Pneumococcus: Questions and Answers Information About the Disease and Vaccines
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

362.Full.Pdf
AMERICAN ACADEMY OF PEDIATRICS Committee on Infectious Diseases Policy Statement: Recommendations for the Prevention of Pneumococcal Infections, Including the Use of Pneumococcal Conjugate Vaccine (Prevnar), Pneumococcal Polysaccharide Vaccine, and Antibiotic Prophylaxis ABSTRACT. Heptavalent pneumococcal conjugate vac- lular pertussis; HbOC, Haemophilus influenzae type b conjugate cine (PCV7) is recommended for universal use in chil- vaccine; HIV, human immunodeficiency virus; AOM, acute otitis dren 23 months and younger, to be given concurrently media. with other recommended childhood vaccines at 2, 4, 6, and 12 to 15 months of age. For children 7 to 23 months he purpose of this report is to provide recom- old who have not received previous doses of PCV7, ad- ministration of a reduced number of doses is recom- mendations for use of the heptavalent pneumo- mended. Two doses of PCV7 are recommended for chil- Tcoccal conjugate vaccine (PCV7), Prevnar (Led- dren 24 to 59 months old at high risk of invasive erle Laboratories, Pearl River, NY; Wyeth-Ayerst pneumococcal infection—including children with func- Pharmaceuticals, Marietta, PA), and 23-valent pneumo- tional, anatomic, or congenital asplenia; infection with coccal polysaccharide (23PS) vaccines. In addition, rec- human immunodeficiency virus; and other predisposing ommendations for the continuing use of antibiotic pro- conditions—who have not been immunized previously phylaxis in children with sickle cell disease (SCD) and with PCV7. Recommendations have been made for use of asplenia will be given, and the use of antibiotics and 23-valent pneumococcal polysaccharide (23PS) vaccine in vaccines in children who attend out-of-home care will high-risk children to expand serotype coverage. -

Acute Otitis Media, Acute Bacterial Sinusitis, and Acute Bacterial Rhinosinusitis
Acute Otitis Media, Acute Bacterial Sinusitis, and Acute Bacterial Rhinosinusitis This guideline, developed by Larry Simmons, MD, in collaboration with the ANGELS team, on October 3, 2013, is a significantly revised version of the Recurrent Otitis Media guideline by Bryan Burke, MD, and includes the most recent information for acute otitis media, acute bacterial sinusitis, and acute bacterial rhinosinusitis. Last reviewed by Larry Simmons, MD on July 5, 2016. Preface As the risk factors for the development of acute otitis media (AOM) and acute bacterial sinusitis (ABS)/ acute bacterial rhinosinusitis (ABRS) are similar, the bacterial pathogens are essentially the same for both AOM and ABS/ABRS, and since the antimicrobial treatments are similar, the following guideline is based, unless otherwise referenced, on recently published evidenced-based guidelines by the American Academy of Pediatrics (AAP) for AOM,1,2 and by the Infectious Diseases Society of 3 America (IDSA) for ABRS. This guideline applies to children 6 months to 12 years of age and otherwise healthy children without pressure equalizer (PE) tubes, immune deficiencies, cochlear implants, or anatomic abnormalities including cleft palate, craniofacial anomalies, and Down syndrome. However, the IDSA ABRS guideline includes recommendations for children and adult patients. Key Points Acute otitis media (AOM) is characterized by a bulging tympanic membrane (TM) + middle-ear effusion. Antibiotic treatment is indicated in children ≥6 months of age with severe AOM, children 6-23 months of age with mild signs/symptoms of bilateral AOM. In children 6-23 months of age with non-severe unilateral AOM, and in children ≥24 months of age with bilateral or unilateral 1 AOM who have mild pain and low fever <39°C/102.2°F, either antibiotic treatment or observation is appropriate. -
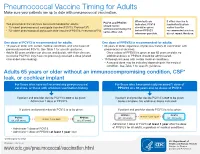
Pneumococcal Vaccine Timing for Adults Make Sure Your Patients Are up to Date with Pneumococcal Vaccination
Pneumococcal Vaccine Timing for Adults Make sure your patients are up to date with pneumococcal vaccination. When both are If either vaccine is PCV13 and PPSV23 Two pneumococcal vaccines are recommended for adults: indicated, PCV13 inadvertently given should not be 13-valent pneumococcal conjugate vaccine (PCV13, Prevnar13®) should be given earlier than the administered during the ® before PPSV23 recommended window, 23-valent pneumococcal polysaccharide vaccine (PPSV23, Pneumovax 23) same office visit. whenever possible. do not repeat the dose. One dose of PCV13 is recommended for adults: One dose of PPSV23 is recommended for adults: 19 years or older with certain medical conditions and who have not 65 years or older, regardless of previous history of vaccination with previously received PCV13. See Table 1 for specific guidance. pneumococcal vaccines. Adults 65 years or older can discuss and decide, with their clinician, – Once a dose of PPSV23 is given at age 65 years or older, no to receive PCV13 if they have not previously received a dose (shared additional doses of PPSV23 should be administered. clinical decision-making). 19 through 64 years with certain medical conditions. – A second dose may be indicated depending on the medical condition. See Table 1 for specific guidance. Adults 65 years or older without an immunocompromising condition, CSF* leak, or cochlear implant For those who have not received any pneumococcal For those who have previously received 1 dose of vaccines, or those with unknown vaccination history PPSV23 at ≥ 65 years and no doses of PCV13 If patient and provider decide PCV13 is not to be given: If patient and provider decide PCV13 is not to be given: Administer 1 dose of PPSV23. -

Adults with DIABETES Are Among Those Who Need Pneumococcal
Patients with diabetes are at an increased risk for complications from pneumococcal disease. Diabetes may be a unique risk factor for increased incidence of sepsis associated with pneumococcal infection. One of the reasons people with diabetes are at greater risk for pneumococcal disease is that they may have abnormalities in immune function that affect their reaction to infection. Pneumococcal disease causes serious illnesses like pneumonia, meningitis, and sepsis. Pneumococcal disease is serious and deadly. In the US, pneumococcal pneumonia, meningitis, and sepsis kill tens of thousands each year. Pneumococcal disease survivors may suffer hearing loss, seizures, blindness, or paralysis. Pneumococcal vaccination is recommended for all adults with diabetes. Adults with DIABETES Are Among Those Who Need Pneumococcal Vaccination There are two types of pneumococcal vaccine recommended for US adults: a pneumococcal conjugate vaccine (PCV13) and a pneumococcal polysaccharide vaccine (PPSV23). Adults 65 and older, and adults age 19 to 64 years with any of the following need to receive both vaccines: immunocompromising conditions or treatments (e.g., HIV/AIDS, leukemia, lymphoma, Hodgkin disease, radiation therapy); a damaged or missing spleen; cochlear implants; or cerebrospinal fluid leaks. Other adults for whom pneumococcal vaccination is recommended only need PPSV23, but may need more than one dose and will need PCV13 when they, too, reach age 65. Please refer to the Adult Pneumococcal Vaccination Guide or visit cdc.gov/vaccines/vpd-vac/pneumo/ for details on timing of vaccine doses. For more information and resources to educate patients about pneumococcal disease, visit adultvaccination.org/professional-resources/pneumo This initiative is supported by unrestricted educational grants from Merck & Co., Inc. -

Rate of Concurrent Otitis Media in Upper Respiratory Tract Infections with Specific Viruses
ORIGINAL ARTICLE Rate of Concurrent Otitis Media in Upper Respiratory Tract Infections With Specific Viruses Cuneyt M. Alper, MD; Birgit Winther, MD, PhD; Ellen M. Mandel, MD; J. Owen Hendley, MD; William J. Doyle, PhD Objective: To estimate the coincidence of new otitis me- Results: A total of 176 children (81%) had isolated PCR dia (OM) for first nasopharyngeal detections of the more detection of at least 1 virus. The OM coincidence rates common viruses by polymerase chain reaction (PCR). were 62 of 144 (44%) for rhinovirus, 15 of 27 (56%) for New OM episodes are usually coincident with a viral up- respiratory syncytial virus, 8 of 11 (73%) and 1 of 5 (20%) per respiratory tract infection (vURTI), but there are con- for influenza A and B, respectively, 6 of 12 (50%) for ad- flicting data regarding the association between specific enovirus, 7 of 18 (39%) for coronavirus, and 4 of 11 (36%) viruses and OM. for parainfluenza virus detections (P=.37). For rhinovi- rus, new OM occurred in 50% of children with and 32% Design: Longitudinal (October-March), prospective fol- without a concurrent CLI (P=.15), and OM risk was pre- low-up of children for coldlike illness (CLI) by diary, middle dicted by OM and breastfeeding histories and by daily ear status by pneumatic otoscopy, and vURTI by PCR. environment outside the home. Setting: Academic medical centers. Conclusions: New OM was associated with nasopha- ryngeal detection of all assayed viruses irrespective of Participants: A total of 102 families with at least 2 chil- the presence or absence of a concurrent CLI. -

2021 Medicare Vaccine Coverage Part B Vs Part D
CDPHP® Medicare Advantage Vaccine Coverage Guide Part B (Medical) vs. Part D (Pharmacy) Medicare Part B (Medical): Medicare Part D (Pharmacy): Vaccinations or inoculations Vaccinations or inoculations are included when the administration is (except influenza, pneumococcal, reasonable and necessary for the prevention of illness. and hepatitis B for members at risk) are excluded unless they are directly related to the treatment of an injury or direct exposure to a disease or condition. • Influenza Vaccine (Flu) • BCG Vaccine • Pneumococcal Vaccine • Diphtheria/Tetanus/Acellular Pertussis Vaccine (ADACEL, (Pneumovax, Prevnar 13) BOOSTRIX, DAPTACEL, INFANRIX) • Hepatitis B Vaccine • Diphtheria/Tetanus/Acellular Pertussis/Inactivated Poliovirus (Recombivax, Engerix-B) Vaccine (KINRIX, QUADRACEL) for members at moderate • Diphtheria/Tetanus Vaccine (DT, Td, TDVAX, TENIVAC) to high risk • Diphtheria/Tetanus/Acellular Pertussis/Inactivated Poliovirus Vac • Other vaccines when directly cine/ Haemophilus Influenzae Type B Conjugate Vaccine (PENTACEL) related to the treatment of an • Diphtheria/Tetanus/Acellular Pertussis/Inactivated Poliovirus injury or direct exposure to a Vaccine/Hepatitis B Vaccine (PEDIARIX) disease or condition, such as: • Haemophilus Influenzae Type B Conjugate Vaccine (ActHIB, PedvaxHIB, • Antivenom Sera Hiberix) • Diphtheria/Tetanus Vaccine • Hepatitis A Vaccine, Inactivated (VAQTA) (DT, Td, TDVAX, TENIVAC) • Hepatitis B Vaccine, Recombinant (ENGERIX-B, RECOMBIVAX HB) • Rabies Virus Vaccine for members at low risk (RabAvert, -

Global Immunization News 25 February 2011
Global Immunization News 25 February 2011 World Health Organization Global Immunization News Inside this issue: Technical Information Meeting of the Global Advisory 2 Committee on Vaccine Safety Polio eradication mourns loss of 2 NEW VACCINES, NEW true polio champion OPPORTUNITIES Announcements from The SIVAC 3 25/02/2011 from Hayatee Hasan, WHO/HQ Initiative In the past two months, four countries ― WHO position on pandemic influ- 3 Guyana, Kenya, Sierra Leone and Yemen ― enza vaccination following reports of narcolepsy subsequent to use of have introduced the pneumococcal conjugate Pandemrix vaccine. They represent the first of a series of countries introducing the vaccine in 2011. PHOTO Cold Chain and Logistics Taskforce 3 WHO concludes that quality issues 4 These introductions represent a major relating to Quinvaxem production milestone - the gap between access to new have been resolved vaccines between developed and developing AFRICA 4-6 countries is shortening; it is extraordinary to The launching of the Pneumococcal see a new vaccine launched in a developing conjugate vaccine (PCV-13) in Si- erra Leone country within one to two years of its introduction in the Americas and Europe, Kenya launches ten-valent pneumo- while in the past, it has taken several years coccal conjugate vaccine (PCV10) Vaccine carrier containing pneumococcal vaccine in (averaging 15 years) between the Kenya Meetings held in afro central introduction of new vaccines in developed and developing countries. AMERICAS 6-8 Peru introduces nationwide HPV vaccination; Argentina announces For more information regarding the launches in these countries, please see the articles on HPV vaccine introduction Kenya, Sierra Leone and Yemen. -

Effectiveness of Intranasal Live Attenuated Influenza Vaccine Against All-Cause Acute Otitis Media in Children Heikkinen Et Al Terho Heikkinen, MD, Phd,* Stan L
Mary INF VACCINE REPORTS 203098 LAIV and Acute Otitis Media Effectiveness of Intranasal Live Attenuated Influenza Vaccine Against All-cause Acute Otitis Media in Children Heikkinen et al Terho Heikkinen, MD, PhD,* Stan L. Block, MD,† Seth L. Toback, MD,‡ Xionghua Wu, PhD,‡ and Christopher S. Ambrose, MD‡ cute otitis media (AOM) remains the most common bacterial Background: Acute otitis media (AOM) is a frequent complication of influ- infection and the most frequent reason for antibiotic treatment enza in children, and influenza vaccination helps protect against influenza- A Pediatr Infect Dis J in infants and young children. Although the incidence of AOM associated AOM. A live attenuated influenza vaccine (LAIV) approved for peaks around the age of 1 year, the rates of AOM are substantial eligible children aged ≥2 years for the prevention of influenza also effec- in older children.1,2 The high prevalence of antimicrobial resistance tively reduces influenza-associated AOM. However, the annual effective- among common bacteria causing AOM has substantially compli- Lippincott Williams & Wilkins ness of LAIV against all-cause AOM is unknown. cated the management of AOM, and efforts to reduce the use of Methods: AOM rates in children aged 6–83 months from 6 randomized, antibiotics for this disease are being assessed. As a consequence, placebo-controlled trials and 2 randomized, inactivated influenza vaccine- prevention of AOM through vaccination is an important area of controlled trials were pooled and analyzed. To enable comparison with Hagerstown, MD research.3,4 studies of AOM prevention by pneumococcal conjugate vaccines, 12-month Pneumococcal conjugate vaccines (PCVs) are currently effectiveness was calculated assuming that LAIV had no effect outside of used in most developed countries to prevent severe invasive pneu- influenza seasons. -

Vaccines-Pneumococcal- Influenza- Shingles Q and A
www.RxFiles.ca - July 2019 RxFiles Q&A Summary A Crawley BSP; J Bareham BSP VACCINES: Pneumococcal, Influenza, & Shingles Immunization Guidelines and Saskatchewan Health Coverage Considerations Vaccines prevent morbidity and mortality to various degrees. Many vaccines are publicly funded, especially if potentially life-saving. When guideline recommendations & public coverage differ, clinicians/patients must weigh the evidence for benefit versus the out-of-pocket patient cost. Note: vaccine costs listed in this document do not include markup, dispensing fees, or administration fees, which can vary depending on who is administering the vaccine. 1. Who may benefit from a PNEUMOCOCCAL vaccine in Saskatchewan? Available vaccines include the PNEUMOVAX 23-valent vaccine ($24) and the PREVNAR 13-valent vaccine ($103). Covered in Sask:1 Evidence for benefit Clinical Controversies 1 dose of PNEUMOVAX for anyone A single pneumococcal vaccination Immunization guidelinesNACI suggest that if ≥65 years old. appears to reduce the risk of PNEUMOVAX was given before the age of 65, a booster 1 dose of PNEUMOVAX for anyone community-acquired pneumonia by dose should be given 5 years later to all patients with specific medical conditions 30% (NNT = 55) and the risk of a COPD regardless of risk factors.18 This recommendation is (e.g. diabetes, COPD, others*). exacerbation by 40% (NNT = 8).2,19,20 based on the tendency for older adults to have a 2 doses of PNEUMOVAX spaced 5+ Benefits are consistent regardless of weakened immune system. years apart for anyone with which vaccine formulation is used.2-4 Immunization guidelines suggest that the theoretical specific high risk medical No trials have yet assessed the efficacy greater potency of PREVNAR over PNEUMOVAX may conditions (e.g. -

Otovent Nasal Balloon for Otitis Media with Effusion
pat hways Otovent nasal balloon for otitis media with effusion Medtech innovation briefing Published: 15 March 2016 www.nice.org.uk/guidance/mib59 Summary Otovent is a balloon device designed to relieve the symptoms of otitis media with effusion, commonly known as glue ear. An Otovent kit consists of a nose piece and 5 latex balloons that are inflated yb blowing through the nose. Four randomised controlled trials, all in children, have shown that using the device causes significant improvements, compared with standard care, in middle ear function; 1 of the trials also reported a significant reduction in the need for entilationv tube (grommet) insertion surgery. Outcomes varied by compliance with (that is, adherence to) treatment, and standard care was not consistently described. The Otovent kit is available to buy or can be provided on a NHS prescription. The recommended retail price is £7.84 including VAT and the current Drug Tariff price is £4.90 excluding VAT. No additional consumables are needed. © NICE 2020. All rights reserved. Subject to Notice of rights (https://www.nice.org.uk/terms-and- Page 1 of conditions#notice-of-rights). 24 Otovent nasal balloon for otitis media with effusion (MIB59) Product summary and likely place in Effectiveness and safety therapy • No relevant evidence was found for the use of • Otovent is designed to help open the Otovent in adults. Eustachian tubes and equalise the air pressure in the middle ear. • Four randomised controlled trials involving a total of 565 children showed statistically significant • The device can be used in people improvements in middle ear function with with Eustachian tube dysfunction Otovent compared with standard care, as associated with glue ear (otitis determined by tympanometry and pneumatic media with effusion), or after flying, otometry. -

Pneumococcal Vaccine Called PCV7, Or to Any Vaccine Spread from Person to Person Through Close Contact
VACCINE INFORMATION STATEMENT Pneumococcal Conjugate Vaccine (PCV13) Many Vaccine Information Statements are available in Spanish and other languages. See www.immunize.org/vis Hojas de informacion sobre vacunas est&n What You Need to Know disponibles en espafiol y en muclios otros idiomas, Visite www.immunize.org/vis 1 Why get vaccinated? ] Some people should not get this vaccine Vaccination can protect both children and adults from pneumococcal disease. Anyone who has ever had a life-threatening allergic reaction to a dose of this vaccine, to an earlier Pneumococcal disease is caused by bacteria that can pneumococcal vaccine called PCV7, or to any vaccine spread from person to person through close contact. It containing diphtheria toxoid (for example, DTaP), can cause ear infections, and it can also lead to more should not get PC VI3. serious infections of the: • Lungs (pneumonia),' Anyone with a severe allergy to any component of • Blood (bacteremia), and PC VI3 should not get the vaccine. Tell your doctor if the • Covering of the brain and spinal cord (meningitis). person being vaccinated has any severe allergies. Pneumococcal pneumonia is most common among If the person scheduled for vaccination is not feeling adults. Pneumococcal meningitis can cause deafness and well, your healthcare provider might decide to brain damage, and it kills about 1 child in 10 who get it. reschedule the shot on another day. Anyone can get pneumococcal disease, but children under 2 years of age and adults 65 years and older, Risks of a vaccine reaction people with certain medical conditions, and cigarette With any medicine, including vaccines, there is a chance smokers are at the highest risk. -

Adult Pneumococcal Vaccination Recommendations
Adult Pneumococcal Vaccination Recommendations Background1,2 Streptococcus pneumoniae is a leading cause of invasive disease, including bacteremia, meningitis, and pneumonia in the United States. It is estimated to be responsible for 4 million episodes of illness, 445,000 hospitalizations, and 22,000 deaths per year. Incidence of invasive disease ranges from 3.8 cases per 100,000 persons among adults aged 18-34 years to 36.4 cases per 100,000 persons among adults aged ≥ 65 years. Patients with high-risk immunocompromising medical conditions, such as hematologic malignancies and human immunodeficiency virus, have up to a 20-fold increased risk for invasive pneumococcal disease. The Centers for Disease Control and Prevention (CDC) Advisory Committee on Immunization Practices (ACIP) currently recommends pneumococcal for all adults aged ≥ 65 years, as well as adults aged 19-64 years with immumocompromising conditions. Two pneumococcal vaccines are available, 23-valent pneumococcal polysaccharide vaccine (PPSV23) and 13-valent polysaccharide vaccine (PCV13). The recommendations below outline the preferred formulations and vaccination schedules according to the ACIP guidelines. Pneumococcal Vaccination for Adults Aged ≥ 65 Years3,4 In 2010, ACIP recommended that all adults should be vaccinated with PPSV23 at age 65 years. In 2014, these recommendations were updated based on results from a randomized, placebo-controlled trial showing efficacy of PCV13 in preventing pneumonia in 85,000 adults aged ≥ 65 years. ACIP now recommends that both PCV13 and PPSV23 should be routinely administered to all adults aged ≥ 65 years. In addition, ACIP recently revised the recommended intervals for sequential use of PCV13 and PPSV23 in this patient population.