Identification of Chemical Composition of Plant Extracts of Nardostachys Jatamansi DC Using GC/MS
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Valerenic Acid Potentiates and Inhibits GABAA Receptors: Molecular Mechanism and Subunit Specificity
ARTICLE IN PRESS + MODEL Neuropharmacology xx (2007) 1e10 www.elsevier.com/locate/neuropharm Valerenic acid potentiates and inhibits GABAA receptors: Molecular mechanism and subunit specificity S. Khom a, I. Baburin a, E. Timin a, A. Hohaus a, G. Trauner b, B. Kopp b, S. Hering a,* a Department of Pharmacology and Toxicology, University of Vienna, Althanstrasse 14, A-1090 Vienna, Austria b Department of Pharmacognosy, University of Vienna, Althanstrasse 14, A-1090 Vienna, Austria Received 8 December 2006; received in revised form 11 April 2007; accepted 30 April 2007 Abstract Valerian is a commonly used herbal medicinal product for the treatment of anxiety and insomnia. Here we report the stimulation of chloride currents through GABAA receptors (IGABA) by valerenic acid (VA), a constituent of Valerian. To analyse the molecular basis of VA action, we expressed GABAA receptors with 13 different subunit compositions in Xenopus oocytes and measured IGABA using the two-microelectrode voltage-clamp technique. We report a subtype-dependent stimulation of IGABA by VA. Only channels incorporating b2 or b3 subunits were stimulated by VA. Replacing b2/3 by b1 drastically reduced the sensitivity of the resulting GABAA channels. The stimulatory effect of VA on a1b2 receptors was substantially reduced by the point mutation b2N265S (known to inhibit loreclezole action). Mutating the corresponding residue of b1 (b1S290N) induced VA sensitivity in a1b1S290N comparable to a1b2 receptors. Modulation of IGABA was not significantly dependent on incorporation of a1, a2, a3 or a5 subunits. VA displayed a significantly lower efficiency on channels incorporating a4 subunits. IGABA modulation by VA was not g subunit dependent and not inhibited by flumazenil (1 mM). -

Indigenous Use and Ethnopharmacology of Medicinal Plants in Far-West Nepal
Indigenous Use and Ethnopharmacology of Medicinal Plants in Far-west Nepal Ripu M. Kunwar, Y. Uprety, C. Burlakoti, C.L. Chowdhary and R.W. Bussmann Research Abstract Ethnopharmacological knowledge is common and im- jor part of these therapies. Interest in phytomedicine is port among tribal populations but much of the information also renewed during the last decade and many medicinal is empirical at best lacking scientific validation. Despite plant species are being screened for pharmacological ac- widespread use of plant resources in traditional medi- tivities. The global demand of herbal medicine is growing cines, bioassay analysis of very few plant species have and its market is expanding at the rate of 20% annually in been conducted to investigate their medicinal properties, India (Srivastava 2000, Subrat 2002). The world market and to ascertain safety and efficacy of traditional reme- for herbal remedies in 1999 was worth of U.S.$19.4 bil- dies. The present study analyses indigenous uses of me- lion (Laird & Pierce 2002). dicinal plants of far-west Nepal and compares with earlier ayurveda studies, phytochemical assessments and phar- Numerous drugs have entered into the international mar- macological actions. A field study was carried out in Baita- ket through exploration of ethnopharmacology and tradi- di and Darchula districts of far-west Nepal. Group discus- tional medicine (Bussmann 2002) with extensive uses of sions, informal meetings, questionnaire surveys and field medicinal plants. It is estimated that 25% of prescription observations were employed for primary data collection. drugs contain active principles derived from higher plants (Tiwari & Joshi 1990). The first compound derived from Voucher specimens were collected with field notes and herbal remedies to enter the international market was codes and deposited at Tribhuvan University Central Her- ephedrine, an amphetamine like stimulant from Ephed- barium (TUCH), Kathmandu. -

A Review on Biological Activities and Conservation of Endangered Medicinal Herb Nardostachys Jatamansi
Int. J. Med. Arom. Plants, ISSN 2249 – 4340 REVIEW ARTICLE Vol. 3, No. 1, pp. 113-124, March 2013 A review on biological activities and conservation of endangered medicinal herb Nardostachys jatamansi Uma M. SINGH1, Vijayta GUPTA2, Vivekanand P. RAO3, Rakesh S. SENGAR3, Manoj K. YADAV3 1Department of Molecular Biology & Genetic Engineering, Govind Ballabh Pant University of Agriculture & Technology, Pantnagar, Uttarakhand-263145, India. 2Biotechnology Division, Central Institute of Medicinal and Aromatic Plant, Lucknow, Uttar Pradesh-226015, India. 3Department of Agriculture Biotechnology, Sardar Vallabh-bhai Patel University of Agriculture & Technolo- gy, Meerut, Uttar Pradesh-250110, India. Article History: Received 6th December 2012, Revised 23rd January 2013, Accepted 25th January 2013. Abstract: Nardostachys jatamansi DC also known as Indian Spikenard or Indian Valerian, is a valued medicinal plant of family Valerianaceae. This rhizome bearing plant is native of the Himalayas of India and Nepal and preferably found from 2200 m to 5000 m asl in random forms. The extract of rhizome is widely used in the formulation of traditional Ayurvedic medicines as well as modern herbal preparations for curing several ailments. In some parts of their range ow- ing to overharvest for medicinal use and trade, habitat degradation and other biotic interferences leads plant into threat category. In India the observed population of jatamansi declines of 75-80% and classified as Endangered in Arunachal Pradesh, Sikkim and Himachal Pradesh and Critically Endangered in Uttarakhand. Realizing the high level of threat CITES has notified N. jatamansi for its schedule care to ensure the conservation. Hence, emphasis should be given on proper conservation and apply biotechnological tools for sustainable use which in turn help to save it from extinction. -

Plant-Based Medicines for Anxiety Disorders, Part 2: a Review of Clinical Studies with Supporting Preclinical Evidence
CNS Drugs 2013; 24 (5) Review Article Running Header: Plant-Based Anxiolytic Psychopharmacology Plant-Based Medicines for Anxiety Disorders, Part 2: A Review of Clinical Studies with Supporting Preclinical Evidence Jerome Sarris,1,2 Erica McIntyre3 and David A. Camfield2 1 Department of Psychiatry, Faculty of Medicine, University of Melbourne, Richmond, VIC, Australia 2 The Centre for Human Psychopharmacology, Swinburne University of Technology, Melbourne, VIC, Australia 3 School of Psychology, Charles Sturt University, Wagga Wagga, NSW, Australia Correspondence: Jerome Sarris, Department of Psychiatry and The Melbourne Clinic, University of Melbourne, 2 Salisbury Street, Richmond, VIC 3121, Australia. Email: [email protected], Acknowledgements Dr Jerome Sarris is funded by an Australian National Health & Medical Research Council fellowship (NHMRC funding ID 628875), in a strategic partnership with The University of Melbourne, The Centre for Human Psychopharmacology at the Swinburne University of Technology. Jerome Sarris, Erica McIntyre and David A. Camfield have no conflicts of interest that are directly relevant to the content of this article. 1 Abstract Research in the area of herbal psychopharmacology has revealed a variety of promising medicines that may provide benefit in the treatment of general anxiety and specific anxiety disorders. However, a comprehensive review of plant-based anxiolytics has been absent to date. Thus, our aim was to provide a comprehensive narrative review of plant-based medicines that have clinical and/or preclinical evidence of anxiolytic activity. We present the article in two parts. In part one, we reviewed herbal medicines for which only preclinical investigations for anxiolytic activity have been performed. In this current article (part two), we review herbal medicines for which there have been both preclinical and clinical investigations for anxiolytic activity. -
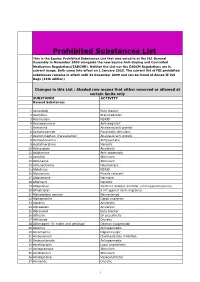
Prohibited Substances List
Prohibited Substances List This is the Equine Prohibited Substances List that was voted in at the FEI General Assembly in November 2009 alongside the new Equine Anti-Doping and Controlled Medication Regulations(EADCMR). Neither the List nor the EADCM Regulations are in current usage. Both come into effect on 1 January 2010. The current list of FEI prohibited substances remains in effect until 31 December 2009 and can be found at Annex II Vet Regs (11th edition) Changes in this List : Shaded row means that either removed or allowed at certain limits only SUBSTANCE ACTIVITY Banned Substances 1 Acebutolol Beta blocker 2 Acefylline Bronchodilator 3 Acemetacin NSAID 4 Acenocoumarol Anticoagulant 5 Acetanilid Analgesic/anti-pyretic 6 Acetohexamide Pancreatic stimulant 7 Acetominophen (Paracetamol) Analgesic/anti-pyretic 8 Acetophenazine Antipsychotic 9 Acetylmorphine Narcotic 10 Adinazolam Anxiolytic 11 Adiphenine Anti-spasmodic 12 Adrafinil Stimulant 13 Adrenaline Stimulant 14 Adrenochrome Haemostatic 15 Alclofenac NSAID 16 Alcuronium Muscle relaxant 17 Aldosterone Hormone 18 Alfentanil Narcotic 19 Allopurinol Xanthine oxidase inhibitor (anti-hyperuricaemia) 20 Almotriptan 5 HT agonist (anti-migraine) 21 Alphadolone acetate Neurosteriod 22 Alphaprodine Opiod analgesic 23 Alpidem Anxiolytic 24 Alprazolam Anxiolytic 25 Alprenolol Beta blocker 26 Althesin IV anaesthetic 27 Althiazide Diuretic 28 Altrenogest (in males and gelidngs) Oestrus suppression 29 Alverine Antispasmodic 30 Amantadine Dopaminergic 31 Ambenonium Cholinesterase inhibition 32 Ambucetamide Antispasmodic 33 Amethocaine Local anaesthetic 34 Amfepramone Stimulant 35 Amfetaminil Stimulant 36 Amidephrine Vasoconstrictor 37 Amiloride Diuretic 1 Prohibited Substances List This is the Equine Prohibited Substances List that was voted in at the FEI General Assembly in November 2009 alongside the new Equine Anti-Doping and Controlled Medication Regulations(EADCMR). -

Medicinal Plant Conservation
MEDICINAL Medicinal Plant PLANT SPECIALIST GROUP Conservation Silphion Volume 13 Newsletter of the Medicinal Plant Specialist Group of the IUCN Species Survival Commission Chaired by Danna J. Leaman Chair’s Note . 2 Silphion revisited – Monika Kiehn . 4 Taxon File On the history, botany, distribution, uses and conservation aspects of Nardostachys jatamansi in India – Niranjan Chandra Shah. 8 A dogmatic tradition posing threat to Bombax ceiba - the Indian Red Kapok Tree – Vartika Jain, S.K. Verma & S.S. Katewa. 12 Estudio de mercado y sustentabilidad de la recolección silvestre de bailahuén, una planta medicinal chilena – Hermine Vogel, Benita González, José San Martín, Iván Razmilic, Pablo Villalobos & Ernst Schneider . 15 Conferences and Meetings Coming up – Natalie Hofbauer. 21 CITES News – Uwe Schippmann . 22 CITES medicinal plant species in Asia – treasured past, threatened future? – Teresa Mulliken & Uwe Schippmann . 23 Reviews and Notices of Publication. 31 List of MPSG Members . 33 ISSN 1430-95X 1 December 2007 our future membership-building efforts in Africa, Aus- Chair’s Note tralia-New Zealand, the Pacific, and the Middle East. Table 1. Changes in MPSG membership by region, 1995- Danna J. Leaman 2007 Looking back Region 1995 % 2007 % % change As this 13th volume of Medicinal Plant Conservation is Africa 9 28 7 8 -20 prepared, I am looking back to the first volume, a slen- Asia 5 15 25 29 +14 der eight pages, published in April 1995, one year after Australia-NZ 1 3 2 2 -1 the Medicinal Plant Specialist Group was established within -

Genetic Diversity Analysis of Nardostachys Jatamansi DC, an Endangered Medicinal Plant of Central Himalaya, Using Random Amplified Polymorphic DNA (RAPD) Markers
Vol. 12(20), pp. 2816-2821, 15 May, 2013 DOI: 10.5897/AJB12.9717 African Journal of Biotechnology ISSN 1684-5315 ©2013 Academic Journals http://www.academicjournals.org/AJB Full Length Research Paper Genetic diversity analysis of Nardostachys jatamansi DC, an endangered medicinal plant of Central Himalaya, using random amplified polymorphic DNA (RAPD) markers Uma M. Singh1, Dinesh Yadav2, M. K. Tripathi3, Anil Kumar4 and Manoj K. Yadav1* 1Department of Biotechnology, SVP University of Agriculture and Technology, Meerut 250 110, India. 2Department of Biotechnology, DDU University, Gorakhpur, India. 3Department of Biochemistry, Central Institute of Agricultural Engineering, Bhopal, India. 4Department of MBGE, GB Pant University of Agriculture and Technology, Pantnagar, India. Accepted 18 April, 2013 The genetic diversity analysis of eight populations of Nardostachys jatamansi DC. collected from different altitude of Central Himalaya has been attempted using 24 sets of random amplified polymorphic DNA (RAPD) primers. These sets of RAPD marker generated a total of 346 discernible and reproducible bands across the analysed population with 267 polymorphic and 75 monomorphic bands. The unweighted pair group method with arithmetic average (UPGMA) cluster analysis revealed three distinct clusters: I, II and III. The cluster I was represented by N. jatamansi population collected from Panwali Kantha (3200 m asl) and Kedarnath (3584 m asl), India together with Jumla (2562 m asl) from Nepal. Cluster II included collections from Har Ki Doon (3400 m asl) and Tungnath (3600 m asl) from India while Cluster III was represented by collections from Munsiyari (2380 m asl), Dayara (3500 m asl) and Valley of Flowers (3400 m asl) from India. -

Ion Channels
UC Davis UC Davis Previously Published Works Title THE CONCISE GUIDE TO PHARMACOLOGY 2019/20: Ion channels. Permalink https://escholarship.org/uc/item/1442g5hg Journal British journal of pharmacology, 176 Suppl 1(S1) ISSN 0007-1188 Authors Alexander, Stephen PH Mathie, Alistair Peters, John A et al. Publication Date 2019-12-01 DOI 10.1111/bph.14749 License https://creativecommons.org/licenses/by/4.0/ 4.0 Peer reviewed eScholarship.org Powered by the California Digital Library University of California S.P.H. Alexander et al. The Concise Guide to PHARMACOLOGY 2019/20: Ion channels. British Journal of Pharmacology (2019) 176, S142–S228 THE CONCISE GUIDE TO PHARMACOLOGY 2019/20: Ion channels Stephen PH Alexander1 , Alistair Mathie2 ,JohnAPeters3 , Emma L Veale2 , Jörg Striessnig4 , Eamonn Kelly5, Jane F Armstrong6 , Elena Faccenda6 ,SimonDHarding6 ,AdamJPawson6 , Joanna L Sharman6 , Christopher Southan6 , Jamie A Davies6 and CGTP Collaborators 1School of Life Sciences, University of Nottingham Medical School, Nottingham, NG7 2UH, UK 2Medway School of Pharmacy, The Universities of Greenwich and Kent at Medway, Anson Building, Central Avenue, Chatham Maritime, Chatham, Kent, ME4 4TB, UK 3Neuroscience Division, Medical Education Institute, Ninewells Hospital and Medical School, University of Dundee, Dundee, DD1 9SY, UK 4Pharmacology and Toxicology, Institute of Pharmacy, University of Innsbruck, A-6020 Innsbruck, Austria 5School of Physiology, Pharmacology and Neuroscience, University of Bristol, Bristol, BS8 1TD, UK 6Centre for Discovery Brain Science, University of Edinburgh, Edinburgh, EH8 9XD, UK Abstract The Concise Guide to PHARMACOLOGY 2019/20 is the fourth in this series of biennial publications. The Concise Guide provides concise overviews of the key properties of nearly 1800 human drug targets with an emphasis on selective pharmacology (where available), plus links to the open access knowledgebase source of drug targets and their ligands (www.guidetopharmacology.org), which provides more detailed views of target and ligand properties. -

IUCN Red Listed Medicinal Plants of Siddha
REVIEW ARTICLE IUCN Red Listed Medicinal Plants of Siddha Divya Kallingilkalathil Gopi, Rubeena Mattummal, Sunil Kumar Koppala Narayana*, Sathiyarajeshwaran Parameswaran Siddha Central Research Institute, (Central Council for Research in Siddha, Ministry of AYUSH, Govt. of India), Arumbakkam, Chennai 600106, India. *Correspondence: E-mail: [email protected] ABSTRACT Introduction: Siddha system which aims at both curative and preventive aspects is a holistic treatment methodology using herbals, metals, minerals and animal products. Medicinal plant conservation is one of global concerns because the consequence is loss of many species useful in the primary healthcare of mankind. These natural resources are dwindling, as nearly 80 to 85% of raw drugs are sourced from the wild. International Union for Conservation of Nature (IUCN) is the global authority on the status of the natural world and the measures needed to safeguard it. IUCN congresses have produced several key international environmental agreements like the Convention on Biological Diversity (CBD), the Convention on International Trade in Endangered Species (CITES) etc. It is noted that raw drugs for making a good number of Siddha formulations are derived from plants falling under IUCN’s rare, endangered and threatened (RET) category. The current study is aimed at exploring the RET status of medicinal plants used in Siddha. Method: The data of medicinal plants used in various Siddha formulations and as single drugs were collected and the IUCN status of the plants was checked in the Red list. Result: Siddha medicinal plants like Aconitum heterophyllum, Aquilaria malaccensis, Adhatoda beddomei, Nardostachys jatamansi are some of the examples of critically endangered species of plants facing threat due to continuous exploitation from wild. -

Zebrafish Behavioural Profiling Identifies GABA and Serotonin
ARTICLE https://doi.org/10.1038/s41467-019-11936-w OPEN Zebrafish behavioural profiling identifies GABA and serotonin receptor ligands related to sedation and paradoxical excitation Matthew N. McCarroll1,11, Leo Gendelev1,11, Reid Kinser1, Jack Taylor 1, Giancarlo Bruni 2,3, Douglas Myers-Turnbull 1, Cole Helsell1, Amanda Carbajal4, Capria Rinaldi1, Hye Jin Kang5, Jung Ho Gong6, Jason K. Sello6, Susumu Tomita7, Randall T. Peterson2,10, Michael J. Keiser 1,8 & David Kokel1,9 1234567890():,; Anesthetics are generally associated with sedation, but some anesthetics can also increase brain and motor activity—a phenomenon known as paradoxical excitation. Previous studies have identified GABAA receptors as the primary targets of most anesthetic drugs, but how these compounds produce paradoxical excitation is poorly understood. To identify and understand such compounds, we applied a behavior-based drug profiling approach. Here, we show that a subset of central nervous system depressants cause paradoxical excitation in zebrafish. Using this behavior as a readout, we screened thousands of compounds and identified dozens of hits that caused paradoxical excitation. Many hit compounds modulated human GABAA receptors, while others appeared to modulate different neuronal targets, including the human serotonin-6 receptor. Ligands at these receptors generally decreased neuronal activity, but paradoxically increased activity in the caudal hindbrain. Together, these studies identify ligands, targets, and neurons affecting sedation and paradoxical excitation in vivo in zebrafish. 1 Institute for Neurodegenerative Diseases, University of California, San Francisco, CA 94143, USA. 2 Cardiovascular Research Center and Division of Cardiology, Department of Medicine, Massachusetts General Hospital, Harvard Medical School, Charlestown, MA 02129, USA. -

Spikenard, Safety Data Sheet
Safety Data Sheet Section 1: Identification Product Name: Spikenard Oil Botanical Name: Nardostachys jatamansi Synonyms: Nardostachys grandiflora, Nardus indica, Patrinia jatamansi, Valeriana jatamansi, Valeriana wallichii, Nardostachys chinensis, Nardostachys gracilis INCI Name: Nardostachys chinensis root oil CAS #: 8022-22-8 Country of Origin: Nepal Company: Soapgoods Inc Address: 1824 Willow Trail Pkwy, Ste 200. Norcross. GA 30093 Phone: (404) 924-9080 E-Mail: [email protected] Emergency Phone: Chemtrec: 1-800-424-9300 Recommended Use: Personal Care Section 2: Composition/Information on Ingredients Chemical Identification: Oil, spikenard UN No. 2319: Terpene hydrocarbons, n.o.s. Packaging Group: III Class: 3 Section 3: Hazard(s) Identification Carvacrol. Section 4: Physical and Chemical Properties Appearance: Golden yellow to greenish color slightly viscous liquid. Odor: Characteristic earthy pleasant woody odor. Solubility: Soluble in alcohol and oils. Insoluble in water. Specific Gravity: 0.930 - 0.98 @ 20°C Optical Rotation: -12.0 - -8.0 @ 20°C Refractive Index: 1.500 - 1.545 @ 20°C Gurjunene: 30 - 65 % Patchoulene: 10 - 30 % Maaliene: 5.0 - 18 % Extraction Method: Steam distillation of the dried root. Contents: Gurjunene, patchoulene, maaliene, aristolone, patchouli alcohol, seychellene, nardol, nardostachone, camphene, pinene, limonene Flash Point: 85 °C Section 5: Fire-Fighting Measures Flash Point: 85 °C Combustible liquid. Will ignite if moderately heated. Section 6: Stability and Reactivity Reactivity: Stable. Decomposition: When heated to decomposition produces toxic and carbon monoxide smoke. Section 7: Toxicological Information/Information Liquid may irritate skin and eyes. Should be avoided during pregnancy. Section 8: Exposure Controls/Personal Protection Spillage: Absorb spills, cover with an inert, non-combustible, inorganic absorbent material, and remove to an approved disposal container. -

Plant Conservation Report 2020
Secretariat of the CBD Technical Series No. 95 Convention on Biological Diversity 4 PLANT CONSERVATION95 REPORT 2020: A review of progress towards the Global Strategy for Plant Conservation 2011-2020 CBD Technical Series No. 95 PLANT CONSERVATION REPORT 2020: A review of progress towards the Global Strategy for Plant Conservation 2011-2020 A contribution to the fifth edition of the Global Biodiversity Outlook (GBO-5). The designations employed and the presentation of material in this publication do not imply the expression of any opinion whatsoever on the part of the copyright holders concerning the legal status of any country, territory, city or area or of its authorities, or concerning the delimitation of its frontiers or boundaries. This publication may be reproduced for educational or non-profit purposes without special permission, provided acknowledgement of the source is made. The Secretariat of the Convention and Botanic Gardens Conservation International would appreciate receiving a copy of any publications that use this document as a source. Reuse of the figures is subject to permission from the original rights holders. Published by the Secretariat of the Convention on Biological Diversity in collaboration with Botanic Gardens Conservation International. ISBN 9789292257040 (print version); ISBN 9789292257057 (web version) Copyright © 2020, Secretariat of the Convention on Biological Diversity Citation: Sharrock, S. (2020). Plant Conservation Report 2020: A review of progress in implementation of the Global Strategy for Plant Conservation 2011-2020. Secretariat of the Convention on Biological Diversity, Montréal, Canada and Botanic Gardens Conservation International, Richmond, UK. Technical Series No. 95: 68 pages. For further information, contact: Secretariat of the Convention on Biological Diversity World Trade Centre, 413 Rue St.