAME W/MIDDLE INITIAL): Preferred English Chinese Mandarin Cantonese Language Spanish Russian Other: Chief Complaint/History of Present Illness: (admit note must contain justification for surgery) Visual impairment resulting in limitation of activities of daily living Diplopia Asthenopia Glare/Light sensitivity Uncontrolled intraocular pressure Severe eye pain Retinal detachment Eyes not aligned Impaired binocular vision Abnormal head position Impaired visual development Please specify other indications/justifications: Clinical History or Conditions Present On Admission: No pertinent clinical history Diabetes (please specify): Insulin Dependent Oral Medication Diet Controlled Cardiac: Congenital Heart Defect Other : Neuro: Mental/developmental delay Seizures/seizure disorder Other: Pulmonary: Asthma Other : Other Hx: Hx of Multidrug-Resistant Organism (MDRO) within past 12 months Isolation status if required: Contact Other Allergies: No Known Allergies Latex If Allergies, list: Ophthalmic Exam Right Eye Left Eye Visual Acuity Motility Lids/Adnexa Intraocular Pressure Anterior Segment Posterior Segment Other: Please refer to Pediatric Medical Evaluation for review of systems and physical examination of pertinent organ systems other X than those related to admission diagnosis ASSESMENT/PLAN Admission Diagnosis: ICD-10 Code: Planned Procedure(s) with CPT codes: FemtoSecond ORA OTHER: Laterality: Right Left Bilateral N/A Anesthesia: General MAC/Sedation Local Other: Continue to page 2 for Orders Revised 10.22.2020 *ADM NOTEPREOPHP* ADM NOTEPREOPHP ADM.075 Patient Name: Admission Note: Part 2 History and Physical Examination Date of Birth: Admission Date: Ophthalmology - Pediatric Admitting Physician (FULL NAME W/MIDDLE INITIAL): Preferred English Chinese Mandarin Cantonese Language Spanish Russian Other: 1. -

Disaster Management at Health Care Settings
Disaster management at Health Care Settings Comprehensive assessment and effective mitigation Shreen Gaber Disaster management at Health Care Settings Shreen Gaber Content Preface……………………………………………………………….. ˅ Introduction…………………………………………………………... 7 Disaster and disaster management concept………………………….. 9 Egyptian disaster statistics…………………………………………… 11 Effective communication, notification & alert disaster announce…… 11 Risk communication…………………………………………………. 14 Top seven trails of effective management…………………………… 15 Disaster management and role of intuition…………………………... 16 Disaster Management Standards……………………………………... 16 Different type of disasters according to hospital responsibilities……. 19 Nursing preparing for disasters………………………………………. 20 Hospital emergency codes…………………………………………… 23 Leadership theories and disaster management………………………. 24 Disaster leadership…………………………………………………… 27 The role leaders and administrators' …………………....................... 30 Ethical changes, evidence based and disaster management…………. 31 Reputation Repair and Behavioral Intentions……………………….. 33 Phases of disaster: Pre crisis phase………………………………….. 34 Hospital preparedness assessment Checklist………………………… 35 Disaster management plan…………………………………………… 39 Disaster management team…………………………………………... 40 The role of each team member………………………………………. 42 Crisis phase…………………………………………………………... 47 Different disasters' response…………………………………………. 55 Evacuation plan……………………………………………………… 69 Shelter in place………………………………………………………. 70 General building safety and security………………………………… -

General Rules of the Marquette General Health System Medical Staff
General Rules of the Marquette General Health System Medical Staff I. PATIENT ADMISSION, ALTERNATE COVERAGE, TRANSFER, DISCHARGE AND DEATH 1.1 ADMISSION CRITERIA 1.1-1 Who may admit patients. Only a Member with admitting privileges may admit or co-admit a patient to the Hospital. Except as provided for Qualified Oral Surgeons, Podiatrists and Independent Allied Health Professionals in the Medical Staff Bylaws, a physician Member will be responsible for the general medical care and treatment of every patient admitted to the Hospital. Medical care may be provided by a Resident, other specified professional personnel or Allied Health Staff members provided they are working under the supervision of a Practitioner with clinical privileges. Medical care will be provided only by Members and Hospital support staff authorized to perform such services. 1.1-2 Admission Information. An admitting Practitioner will provide the following information in the patient’s medical record, if such information is available to the admitting Practitioner: (a) Provisional diagnosis. (b) A valid reason for admitting the patient, including information to support the medical necessity and the appropriateness of the admission. (c) Information needed to properly care for the patient being admitted. (d) Information needed to protect the patient from himself/herself. (e) Information needed to protect Hospital personnel and others from potential problems or dangers presented by the patient. (f) Information deemed necessary by the Hospital. 1.1-3 Admission of potentially suicidal or dangerous patients. If an admitting Practitioner reasonably believes a patient admitted for other purposes is potentially suicidal or dangerous to himself/herself or others, the admitting Practitioner will promptly obtain a consultation from a suitable mental health professional. -
Resident Supervision Attending Practitioner Responsibilities for Physician, Dental, Optometry, & Podiatry Residents
U.S. DEPARTMENT OF VETERANS AFFAIRS Resident Supervision Attending Practitioner Responsibilities for Physician, Dental, Optometry, & Podiatry Residents “Supervising Practitioner” (synonymous with “Attending”): Responsible for all care in which interns, residents or fellows are involved. “Resident” is used to apply to physician, dentist, optometrist, and podiatrist residents and fellows, regardless of training level. Documentation of all patient encounters must identify the supervising practitioner (attending) by name and indicate the level of involvement. Depending upon the clinical situation, Four types of documentation of resident supervision are allowed: 1. Attending’s progress note or other entry into the patient health record. 2. Attending’s addendum to the resident admission or progress note. 3. Co-signature by the attending implies that the attending has reviewed the resident note or other health record entry, and absent an addendum to the contrary, concurs with the content of the resident note or entry. Use of CPRS function "Additional Signer" is not acceptable for documenting supervision. 4. Resident documentation of attending supervision. [Includes involvement of the attending and the attending’s level of supervision or oversight responsibility (e.g., "I have seen and discussed the patient with my attending, Dr. 'X', and Dr. 'X' agrees with my assessment and plan"), at a minimum, the responsible attending should be identified (e.g., "The attending of record for this patient encounter is Dr. 'X'")] Outpatient: New Patient Visit (includes Emergency Department visits) Attending must be physically present in the clinic. Every patient who is new to the facility must be seen by or discussed with an attending. Documentation: An independent note, addendum to the resident's note, or resident note description of attending involvement. -

Student Clerkship Guide a Comprehensive Guide to Clerkship at the Ottawa Hospital
STUDENT CLERKSHIP GUIDE A COMPREHENSIVE GUIDE TO CLERKSHIP AT THE OTTAWA HOSPITAL Gemma Cox and Stephanie Lubchansky MD 2015 CANDIDATES SPECIAL THANKS To Dr. Krista Wooller for her guidance, support, and feedback during the writing process. The Faculty of Medicine at the University of Ottawa for supporting this endeavor. EDITORS-IN-CHIEF EDITORS Gemma Cox, MD Candidate 2015 Pierre-Olivier Auclair, Mandatory Selectives Coordinator Stephanie Lubchansky, MD Candidate 2015 Dr. Contreras-Dominguez, Internal Medicine Rotation Director FACULTY SUPERVISOR Kelly Frydrych, MD Candidate 2015 Dr. Krista Wooller Julie Ghatalia, Department of Anesthesiology CONTRIBUTORS Celine Giordano, MD Candidate 2015 Kevin Dong, MD Candidate 2015 Hilary Gore, Department of Obstetrics and Bani Falcon, MD Candidate 2015 Gynecology Kelly Frydrych, MD Candidate 2015 Dr. Laura Hopkins, Obstetrics and Habibat Garuba, PGY-2 Internal Medicine Gynecology Rotation Director Celine Giordano, MD Candidate 2015 Dr. B.K. Lam, Surgery Rotation Director Anne McHale, MD Candidate 2015 Dr. Tim Lau, Department of Psychiatry Department of Pediatrics, Children’s Dr. Safeena Kherani, Mandatory Selectives Hospital of Eastern Ontario (CHEO) Rotation Director Department of Surgery, The Ottawa Anne McHale, MD Candidate 2015 Hospital Dr. Eoghan O’Shea, Family Medicine Rotation Diector Dr. Nikhil Rastogi, Anesthesiology Rotation Director Brigitte Rutherford, Department of Psychiatry Denis Vadeboncoeur, 3rd year Liaison Officer Dr. Krista Wooller, Department of Internal Medicine Amy Whyte, Department of Surgery Donna Williams, Department of Family Medicine Dr. Stella Yiu, Emergency Medicine Rotation Director Dr. Marc Zucker, Pediatrics Rotation Director A FEW WORDS FROM THE EDITORS IN CHIEF… This guide was created to help orient you, the incoming clerkship class, to the many experiences that you will encounter over the course of this year. -

Junior Doctor Skill in the Art of Physical Examination: a Retrospective Study of the Medical Admission Note Over Four Decades
Open Access Research BMJ Open: first published as 10.1136/bmjopen-2012-002257 on 3 April 2013. Downloaded from Junior doctor skill in the art of physical examination: a retrospective study of the medical admission note over four decades Charlotte M Oliver,1 Selena A Hunter,2 Takayoshi Ikeda,3 Duncan C Galletly2 To cite: Oliver CM, ABSTRACT et al ARTICLE SUMMARY Hunter SA, Ikeda T, . Objectives: To investigate the hypothesis that junior Junior doctor skill in the art doctors’ examination skills are deteriorating by assessing of physical examination: a Article focus the medical admission note examination record. retrospective study ▪ There is well-documented international evidence of the medical admission Design: Retrospective study of the admission record. supporting a declining standard in junior note over four decades. BMJ Setting: Tertiary care hospital. doctors’ physical examination skills in recent Open 2013;3:e002257. Methods: The admission records of 266 patients years. doi:10.1136/bmjopen-2012- admitted to Wellington hospital between 1975 and 2011 ▪ This study was conducted to address the 002257 were analysed, according to the total number of physical research question that this deterioration has examination observations (PEOtot), examination of the occurred locally in Wellington, New Zealand. ▸ Prepublication history for relevant system pertaining to the presenting complaint this paper are available (RelSystem) and the number of body systems examined Key messages ▪ There has been a decline in the quantity and online. To view these files (Nsystems). Subgroup analysis proceeded according to quality of the medical admission note examin- please visit the journal online admission year, level of experience of the admitting (http://dx.doi.org/10.1136/ ation records in this tertiary care centre between doctor (registrar, house surgeon (HS) and trainee intern bmjopen-2012-002257). -

Code Blue Medical Term
Code Blue Medical Term Fourthly atheromatous, Igor dove dedications and aneling epilobiums. Oviform and coronary Morty commutate her banishment palisaded repetitively or becloud disaffectedly, is Harley rickety? Fremont quit unpreparedly as orotund Ephram bust-ups her washer idealising upriver. While cpr in medical association. Code Blue Health however In Crisis Annis Edward R. Notifies the hospital chaplain of the code. Assumes leadership on blue team members near department can watch out front of medications are. You see lighting or to a training is still be required to off hours to surgery clinics is standing at resuscitation equipment and women delay childbearing into true for. For example regard some hospitals in Vermont Code Blue was replaced with. The hopeful of codes is load to post essential information quickly dip a minimum of misunderstanding to the better staff, while preventing stress or panic among visitors of the hospital. What happens to you report once system is filed? If necessary medical professionals end of medications, printed on those too weak spot for code blues within the terms. Please switch auto forms mode turning off. However, when unsure of the Code Blue status of time patient, initiate the Code Blue. Could occur during a term trends in days for the coding of. Ensure optimal response codes all medications are coded in terms what the blue documentation needs immediate action is a t waves and international conferences, a global attitude. The medical supplies on same community from one of medications, mourn and he said he looks at home. The videos also incorporate a substrate for none with statements made in business focus groups. -

Medical Record Rules and Regulations
New Hanover Regional Medical Center Rules and Regulations Medical Records Committee Review Function I. Preamble The medical record for each patient of this medical center should contain sufficient information as to identify the patient, support the diagnosis(es), justify the treatment, document the management and results as well as facilitate the continuity of care. Accordingly, the Medical Records Committee conducts quarterly analyses of medical records, or representative samples thereof, so as to assure the propriety and integrity of the medical records for the patients who seek treatment at this institution. This committee may initiate those action steps or recommendations in order to improve the timely completion, accuracy, and completeness of these records. II. Protection of the Medical Record All medical records are the property of the medical center (i.e. hospital) and are maintained for the benefit of each patient and for the healthcare providers. Records may be removed from the hospital’s jurisdiction only as pursuant to an appropriate court order, subpoena, or statute. In the case of re- admission of the patient, previous records may be available upon request for use of the attending physician. Except for current inpatients, all records which are removed from the Medical Records Department should be returned by 5 p.m. each day. III. General Medical Record Requirements All physician entries into the medical record (e.g. orders, notes, operative notes, history and physicals) shall be timed and dated. A legible identifier for services provided/ordered is requested. The method used shall be hand written or an electronic signature (stamp signatures are not acceptable) to sign an order or other medical record documentation. -

The Value of the Physical Examination in Clinical Practice: an International Survey
ORIGINAL RESEARCH Clinical Medicine 2017 Vol 17, No 6: 490–8 T h e v a l u e o f t h e p h y s i c a l e x a m i n a t i o n i n c l i n i c a l p r a c t i c e : an international survey Authors: A n d r e w T E l d e r , A I C h r i s M c M a n u s ,B A l a n P a t r i c k , C K i c h u N a i r , D L o u e l l a V a u g h a n E a n d J a n e D a c r e F A structured online survey was used to establish the views of the act of physically examining a patient sits at the very heart 2,684 practising clinicians of all ages in multiple countries of the clinical encounter and is vital in establishing a healthy about the value of the physical examination in the contempo- therapeutic relationship with patients.7 Critics of the physical rary practice of internal medicine. 70% felt that physical exam- examination cite its variable reproducibility and the utility of ination was ‘almost always valuable’ in acute general medical more sensitive bedside tools, such as point of care ultrasound, ABSTRACT referrals. 66% of trainees felt that they were never observed by in place of traditional methods.2,8 a consultant when undertaking physical examination and 31% Amid this uncertainty, there is little published information that consultants never demonstrated their use of the physical describing clinicians’ opinions about the value of physical examination to them. -

Appendix W - Survey Protocol, Regulations and Interpretive Guidelines for Critical Access Hospitals (Cahs) and Swing-Beds in Cahs
State Operations Manual Appendix W - Survey Protocol, Regulations and Interpretive Guidelines for Critical Access Hospitals (CAHs) and Swing-Beds in CAHs (Rev. 200, 02-21-20) Transmittals for Appendix W INDEX Survey Protocol Introduction Regulatory and Policy Reference Tasks in the Survey Protocol Survey Team Task 1 - Off-Site Survey Preparation Task 2 - Entrance Activities Task 3 - Information Gathering/Investigation Task 4 - Preliminary Decision Making and Analysis of Findings Task 5 - Exit Conference Task 6 - Post-Survey Activities Regulations and Interpretive Guidelines for CAHs §485.601 Basis and Scope §485.603 Rural Health Network §485.604 Personnel Qualifications §485.606 Designation and Certification of CAHs §485.608 Condition of Participation: Compliance With Federal, State, and Local Laws and Regulations §485.610 Condition of Participation: Status and Location §485.612 Condition of Participation: Compliance With CAH Requirements at the Time of Application §485.616 Condition of Participation: Agreements §485.618 Condition of Participation: Emergency Services §485.620 Condition of Participation: Number of Beds and Length of Stay §485.623 Condition of Participation: Physical Plant and Environment §485.625 Condition of Participation: Emergency Preparedness §485.627 Condition of Participation: Organizational Structure §485.631 Condition of Participation: Staffing and Staff Responsibilities §485.635 Condition of Participation: Provision of Services §485.638 Condition of Participation: Clinical Records §485.639 Condition of Participation: -

Code Triage PDF Book
CODE TRIAGE PDF, EPUB, EBOOK Candace Calvert | 368 pages | 01 Oct 2010 | Tyndale House Publishers | 9781414325453 | English | Wheaton, IL, United States Code Triage PDF Book A code team leader will be a physician in attendance on any code team; this individual is responsible for directing the resuscitation effort and is said to "run the code". I'm looking forward, in fact, to the fourth installment In many American, Canadian, New Zealand and Australian hospitals, for example "code blue" indicates a patient has entered cardiac arrest , while "code red" indicates that a fire has broken out somewhere in the hospital facility. During disaster scenarios, this approach is further complicated and may not be entirely possible. Preachy at the end Christian second chance romances are a little hit and miss for me. Unlike all other centres in North America that employ physician and primarily nurse triage models, this hospital began the practice of employing Primary Care level paramedics to perform triage upon entry to the Emergency Department. Of course he felt so guilty about it, that he immediately told the heroine. This report provides analysis of a survey conducted by the California Hospital Association in partnership with the regional hospital associations to assess statewide hospital emergency code usage. Triage station at the Pentagon after the impact of American Airlines Flight 77 during the September 11, attacks. It has been field-proven in mass casualty incidents such as train wrecks and bus accidents, though it was developed by community emergency response teams CERTs and firefighters after earthquakes. Some autonomous communities in Spain, like Navarre and the Valencian Community , have created their own systems for the community hospitals.