Lymphatic Filariasis Elimination Program Annual Report (2017/18)
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

SECOND KATHMANDU VALLEY WATER SUPPLY IMPROVEMENT PROJECT Procurement Workshop Kathmandu, 10 February 2021 Kathmandu – Demography
SECOND KATHMANDU VALLEY WATER SUPPLY IMPROVEMENT PROJECT Procurement Workshop Kathmandu, 10 February 2021 Kathmandu – Demography • Population ~ 3 million; floating population ~1.2 million • Average household size – 4.2 persons • 575 sq.km Valley Area • 18 municipalities, 3 districts (Kathmandu, Bhaktapur, and Lalitpur) • Bell shaped valley with elevation varying from 1400m at periphery – 1280m • About 500 hotels; 44000 beds; Average 5000 tourists per day SKVWSIP – Institutional Arrangements Institution SKVWSIP Implementation Structure MWS Executing Agency Project Implementation Directorate – KUKL Implementing Agency – Distribution network (PID-KUKL) and House service connections Melamchi Water Supply Development Board Implementing Agency – Bulk water (MWSDB) infrastructure SKVWSIP – Project Area WTP & DNI COVERAGE AREA SUNDARIJAL WTP JORPATI N JORPATI S CHABAHIL GOTATHAR PEPSICOLA KIRTIPUR THIMMI BHAKTAPUR SKVWSIP – Overview & Timeline • Total estimated project cost – $230 million • Project area: Greenfield development outside Ring Road in Kathmandu Valley • Limited public water supply network; reliance on KUKL tankers, borewells, hand pumps, traditional water sources and private tankers • Beneficiaries: About 110,000 households Aspects Arrangements Commencement of procurement First half of 2021 Implementation period January 2022 – December 2028 Completion date December 2028 SKVWSIP – Procurement Packages Scope Indicative number of contracts WTP (255 MLD) 1 Distribution network (about 700 km total) 3–4 Structural retrofitting of Headwork structure of Melamchi water 1 diversion IT-based decision support system for O&M of Melamchi Tunnel 1 IT-based early warning system for Melamchi Headworks 1 Capacity building of KUKL to strengthen operational and technical 2 competencies Project Consultants 2 Proposed Distribution Network Packages under Second Kathmandu Valley Water Supply Improvement Project Procurement Workshopt Presentation to Prospective Bidders for New DNI packages (DNI-8, 9 & 10) PID-KUKL Feb 2021 Location of DNI Packages Outside Ring Road (DNI pkg. -

Tables Table 1.3.2 Typical Geological Sections
Tables Table 1.3.2 Typical Geological Sections - T 1 - Table 2.3.3 Actual ID No. List of Municipal Wards and VDC Sr. No. ID-No. District Name Sr. No. ID-No. District Name Sr. No. ID-No. District Name 1 11011 Kathmandu Kathmandu Ward No.1 73 10191 Kathmandu Gagalphedi 145 20131 Lalitpur Harisiddhi 2 11021 Kathmandu Kathmandu Ward No.2 74 10201 Kathmandu Gokarneshwar 146 20141 Lalitpur Imadol 3 11031 Kathmandu Kathmandu Ward No.3 75 10211 Kathmandu Goldhunga 147 20151 Lalitpur Jharuwarasi 4 11041 Kathmandu Kathmandu Ward No.4 76 10221 Kathmandu Gongabu 148 20161 Lalitpur Khokana 5 11051 Kathmandu Kathmandu Ward No.5 77 10231 Kathmandu Gothatar 149 20171 Lalitpur Lamatar 6 11061 Kathmandu Kathmandu Ward No.6 78 10241 Kathmandu Ichankhu Narayan 150 20181 Lalitpur Lele 7 11071 Kathmandu Kathmandu Ward No.7 79 10251 Kathmandu Indrayani 151 20191 Lalitpur Lubhu 8 11081 Kathmandu Kathmandu Ward No.8 80 10261 Kathmandu Jhor Mahakal 152 20201 Lalitpur Nallu 9 11091 Kathmandu Kathmandu Ward No.9 81 10271 Kathmandu Jitpurphedi 153 20211 Lalitpur Sainbu 10 11101 Kathmandu Kathmandu Ward No.10 82 10281 Kathmandu Jorpati 154 20221 Lalitpur Siddhipur 11 11111 Kathmandu Kathmandu Ward No.11 83 10291 Kathmandu Kabresthali 155 20231 Lalitpur Sunakothi 12 11121 Kathmandu Kathmandu Ward No.12 84 10301 Kathmandu Kapan 156 20241 Lalitpur Thaiba 13 11131 Kathmandu Kathmandu Ward No.13 85 10311 Kathmandu Khadka Bhadrakali 157 20251 Lalitpur Thecho 14 11141 Kathmandu Kathmandu Ward No.14 86 10321 Kathmandu Lapsephedi 158 20261 Lalitpur Tikathali 15 11151 Kathmandu -

Food Insecurity and Undernutrition in Nepal
SMALL AREA ESTIMATION OF FOOD INSECURITY AND UNDERNUTRITION IN NEPAL GOVERNMENT OF NEPAL National Planning Commission Secretariat Central Bureau of Statistics SMALL AREA ESTIMATION OF FOOD INSECURITY AND UNDERNUTRITION IN NEPAL GOVERNMENT OF NEPAL National Planning Commission Secretariat Central Bureau of Statistics Acknowledgements The completion of both this and the earlier feasibility report follows extensive consultation with the National Planning Commission, Central Bureau of Statistics (CBS), World Food Programme (WFP), UNICEF, World Bank, and New ERA, together with members of the Statistics and Evidence for Policy, Planning and Results (SEPPR) working group from the International Development Partners Group (IDPG) and made up of people from Asian Development Bank (ADB), Department for International Development (DFID), United Nations Development Programme (UNDP), UNICEF and United States Agency for International Development (USAID), WFP, and the World Bank. WFP, UNICEF and the World Bank commissioned this research. The statistical analysis has been undertaken by Professor Stephen Haslett, Systemetrics Research Associates and Institute of Fundamental Sciences, Massey University, New Zealand and Associate Prof Geoffrey Jones, Dr. Maris Isidro and Alison Sefton of the Institute of Fundamental Sciences - Statistics, Massey University, New Zealand. We gratefully acknowledge the considerable assistance provided at all stages by the Central Bureau of Statistics. Special thanks to Bikash Bista, Rudra Suwal, Dilli Raj Joshi, Devendra Karanjit, Bed Dhakal, Lok Khatri and Pushpa Raj Paudel. See Appendix E for the full list of people consulted. First published: December 2014 Design and processed by: Print Communication, 4241355 ISBN: 978-9937-3000-976 Suggested citation: Haslett, S., Jones, G., Isidro, M., and Sefton, A. (2014) Small Area Estimation of Food Insecurity and Undernutrition in Nepal, Central Bureau of Statistics, National Planning Commissions Secretariat, World Food Programme, UNICEF and World Bank, Kathmandu, Nepal, December 2014. -

Of Hetauda-Dhalkebar-Duhabi 400 Kv TL
Updated Resettlement Action Plan (RAP) of Hetauda-Dhalkebar-Duhabi 400 kV TL Submitted To: Nepal India Electricity Transmission and Trade Project Hetauda-Dhalkebar-Duhabi 400 kV Transmission Line Nepal Electricity Authority Kharipati, Bhaktapur Prepared And Submitted By: Environment and Social Studies Department Engineering Services Directorate Nepal Electricity Authority Kharipati, Bhaktapur May, 2017 Updated Resettlemention Action Plan i ABBREVIATIONS CBO Community Based Organization CDO Chief District Officer CDC Compensation Determination Committee CFUG Community Forest User Group DADO District Agriculture Development Office DDC District Development Committee DFO District Forest Office DHO District Health Office EIA Environmental Impact Assessment EMF Electromagnetic Fields ESMF Environmental and Social Management Framework ESSD Environment and Social Studies Department FGD Focus Group Discussion GON Government of Nepal HEP Hydro Electric Project HH Household HDD-ESMU Hetauda-Dhalkebar-Duhabi Environnent & Social Mgmt. Unit INPS Integrated Nepal Power System IPP Independent Power Producers IRPA International Radiation Protection Association KIIs Key Informant Interviews km Kilometer kV Kilovolt LCF Local Consultative Forum LDO Local Development Officer LARU Land Acquisition and Rehabilitation Unit NEA Nepal Electricity Authority NRs. Nepalese Rupees NGO Non Governmental Organization PAF Project Affected Family PAP Project Affected Person PCU Program Coordination Unit PRA Participatory Rapid Appraisal RAP Resettlement Action Plan ROW -

Program Areas/Program Elements: A06/A025, A08/A036, A06/A026, A08/A025, A08/A036, A18/A074 Submitted To
SAJHEDARI BIKAAS PROGRAM Quarterly Conflict Assessment (November 2013) Produced by Pact (Contract No: AID-367-C-13-00003) Program Areas/Program Elements: A06/A025, A08/A036, A06/A026, A08/A025, A08/A036, A18/A074 Submitted to THE DEMOCRACY AND GOVERNANCE OFFICE THE UNITED STATES AGENCY FOR INTERNATIONAL DEVELOPMENT (USAID) NEPAL MISSION Maharajgunj, Kathmandu, Nepal Submitted to USAID November, 2013 Contracting Officer Represenative Meghan T. Nalbo Submitted to the DEC by Nick Langton, Chief of Party, Sajhedari Bikaas Program PACT Inc. Nepal Sushma Niwas, Sallaghari, Bansbari, House No 589 Budhanilkantha Sadad, Kathmandu, Ward No 3 Post Box No. 24200, Kathmandu, Nepal This report was produced and converted to pdf format using Microsoft Word 2010. The images included in the report are jpg files. The language of the document is English. Sajhedari Bikaas Project Partnership for Local Development Quarterly Conflict Assessment (November 2013) An initial perception assessment of conflicts, tensions and insecurity in Sajhedari Bikaas project districts in Nepal’s Far West and Mid-West regions. Sajhedari Bikaas Project Partnership for Local Development Quarterly Conflict Assessment A initial perception assessment of conflicts, tensions and insecurity in Sajhedari Bikaas project districts in Nepal’s Far West and Mid-West regions (November 2013) Prepared by Saferworld for the Sajhedari Bikaas Project (Under Contract no. AID-367-C-13-00003) This study/assessment is made possible by the generous support of the American people through the United States Agency for International Development (USAID). The contents are the responsibility of Saferworld and do not necessarily reflect the views of USAID or the United States Government. Introduction Sajhedari Bikaas Project is a USAID-funded 5-year project aimed at empowering communities to direct their own development. -

Resettlement Action Plan (RAP) of Hetauda-Dhalkebar-Duhabi 400 Kv and Dhalkebar-Bhittamod 400 Kv TL Project
Resettlement Action Plan (RAP) of Hetauda-Dhalkebar-Duhabi 400 Public Disclosure Authorized kV And Dhalkebar-Bhittamod 400 kV TL Project (Angle Tower, Sub-stations and Structures) Public Disclosure Authorized Prepared And Submitted By: Public Disclosure Authorized Environment And Social Studies Department Engineering Services Nepal Electricity Authority Kharipati, Bhaktapur February, 2011 Public Disclosure Authorized Resettlemention Action Plan ABBREVIATIONS CBO Community Based Organization CDO Chief District Officer CDC Compensation Determination Committee CFUG Community Forest User Group DADO District Agriculture Development Office DDC District Development Committee DFO District Forest Office DHO District Health Office EIA Environmental Impact Assessment EMF Electromagnetic Fields ESMF Environmental and Social Management Framework ESSD Environment and Social Studies Department FGD Focus Group Discussion GON Government of Nepal HEP Hydro Electric Project HH Household HDD~ESMU Hetauda-D.halkebar-Duhabi Environnent & Social Mgmt. Unit INPS Integrated Nepal Power System IPP Independent Power Producers IRPA International Radiation Protection Association KlIs Key Informant Interviews km Kilometer kV Kilovolt LCF Local Consultative Forum LDO Local Development Officer LARU Land Acquisition and Rehabilitation Unit NEA Nepal Electricity Authority NRs. Nepalese Rupees NGO Non Governmental Organization PAF Project Affected Family PAP Project Affected Person PCU Program Coordination Unit PRA Participatory Rapid Appraisal RAP Resettlement Action -

Japan International Cooperation Agency (JICA)
Chapter 3 Project Evaluation and Recommendations 3-1 Project Effect It is appropriate to implement the Project under Japan's Grant Aid Assistance, because the Project will have the following effects: (1) Direct Effects 1) Improvement of Educational Environment By replacing deteriorated classrooms, which are danger in structure, with rainwater leakage, and/or insufficient natural lighting and ventilation, with new ones of better quality, the Project will contribute to improving the education environment, which will be effective for improving internal efficiency. Furthermore, provision of toilets and water-supply facilities will greatly encourage the attendance of female teachers and students. Present(※) After Project Completion Usable classrooms in Target Districts 19,177 classrooms 21,707 classrooms Number of Students accommodated in the 709,410 students 835,820 students usable classrooms ※ Including the classrooms to be constructed under BPEP-II by July 2004 2) Improvement of Teacher Training Environment By constructing exclusive facilities for Resource Centres, the Project will contribute to activating teacher training and information-sharing, which will lead to improved quality of education. (2) Indirect Effects 1) Enhancement of Community Participation to Education Community participation in overall primary school management activities will be enhanced through participation in this construction project and by receiving guidance on various educational matters from the government. 91 3-2 Recommendations For the effective implementation of the project, it is recommended that HMG of Nepal take the following actions: 1) Coordination with other donors As and when necessary for the effective implementation of the Project, the DOE should ensure effective coordination with the CIP donors in terms of the CIP components including the allocation of target districts. -

Human–Tiger Panthera Tigris Conflict and Its Perception in Bardia National Park, Nepal
Human–tiger Panthera tigris conflict and its perception in Bardia National Park, Nepal B ABU R. BHATTARAI and K LAUS F ISCHER Abstract Human–wildlife conflict is a significant problem Wang & Macdonald, 2006). An increase in the human that often results in retaliatory killing of predators. Such population has resulted in increased incidence of conflict conflict is particularly pronounced between humans and between people and carnivores (Graham et al., 2005; tigers Panthera tigris because of fatal attacks by tigers on Woodroffe et al., 2005a). This often results in retaliatory humans. We investigated the incidence and perception of persecution, which is a significant threat to large carnivores human–tiger conflict in the buffer zone of Bardia National (Mishra et al., 2003; Treves & Karanth, 2003; Nyhus & Park, Nepal, by interviewing 273 local householders and Tilson, 2004). Thus, conservation measures to protect large 27 key persons (e.g. representatives of local communities, carnivores can be controversial and may lack support Park officials). Further information was compiled from from local communities (Graham et al., 2005). the Park’s archives. The annual loss of livestock attributable Large carnivores play a significant role in ecosystem to tigers was 0.26 animals per household, amounting to an functioning, with their absence inducing changes in annual loss of 2% of livestock. Livestock predation rates were predator–prey relationships and inter-specific competition particularly high in areas with low abundance of natural (Treves & Karanth, 2003). Many carnivores serve as prey. During 1994–2007 12 people were killed and a further important umbrella and flagship species, benefiting other four injured in tiger attacks. -

Strengthening the Role of Civil Society and Women in Democracy And
HARIYO BAN PROGRAM Monitoring and Evaluation Plan 25 November 2011 – 25 August 2016 (Cooperative Agreement No: AID-367-A-11-00003) Submitted to: UNITED STATES AGENCY FOR INTERNATIONAL DEVELOPMENT NEPAL MISSION Maharajgunj, Kathmandu, Nepal Submitted by: WWF in partnership with CARE, FECOFUN and NTNC P.O. Box 7660, Baluwatar, Kathmandu, Nepal First approved on April 18, 2013 Updated and approved on January 5, 2015 Updated and approved on July 31, 2015 Updated and approved on August 31, 2015 Updated and approved on January 19, 2016 January 19, 2016 Ms. Judy Oglethorpe Chief of Party, Hariyo Ban Program WWF Nepal Baluwatar, Kathmandu Subject: Approval for revised M&E Plan for the Hariyo Ban Program Reference: Cooperative Agreement # 367-A-11-00003 Dear Judy, This letter is in response to the updated Monitoring and Evaluation Plan (M&E Plan) for the Hariyo Program that you submitted to me on January 14, 2016. I would like to thank WWF and all consortium partners (CARE, NTNC, and FECOFUN) for submitting the updated M&E Plan. The revised M&E Plan is consistent with the approved Annual Work Plan and the Program Description of the Cooperative Agreement (CA). This updated M&E has added/revised/updated targets to systematically align additional earthquake recovery funding added into the award through 8th modification of Hariyo Ban award to WWF to address very unexpected and burning issues, primarily in four Hariyo Ban program districts (Gorkha, Dhading, Rasuwa and Nuwakot) and partly in other districts, due to recent earthquake and associated climatic/environmental challenges. This updated M&E Plan, including its added/revised/updated indicators and targets, will have very good programmatic meaning for the program’s overall performance monitoring process in the future. -
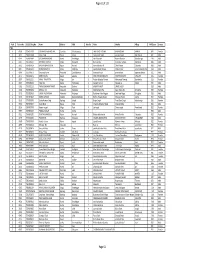
TSLC PMT Result
Page 62 of 132 Rank Token No SLC/SEE Reg No Name District Palika WardNo Father Mother Village PMTScore Gender TSLC 1 42060 7574O15075 SOBHA BOHARA BOHARA Darchula Rithachaupata 3 HARI SINGH BOHARA BIMA BOHARA AMKUR 890.1 Female 2 39231 7569013048 Sanju Singh Bajura Gotree 9 Gyanendra Singh Jansara Singh Manikanda 902.7 Male 3 40574 7559004049 LOGAJAN BHANDARI Humla ShreeNagar 1 Hari Bhandari Amani Bhandari Bhandari gau 907 Male 4 40374 6560016016 DHANRAJ TAMATA Mugu Dhainakot 8 Bali Tamata Puni kala Tamata Dalitbada 908.2 Male 5 36515 7569004014 BHUVAN BAHADUR BK Bajura Martadi 3 Karna bahadur bk Dhauli lawar Chaurata 908.5 Male 6 43877 6960005019 NANDA SINGH B K Mugu Kotdanda 9 Jaya bahadur tiruwa Muga tiruwa Luee kotdanda mugu 910.4 Male 7 40945 7535076072 Saroj raut kurmi Rautahat GarudaBairiya 7 biswanath raut pramila devi pipariya dostiya 911.3 Male 8 42712 7569023079 NISHA BUDHa Bajura Sappata 6 GAN BAHADUR BUDHA AABHARI BUDHA CHUDARI 911.4 Female 9 35970 7260012119 RAMU TAMATATA Mugu Seri 5 Padam Bahadur Tamata Manamata Tamata Bamkanda 912.6 Female 10 36673 7375025003 Akbar Od Baitadi Pancheswor 3 Ganesh ram od Kalawati od Kalauti 915.4 Male 11 40529 7335011133 PRAMOD KUMAR PANDIT Rautahat Dharhari 5 MISHRI PANDIT URMILA DEVI 915.8 Male 12 42683 7525055002 BIMALA RAI Nuwakot Madanpur 4 Man Bahadur Rai Gauri Maya Rai Ghodghad 915.9 Female 13 42758 7525055016 SABIN AALE MAGAR Nuwakot Madanpur 4 Raj Kumar Aale Magqar Devi Aale Magar Ghodghad 915.9 Male 14 42459 7217094014 SOBHA DHAKAL Dolakha GhangSukathokar 2 Bishnu Prasad Dhakal -

Groundwater Research in NEPAL for Tiger Conservation
GROUNDWATER RESEARCH IN NEPAL FOR TIGER CONSERVATION A reconnaissance study to groundwater dynamics in an alluvial mega-fan in Bardiya National Park (Terai), focusing on the interaction between groundwater and the Karnali river. Author: Hanne. Berghuis. MSc. Thesis. Program: Earth, Surface and Water at Utrecht University. 1st Supervisor: Prof. Dr. Jasper Griffioen. 2nd Supervisor: Dr. Derek Karssenberg. Date: 28-06-2019. Student No.: 6190987. Contact: [email protected]. Photo credits: Esther Leystra (2019). Nepal: Bardiya National Park. Acknowledgement I’d like to thank my supervisor Jasper Griffioen for the opportunity to hydrologically explore Bardiya. His enthusiasm for the project was inspiring and his close involvement was very motivating. My friend Ewa van Kooten introduced me to this project. Together we travelled to Nepal for three months. Thanks to her I enjoyed every single day of our time in Bardiya. She often came up with new ideas for field measurements, creative ways to fabricate field equipment or interpretations for unexpected observations. I am grateful for the Himalayan Tiger Foundation (HTF), who took the initial initiative for hydrological research in Bardiya. I very much appreciate their efforts for the conservation of the wild tiger. During the meetings in the Netherlands and around the campfire in Bardiya with the members and co of HTF, I have learned and laughed a lot. Moreover, I like to thank them for getting us in touch with the National Trust for Nature Conservation (NTNC). The staff of NTNC heartily welcomed us in Bardiya and at their office. They made us feel like a part of the NTNC-family by letting us join their festivals, dinners and campfires. -

Distribution of Arsenic Biosand Filters in Rural Nepal
DISTRIBUTION OF ARSENIC BIOSAND FILTERS IN RURAL NEPAL SLOAN SCHOOL OF MANAGEMENT APRIL 2004 THE G-LAB TEAM Basak Yildizbayrak, MBA 2004 Nikos Moschos, MBA 2004 Tamer Tamar, MBA 2004 Yann Le Tallec, Ph.D 2006 Acknowledgment: We would like to thank the Bergstrom Family Foundation for its support of this project. TABLE OF CONTENTS A. INTRODUCTION............................................................................................3 1. The Water Problem in Nepal and Arsenic Contamination............................................. 3 2. Project Scope.................................................................................................................. 3 3. Methodology ..................................................................................................................4 4. Important MIT contacts/lead people for various work streams ..................................... 4 B. EXECUTIVE SUMMARY................................................................................5 1. Short-Term Recommendations...................................................................................... 5 2. Long-Term Recommendations for Sustainable Filter Distribution ............................... 5 C. THE WORLD BANK PROJECT .....................................................................7 D. PRODUCT DESIGN AND UNIT COSTS.......................................................8 1. Existing Filters ............................................................................................................... 9 2. Alternative