Behavioral Insomnia of Childhood
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Zimmerman Chair Bedroom
BRUNSWICK ZIMMERMAN BEDROOM BRUNSWICK 7314 7318 CHEST OF DRAWERS ARMOIRE 7331 LANDSCAPE MIRROR 7324 7326 DOUBLE DRESSER TRIPLE DRESSER 7314 CHEST OF DRAWERS 56" H X 38" W X 19" D 7315 LOW CHEST OF DRAWERS 27" H X 42" W X 25" D 7318 ARMOIRE 7315 77" H X 42" W X 25" D LOW CHEST OF DRAWERS 7324 DOUBLE DRESSER 36" H X 60" W X 19" D 7326 TRIPLE DRESSER 39" H X 72" W X 19" D 7330 VERTICAL MIRROR 36" H X 43" W X 2" D 7331 LANDSCAPE MIRROR 26" H X 48" W X 2" D 7350 BRUNSWICK PANEL BED Standard Headboard 52" H Standard Footboard 18" H 7350Q BRUNSWICK PANEL BED 7360 BRUNSWICK CANOPY BED Headboard 52" / 78" H Footboard 18" / 78" H 7331 LANDSCAPE MIRROR - See pricelist for complete bed and case options w/ specs and dimensions - All drawers are standard with full access undermount soft-close glides - All cases have interior frame construction with dust-proof panels between each drawer 7360Q -All Brunswick Beds have rails BRUNSWICK CANOPY BED with hidden bolt mount systems and wooden dovetail slats All beds are available in Twin(T), Full(F), Queen(Q), California King ( C ), King (K) BRUNSWICK 7301 NIGHT TABLE 31" H X 24" W X 15" D 7303 BEDSIDE CHEST 29" H X 28" W X 15" D 7301 7303 NIGHT TABLE BEDSIDE CHEST ZIMMERMAN BEDROOM BY WWW.ZIMMERMANCHAIR.COM FRANCESCA FRANCESCA 8251K Francesca Bed 8224 Double Dresser 8201 NIGHT STAND- 3 Drawers 32"H X 26"W X 18"D 8213 LINGERIE CHEST (not shown) 56"H x 26"W x 20"D 8214 CHEST OF DRAWERS 56"H x 40"W x 20"D 8224 DOUBLE DRESSER 38"H x 60"W x 20"D 8251K FRANCESCA BED Standard Headboard 55"H 8201 Standard Footboard -

Bed Bug Fact Sheet
BED BUGS September 2011 Bed bugs are found worldwide. In recent years, bed bugs have been making a comeback because of changing insect control practices, pesticide resistance and increased international travel. Travel spreads them because the bugs and their eggs are easily transported in luggage, clothing, bedding, and furniture. Quick facts o Bed bugs are fast moving insects that eat mostly at night when their host is asleep. o Prefer human blood but will feed on chickens, mice, and rabbits, too. o They feed on any area of exposed skin, such as the face, neck, shoulders, arms or hands. o The bites don’t hurt, so the person usually doesn’t know that he/she has been bitten, but bed bug bites do irritate the skin. o Depending on availability of food and temperature (70-82F is optimal); it takes 5 weeks to 4 months for the maturation of a bed bug from egg to adult. o They can go 80 to 140 days without a meal. o Adults live about 10 months. Do bed bugs spread disease? o Bed bugs are not known to transmit disease; however, they can cause physical and mental stress. o A reaction to the bites can take 1– 14 days to develop, and some people have no reaction. o Bed bug bites look like mosquito, flea, and spider bites. The only way to confirm the bite is from a bed bug is to find evidence of the bugs in your bed/bedroom. What do bed bugs look like? o Adult bed bugs are oval shaped, wingless, 1/3 inch long, rusty red or mahogany color, and shaped like an apple seed. -

Contemporary DIY Four Poster Bed
Contemporary DIY Four Poster Bed Here are a few housekeeping items before you start that will make this project even easier to tackle. First, this bed needs to be assembled in the space in the bedroom it will be in. The assembled parts are larger than a doorway. I stained and waxed my wood pieces before assembling. Since the wood was already finished, I placed a heavy moving blanket on the floor to protect the wood from scratches. Time to complete: 2-3 days Lumber: 2 - 1” x 2” x 8ft poplar 16 - 1” x 3” x 6ft poplar 2 – 2” x 2” x 6ft poplar 6 - 1” x 6” x 6ft maple 3 – 2” x 2” x8ft maple 2 – 2” x 3” x 8ft maple 2 – 2” x 6” x 6ft maple 4 – 3” x 3” x 8ft maple Materials: Pocket screws 1 ¼ Pocket screws 2 ” Wood screws 1 ¼ ” Wood screws 1 ½ “ Wood glue Sand paper Stain or paint to finish Cut List: Maple 4 - 3” x 3” at 78 ¾” bed posts 2 - 2” x 2” at 60 ½“ top rails 2 - 2” x 6” at 60 ½” footboard and lower headboard planks 6 – 1” x 6” at 60 ½” headboard planks 2 – 2” x 2” at 80 ½” upper rails 2 – 2” x 4” at 80 ½” lower side rails Poplar 2 – 1’ x 2’ at 80 ½” slat cleat 1 – 2’ x 2’ at 80 ½” center support 1 – 2” x 2” at 9 ¼” center support legs 16 – 1” x 3” at 60 ½” slats Preparation Cut, sand and finish all of the maple pieces. -

Hearts Bed with 4 Poster Frame
Hearts Bed With 4 Poster Frame Assembly Instructions - Please keep for future reference 323/8130 333/9613 Dimensions Width - 197cm Depth - 94cm Height - 189cm Important - Please read these instructions fully before starting assembly If you need help or have damaged or missing parts, call the Customer Helpline: Argos = 0345 640 0800 Issue 1 - 08//10/14 Safety and Care Advice Important - Please read these instructions fully before starting assembly • Keep children and animals • We do not IMPORTANT! away from the work area, small recommend the KEEP FOR parts could choke if swallowed. use of power drill/drivers for • Make sure you have enough FUTURE inserting screws, space to layout the parts before as this could damage the unit. REFERENCE starting. Only use hand screwdrivers. • Check you have all the • During assembly do not stand • Assemble on a soft level components and tools listed on or put weight on the product, this surface to avoid damaging the the following pages. could cause damage. unit or your floor. • Remove all fittings from the • Assemble the item as close to • Parts of the assembly will be plastic bags and separate them its final position (in the same easier with 2 people. into their groups. room) as possible. • Unit weight: 20.4 kgs. Care and maintenance • Only clean using a damp cloth • From time to time check that • This product should not be and mild detergent, do no use there are no loose screws on discarded with household bleach or abrasive cleaners. this unit. waste. Take to your local authority waste disposal centre. Warnings • Regularly check and ensure • Prohibit your children from • Do not use this child’s bed if that all bolts and fittings are bouncing and jumping on the any part is broken, torn or tightened properly. -

Behavioral Treatment of Bedtime Problems and Night Wakings In
PEDIATRIC SLEEP Behavioral Treatment of Bedtime Problems and Night Wakings in Infants and Closer to our Customers… Young Children (but don’t just take our word for it.) An American Academy of Sleep Medicine Review Jodi A. Mindell, PhD1,4; Brett Kuhn, PhD2; Daniel S. Lewin, PhD3; Lisa J. Meltzer, PhD4; Avi Sadeh, DSc5 1Department of Psychology, Saint Joseph’s University, Philadelphia, PA; 2University of Nebraska Medical Center, Omaha, NE; 3Children’s National ” Our relationship with Embla, formerly Medcare, has been “ The Xactrace Belts are the best Medical Center, George Washington University School of Medicine, Washington, DC; 4Children’s Hospital of Pennsylvania, Philadelphia, PA; 5Depart- mutually beneficial both educationally and professionally. way to measure breathing effort ment of Psychology, Tel Aviv University, Tel Aviv, Israel Every piece of our future 30 bed facility will be networked and are smoothly interfaced with Abstract: This paper reviews the evidence regarding the effi cacy of be- tinction and preventive parent education. In addition, support is provided together and they have helped us towards our pending 1st the Rembrandt Sleep system”. havioral treatments for bedtime problems and night wakings in young for graduated extinction, bedtime fading/positive routines, and scheduled CoA PSG Accredited sleep program”. – Andy Desrosiers, Holy – Jim Wilcox, RPSGT/CRT, children. It is based on a review of 52 treatment studies by a task force awakenings. Additional research is needed to examine delivery methods of treatment, longer-term effi cacy, and the role of pharmacological agents. Family Hospital , Massachusetts, USA All Children’s Hospital, appointed by the American Academy of Sleep Medicine to develop prac- tice parameters on behavioral treatments for the clinical management of Furthermore, pediatric sleep researchers are strongly encouraged to de- St. -
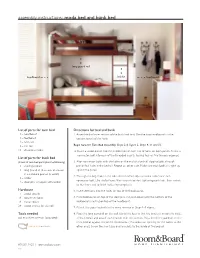
Assembly Instructions: Moda Bed and Bunk Bed
assembly instructions: moda bed and bunk bed long guard rail headboard ladder footboard List of parts for twin bed Directions for bed and bunk 1 – headboard 1. Assemble the lower section of the bunk bed first. Use the two headboards as the 1 – footboard bottom panels of the bunk. 2 – bed rails 1 – slat roll Begin here for Twin Bed Assembly. Steps 2-4, Figure 2, Steps 9, 11 and 12. 18 – decorative bolts 2. Insert a wood dowel into the middle hole of each trio of holes on both panels. Screw a connector bolt into each of the threaded inserts, leaving four or five threads exposed. List of parts for bunk bed ( 2 sets of twin bed parts plus the following) 3. Align connector bolts with the holes on the end of a bedrail, slipping bolts through 1 – short guardrail pre-drilled holes in the bedrail. Repeat on other side. Make sure each bedrail is tight up 1 – long guardrail (4 screws enclosed against the panel. in cardboard pad on bracket) 4. Through the large hole in the side of the bedrail, slip one metal collar over each 1 – ladder connector bolt. Use the ball end Allen wrench to start tightening each bolt, then switch 4 – steel pins wrapped with ladder to the short end to finish tightening completely. Hardware 5. Insert steel pins into the holes on top of the headboards. 4 – wood dowels 8 – connector bolts 6. Place footboards on top of the steel pins and push down until the bottom of the 8 – metal collars footboard is resting on top of the headboard. -
General Information About Bed Bugs
General Information About Bed Bugs Bed bugs have become a nuisance pest in some households and some public lodging facilities in the City of Holland. These bugs are not currently regulated by health agencies because they do not carry or spread disease*. However, bed bugs can be transmitted between households on used furniture, clothing, bedding, toys and personal items. Section 14-4.10 of the City of Holland Ordinance Code states in part: Interior structure. Pest control. The interior of all structures shall be kept free of circumstances that may harbor an infestation of insects or rodents. Infestations, when found, shall be promptly treated for the elimination thereof by a treatment program approved by the enforcing officer. Regular treatments shall continue until the infestation is eliminated. If the treatment program proves ineffective within a reasonable period of time, the enforcing officer may require the use of a more effective treatment program. After the infestation is eliminated, proper precautions shall be taken to prevent reinfestation. Many insect and rodent infestations begin, or worsen, because of poor housekeeping, lack of sanitation and unclean living conditions. This is not the case for bed bugs. Cleanliness, sanitation and housekeeping are not indicators for this pest. Bed bugs can be brought into a home on clothing, in suitcases, in purses and especially on used furniture and used mattresses. Bed bugs can also travel between apartments in a building or between rooms in a hotel. Bed bugs are lazy insects, and do not usually wander very far from their food source. Bed bugs only come out at night, and bite exposed areas of the body – areas that are not covered with clothing such as arms, legs and your back. -

A Case of Sick Sinus Syndrome Presenting As Exploding Head Syndrome
CASE REPORT online © ML Comm J Korean Sleep Res Soc 2012;9:61-63 ISSN 1738-608X A Case of Sick Sinus Syndrome Presenting as Exploding Head Syndrome Hye Yun Kim, Do Young Yoon, Dong Sun Kim, Ji Sun Kwon and Hyun Jeong Han Department of Neurology, Myongji Hospital, Kwandong University College of Medicine, Goyang, Korea Received December 3, 2012 Exploding head syndrome (EHS) is a rare syndrome experienced with explosive noise happening in a head. Revised December 24, 2012 A 78 year old man visited for intractable headache with explosive noises. His vieo-electroencephalography Accepted December 24, 2012 monitoring showed tachy-brady arrhythmia on electrocardiogram. We diagnosed as a sick sinus syndrome Address for correspondence (SSS) presented with EHS. We suggest SSS should be considered with the elderly patients who have EHS Hyun Jeong Han, MD, PhD Department of Neurology, symptom. Myongji Hospital, Kwandong J Korean Sleep Res Soc 2012;9:61-63 University College of Medicine, 697-24 Hawjeong-dong, Key Words: Sick sinus syndrome, Headache. Deogyang-gu, Goyang 412-270, Korea Tel: +82-31-810-5403 Fax: +82-31-969-0500 E-mail: [email protected] Exploding head syndrome (EHS), which is a rare primary night before bed time. headache syndrome is characterized with explosive noise hap- His blood pressure was 130/75 mm Hg and there was not sig- pening in a head.1 EHS was first described as the syndrome of nificant finding on results of routine serologic and cardiologic ‘snapping of the brain,’ by Armstron-Jones in 1920. In 1988, studies including electrocardiogram (ECG). -

Behavioral and Psychological Treatments for Chronic Insomnia Disorder in Adults: an American Academy of Sleep Medicine Clinical Practice Guideline Jack D
https://doi.org/10.5664/jcsm.8986 SPECIAL ARTICLES Behavioral and psychological treatments for chronic insomnia disorder in adults: an American Academy of Sleep Medicine clinical practice guideline Jack D. Edinger, PhD1,2;J.ToddArnedt,PhD3; Suzanne M. Bertisch, MD, MPH4; Colleen E. Carney, PhD5; John J. Harrington, MD, MPH6; Kenneth L. Lichstein, PhD7; Michael J. Sateia, MD, FAASM8; Wendy M. Troxel, PhD9;EricS.Zhou,PhD10;UzmaKazmi,MPH11; Jonathan L. Heald, MA11; Jennifer L. Martin, PhD12,13 1National Jewish Health, Denver, Colorado; 2Duke University Medical Center, Durham, North Carolina; 3Michigan Medicine, University of Michigan, Ann Arbor, Michigan; 4Brigham and Women’s Hospital, Harvard Medical School, Boston, Massachusetts; 5Ryerson University,Toronto, California; 6University of Nebraska Medical Center, Omaha, Nebraska; 7University ofAlabama,Tuscaloosa, Alabama; 8Geisel School of Medicine at Dartmouth, Hanover, New Hampshire; 9RAND Corporation, Pittsburgh, Pennsylvania; 10Harvard Medical School, Dana- Farber Cancer Institute, Boston Children’s Hospital, Boston, Massachusetts; 11American Academy of Sleep Medicine, Darien, Illinois; 12DavidGeffenSchoolofMedicineattheUniversity of California Los Angeles, Los Angeles, California; 13VA Greater Los Angeles Healthcare System, Geriatric Research, Education and Clinical Center, Los Angeles, California Introduction: This guideline establishes clinical practice recommendations for the use of behavioral and psychological treatments for chronic insomnia disorder in adults. Methods: The American -

Duvet Covers • Bed Skirts • Pillows Fabrics from Left: 28709-123, T30453-16, W3001-123, 28645-123, 28711-116 Table of Contents
kravetbedding Duvet Covers • Bed Skirts • Pillows Fabrics from left: 28709-123, T30453-16, W3001-123, 28645-123, 28711-116 Table of Contents Duvet Covers .................................1 Bed Skirts ....................................9 Pillows .....................................17 Pillows: 27750-21, 28902-16 Terms and Conditions of Sale Policies • It is the purchaser’s responsibility to ensure they are ordering the correct style, color, dimensions and options. • Prices are net and are subject to change without notice. • Quotes are honored for 30 days. Graded-In Fabrics and Trimmings • The kravetbedding graded-in fabric offering contains thousands of Kravet and Lee Jofa fabrics and trimmings. Leathers and suedes sold by the hide are not graded into kravetbedding. • No C.O.M. fabrics and trimmings will be accepted by kravetbedding. Terms of Payment • Prepayment is required when placing a kravetbedding order. • C.O.D. orders are not accepted. Production • Orders will not go into production until payment is collected and all fabrics and trimmings are received at the workroom. Shipping • Orders will be shipped complete via UPS Ground Service unless otherwise specified. • Kravetbedding is not responsible for delivery delays due to causes beyond our control. Cancellations • No cancellations are allowed once fabric for the order has been cut. • Phone cancellations will not be honored. • A written notice of cancellation must be received. Claims • If your product is damaged, please contact kravetbedding immediately. • Claims must be made within 14 days from delivery date. • Keep original packaging and cartons. • If applicable, a photograph of the damaged product may be requested. • If appropriate, merchandise claimed to be defective may be inspected by an authorized repair professional in your area. -

Proper Disposal of Bed Bug Infested Household Items
The New York City Department of Health and Mental Hygiene PROPER DISPOSAL OF BED BUG INFESTED HOUSEHOLD ITEMS If you have bed bugs, have your home inspected and treated by a pest management professional before you decide to dispose of anything. (See Preventing and Getting Rid of Bed Bugs Safely). Most times, clothing, bedding and furniture from a home with a bed bug problem can be treated and do not need to be thrown away. If you decide to dispose of items, they should be carefully sealed in a plastic bag or container first so the bed bugs don’t spread. SEALING HOUSEHOLD GOODS FOR DISPOSAL • Items should be enclosed in heavy-duty plastic sheeting or plastic bags before removing them. • All plastic bags and sheeting should be taped so there are no openings. Use duct or box tape. • Carefully handle all sealed infested items when disposing of them to prevent damage to the wrapping. • If possible, place the infested items in a secure garbage container that seals tightly so that bedbugs can’t escape. DISPOSAL OF SEALED ITEMS ¾ SMALLER ITEMS • Place small items such as clothes, bed linens, toys, throw rugs, shoes and other personal belongings in a heavy-duty trash bag and use tape to seal the bag so that bedbugs can’t escape. • Attach a sign on the bags clearly stating, “BED BUG INFESTED - DO NOT TAKE” to discourage other people from taking infested items to their homes. • Infested items to be discarded should be placed on the street curb close to the time they will be collected by the Sanitation Department. -

Periodic Limb Movement Disorder: Characteristics
SLEEP SCIENCE : SLEEP , SLEEPINESS , AND SLEEPLESSNESS Kenneth Lichstein, Ph.D. Professor Emeritus Department of Psychology The University of Alabama sleeplessness II a lot can go wrong topics (among 70 sleep disorders) sleep apnea narcolepsy restless legs periodic limb movements disorders we won’t talk about exploding head syndrome sexsomnia sleep-related epilepsy catathrenia if left untreated, sleep apnea is a slow moving terminal illness Pickwickian syndrome (now called obesity-hypoventilation syndrome) obesity, daytime labored breathing, daytime sleepiness ̶ Burwell et al., 1956 10 years later sleep apnea “Nocturnal polygraphic registrations disclosed respiratory pauses…” ̶ Gastaut et al., 1966 invisible sleep apnea science advances by two processes ❑ steady, incremental, systematic research ❑ abrupt, accidental discovery o Between 1956 and 1966, 10s of thousands of PSGs had been performed world wide and no one noticed some people had quit breathing. o Bed partners were not complaining that their partner had quit breathing. when you don’t know what you are looking for, you don’t see the obvious benign snoring and sleep apnea moderate and severe snoring sleep apnea benign snoring I snoring without breath cessation ▪ occurs in 10-15% of population ▪ sleeping on back increases likelihood of snoring ▪ snorer usually has no knowledge of condition ▪ more troublesome to bed partner ▪ at 5-year follow-up, benign snoring (without weight gain) is not a risk factor for sleep apnea physiology ▪ partial airway obstruction ▪ on continuum