Telemetry As a Tool to Measure Sedative Effects of a Valerian Root Extract and Its Single Constituents in Mice
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Vademecum Agrovet Market Animal Health
Vademecum Agrovet Market Animal Health We are a Peruvian company focused on the development, production and commercialization of veterinary products, driving its technical and creative development to meet the needs of veterinarians and stock farmers with unique products of high quality. www.agrovetmarket.com Mission l Products of Unique Class Provide veterinary, nutritional and farmaceutical products of unique class; developed in a creative and innovative way, under high standards of quality that allow us to reach international markets and consolidate locally through the formal stablishment of strategical alliances. Antibiotics Line of large animals am Line of companion animals ac Line of poultry and swine av www.agrovetmarket.com Antibiotics ® Agrogenta 11 | Vetigen 11 Injectable Solution Broad-spectrum aminoglycoside Composition: Gentamicin (as sulphate) 110 mg, excipients q.s. ad 1 mL. Indications: Treatment and prevention of infections caused by microorganisms sensitive to gentamicin (of the urogenital, respiratory and gastrointestinal systems). Also useful in cases of mastitis, metritis, post-operatory and cutaneous infections, septicemias, among others.. Dosage and Administration: Cattle, horse, sheep, goat, swine, camelid: 1 mL/27.5 kg of b.w.; young animals, dogs and cats: 1 mL/14 kg; poultry: 0.1 mL/1.4 kg; every 24 hours for 3 to 5 consecutive days by subcutaneous or intramuscular route. Intrauterine or intra-mammary route: Cows: 2 mL diluted in 20 mL of physiological saline solution for 3 to 5 days. Mares: 20 mL diluted in 200 - 500 mL of physiological saline solution for 3 to 5 days (only intrauterine route). Commercial Presentation: Bottle x 100 mL and 250 mL. -

Valerenic Acid Potentiates and Inhibits GABAA Receptors: Molecular Mechanism and Subunit Specificity
ARTICLE IN PRESS + MODEL Neuropharmacology xx (2007) 1e10 www.elsevier.com/locate/neuropharm Valerenic acid potentiates and inhibits GABAA receptors: Molecular mechanism and subunit specificity S. Khom a, I. Baburin a, E. Timin a, A. Hohaus a, G. Trauner b, B. Kopp b, S. Hering a,* a Department of Pharmacology and Toxicology, University of Vienna, Althanstrasse 14, A-1090 Vienna, Austria b Department of Pharmacognosy, University of Vienna, Althanstrasse 14, A-1090 Vienna, Austria Received 8 December 2006; received in revised form 11 April 2007; accepted 30 April 2007 Abstract Valerian is a commonly used herbal medicinal product for the treatment of anxiety and insomnia. Here we report the stimulation of chloride currents through GABAA receptors (IGABA) by valerenic acid (VA), a constituent of Valerian. To analyse the molecular basis of VA action, we expressed GABAA receptors with 13 different subunit compositions in Xenopus oocytes and measured IGABA using the two-microelectrode voltage-clamp technique. We report a subtype-dependent stimulation of IGABA by VA. Only channels incorporating b2 or b3 subunits were stimulated by VA. Replacing b2/3 by b1 drastically reduced the sensitivity of the resulting GABAA channels. The stimulatory effect of VA on a1b2 receptors was substantially reduced by the point mutation b2N265S (known to inhibit loreclezole action). Mutating the corresponding residue of b1 (b1S290N) induced VA sensitivity in a1b1S290N comparable to a1b2 receptors. Modulation of IGABA was not significantly dependent on incorporation of a1, a2, a3 or a5 subunits. VA displayed a significantly lower efficiency on channels incorporating a4 subunits. IGABA modulation by VA was not g subunit dependent and not inhibited by flumazenil (1 mM). -

Plant-Based Medicines for Anxiety Disorders, Part 2: a Review of Clinical Studies with Supporting Preclinical Evidence
CNS Drugs 2013; 24 (5) Review Article Running Header: Plant-Based Anxiolytic Psychopharmacology Plant-Based Medicines for Anxiety Disorders, Part 2: A Review of Clinical Studies with Supporting Preclinical Evidence Jerome Sarris,1,2 Erica McIntyre3 and David A. Camfield2 1 Department of Psychiatry, Faculty of Medicine, University of Melbourne, Richmond, VIC, Australia 2 The Centre for Human Psychopharmacology, Swinburne University of Technology, Melbourne, VIC, Australia 3 School of Psychology, Charles Sturt University, Wagga Wagga, NSW, Australia Correspondence: Jerome Sarris, Department of Psychiatry and The Melbourne Clinic, University of Melbourne, 2 Salisbury Street, Richmond, VIC 3121, Australia. Email: [email protected], Acknowledgements Dr Jerome Sarris is funded by an Australian National Health & Medical Research Council fellowship (NHMRC funding ID 628875), in a strategic partnership with The University of Melbourne, The Centre for Human Psychopharmacology at the Swinburne University of Technology. Jerome Sarris, Erica McIntyre and David A. Camfield have no conflicts of interest that are directly relevant to the content of this article. 1 Abstract Research in the area of herbal psychopharmacology has revealed a variety of promising medicines that may provide benefit in the treatment of general anxiety and specific anxiety disorders. However, a comprehensive review of plant-based anxiolytics has been absent to date. Thus, our aim was to provide a comprehensive narrative review of plant-based medicines that have clinical and/or preclinical evidence of anxiolytic activity. We present the article in two parts. In part one, we reviewed herbal medicines for which only preclinical investigations for anxiolytic activity have been performed. In this current article (part two), we review herbal medicines for which there have been both preclinical and clinical investigations for anxiolytic activity. -

(12) United States Patent (10) Patent No.: US 9,101,662 B2 Tamarkin Et Al
USOO91 01662B2 (12) United States Patent (10) Patent No.: US 9,101,662 B2 Tamarkin et al. (45) Date of Patent: *Aug. 11, 2015 (54) COMPOSITIONS WITH MODULATING A61K 47/32 (2013.01); A61 K9/0014 (2013.01); AGENTS A61 K9/0031 (2013.01); A61 K9/0034 (2013.01); A61 K9/0043 (2013.01); A61 K (71) Applicant: Foamix Pharmaceuticals Ltd., Rehovot 9/0046 (2013.01); A61 K9/0048 (2013.01); (IL) A61 K9/0056 (2013.01) (72) Inventors: Dov Tamarkin, Macabim (IL); Meir (58) Field of Classification Search Eini, Ness Ziona (IL); Doron Friedman, CPC ........................................................ A61 K9/12 Karmei Yosef (IL); Tal Berman, Rishon See application file for complete search history. le Ziyyon (IL); David Schuz, Gimzu (IL) (56) References Cited (73) Assignee: Foamix Pharmaceuticals Ltd., Rehovot U.S. PATENT DOCUMENTS (IL) 1,159,250 A 11/1915 Moulton (*) Notice: Subject to any disclaimer, the term of this 1,666,684 A 4, 1928 Carstens patent is extended or adjusted under 35 1924,972 A 8, 1933 Beckert 2,085,733. A T. 1937 Bird U.S.C. 154(b) by 0 days. 2,390,921 A 12, 1945 Clark This patent is Subject to a terminal dis 2,524,590 A 10, 1950 Boe claimer. 2,586.287 A 2/1952 Apperson 2,617,754 A 1 1/1952 Neely 2,767,712 A 10, 1956 Waterman (21) Appl. No.: 14/045,528 2.968,628 A 1/1961 Reed 3,004,894 A 10/1961 Johnson et al. (22) Filed: Oct. 3, 2013 3,062,715 A 11/1962 Reese et al. -
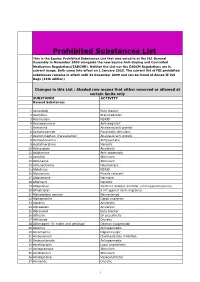
Prohibited Substances List
Prohibited Substances List This is the Equine Prohibited Substances List that was voted in at the FEI General Assembly in November 2009 alongside the new Equine Anti-Doping and Controlled Medication Regulations(EADCMR). Neither the List nor the EADCM Regulations are in current usage. Both come into effect on 1 January 2010. The current list of FEI prohibited substances remains in effect until 31 December 2009 and can be found at Annex II Vet Regs (11th edition) Changes in this List : Shaded row means that either removed or allowed at certain limits only SUBSTANCE ACTIVITY Banned Substances 1 Acebutolol Beta blocker 2 Acefylline Bronchodilator 3 Acemetacin NSAID 4 Acenocoumarol Anticoagulant 5 Acetanilid Analgesic/anti-pyretic 6 Acetohexamide Pancreatic stimulant 7 Acetominophen (Paracetamol) Analgesic/anti-pyretic 8 Acetophenazine Antipsychotic 9 Acetylmorphine Narcotic 10 Adinazolam Anxiolytic 11 Adiphenine Anti-spasmodic 12 Adrafinil Stimulant 13 Adrenaline Stimulant 14 Adrenochrome Haemostatic 15 Alclofenac NSAID 16 Alcuronium Muscle relaxant 17 Aldosterone Hormone 18 Alfentanil Narcotic 19 Allopurinol Xanthine oxidase inhibitor (anti-hyperuricaemia) 20 Almotriptan 5 HT agonist (anti-migraine) 21 Alphadolone acetate Neurosteriod 22 Alphaprodine Opiod analgesic 23 Alpidem Anxiolytic 24 Alprazolam Anxiolytic 25 Alprenolol Beta blocker 26 Althesin IV anaesthetic 27 Althiazide Diuretic 28 Altrenogest (in males and gelidngs) Oestrus suppression 29 Alverine Antispasmodic 30 Amantadine Dopaminergic 31 Ambenonium Cholinesterase inhibition 32 Ambucetamide Antispasmodic 33 Amethocaine Local anaesthetic 34 Amfepramone Stimulant 35 Amfetaminil Stimulant 36 Amidephrine Vasoconstrictor 37 Amiloride Diuretic 1 Prohibited Substances List This is the Equine Prohibited Substances List that was voted in at the FEI General Assembly in November 2009 alongside the new Equine Anti-Doping and Controlled Medication Regulations(EADCMR). -

(12) United States Patent (10) Patent No.: US 9,636.405 B2 Tamarkin Et Al
USOO9636405B2 (12) United States Patent (10) Patent No.: US 9,636.405 B2 Tamarkin et al. (45) Date of Patent: May 2, 2017 (54) FOAMABLE VEHICLE AND (56) References Cited PHARMACEUTICAL COMPOSITIONS U.S. PATENT DOCUMENTS THEREOF M (71) Applicant: Foamix Pharmaceuticals Ltd., 1,159,250 A 1 1/1915 Moulton Rehovot (IL) 1,666,684 A 4, 1928 Carstens 1924,972 A 8, 1933 Beckert (72) Inventors: Dov Tamarkin, Maccabim (IL); Doron 2,085,733. A T. 1937 Bird Friedman, Karmei Yosef (IL); Meir 33 A 1683 Sk Eini, Ness Ziona (IL); Alex Besonov, 2,586.287- 4 A 2/1952 AppersonO Rehovot (IL) 2,617,754. A 1 1/1952 Neely 2,767,712 A 10, 1956 Waterman (73) Assignee: EMY PHARMACEUTICALs 2.968,628 A 1/1961 Reed ... Rehovot (IL) 3,004,894. A 10/1961 Johnson et al. (*) Notice: Subject to any disclaimer, the term of this 3,062,715. A 1 1/1962 Reese et al. tent is extended or adiusted under 35 3,067,784. A 12/1962 Gorman pa 3,092.255. A 6/1963 Hohman U.S.C. 154(b) by 37 days. 3,092,555 A 6/1963 Horn 3,141,821 A 7, 1964 Compeau (21) Appl. No.: 13/793,893 3,142,420 A 7/1964 Gawthrop (22) Filed: Mar. 11, 2013 3,144,386 A 8/1964 Brightenback O O 3,149,543 A 9/1964 Naab (65) Prior Publication Data 3,154,075 A 10, 1964 Weckesser US 2013/0189193 A1 Jul 25, 2013 3,178,352. -

Ion Channels
UC Davis UC Davis Previously Published Works Title THE CONCISE GUIDE TO PHARMACOLOGY 2019/20: Ion channels. Permalink https://escholarship.org/uc/item/1442g5hg Journal British journal of pharmacology, 176 Suppl 1(S1) ISSN 0007-1188 Authors Alexander, Stephen PH Mathie, Alistair Peters, John A et al. Publication Date 2019-12-01 DOI 10.1111/bph.14749 License https://creativecommons.org/licenses/by/4.0/ 4.0 Peer reviewed eScholarship.org Powered by the California Digital Library University of California S.P.H. Alexander et al. The Concise Guide to PHARMACOLOGY 2019/20: Ion channels. British Journal of Pharmacology (2019) 176, S142–S228 THE CONCISE GUIDE TO PHARMACOLOGY 2019/20: Ion channels Stephen PH Alexander1 , Alistair Mathie2 ,JohnAPeters3 , Emma L Veale2 , Jörg Striessnig4 , Eamonn Kelly5, Jane F Armstrong6 , Elena Faccenda6 ,SimonDHarding6 ,AdamJPawson6 , Joanna L Sharman6 , Christopher Southan6 , Jamie A Davies6 and CGTP Collaborators 1School of Life Sciences, University of Nottingham Medical School, Nottingham, NG7 2UH, UK 2Medway School of Pharmacy, The Universities of Greenwich and Kent at Medway, Anson Building, Central Avenue, Chatham Maritime, Chatham, Kent, ME4 4TB, UK 3Neuroscience Division, Medical Education Institute, Ninewells Hospital and Medical School, University of Dundee, Dundee, DD1 9SY, UK 4Pharmacology and Toxicology, Institute of Pharmacy, University of Innsbruck, A-6020 Innsbruck, Austria 5School of Physiology, Pharmacology and Neuroscience, University of Bristol, Bristol, BS8 1TD, UK 6Centre for Discovery Brain Science, University of Edinburgh, Edinburgh, EH8 9XD, UK Abstract The Concise Guide to PHARMACOLOGY 2019/20 is the fourth in this series of biennial publications. The Concise Guide provides concise overviews of the key properties of nearly 1800 human drug targets with an emphasis on selective pharmacology (where available), plus links to the open access knowledgebase source of drug targets and their ligands (www.guidetopharmacology.org), which provides more detailed views of target and ligand properties. -

Zebrafish Behavioural Profiling Identifies GABA and Serotonin
ARTICLE https://doi.org/10.1038/s41467-019-11936-w OPEN Zebrafish behavioural profiling identifies GABA and serotonin receptor ligands related to sedation and paradoxical excitation Matthew N. McCarroll1,11, Leo Gendelev1,11, Reid Kinser1, Jack Taylor 1, Giancarlo Bruni 2,3, Douglas Myers-Turnbull 1, Cole Helsell1, Amanda Carbajal4, Capria Rinaldi1, Hye Jin Kang5, Jung Ho Gong6, Jason K. Sello6, Susumu Tomita7, Randall T. Peterson2,10, Michael J. Keiser 1,8 & David Kokel1,9 1234567890():,; Anesthetics are generally associated with sedation, but some anesthetics can also increase brain and motor activity—a phenomenon known as paradoxical excitation. Previous studies have identified GABAA receptors as the primary targets of most anesthetic drugs, but how these compounds produce paradoxical excitation is poorly understood. To identify and understand such compounds, we applied a behavior-based drug profiling approach. Here, we show that a subset of central nervous system depressants cause paradoxical excitation in zebrafish. Using this behavior as a readout, we screened thousands of compounds and identified dozens of hits that caused paradoxical excitation. Many hit compounds modulated human GABAA receptors, while others appeared to modulate different neuronal targets, including the human serotonin-6 receptor. Ligands at these receptors generally decreased neuronal activity, but paradoxically increased activity in the caudal hindbrain. Together, these studies identify ligands, targets, and neurons affecting sedation and paradoxical excitation in vivo in zebrafish. 1 Institute for Neurodegenerative Diseases, University of California, San Francisco, CA 94143, USA. 2 Cardiovascular Research Center and Division of Cardiology, Department of Medicine, Massachusetts General Hospital, Harvard Medical School, Charlestown, MA 02129, USA. -
Public Use Data Tape Documentation 1992 National Ambulatory Medical Care Survey
Public Use Data Ta~e Documentation 1992 National Ambulatory Medical Care Survey From the CENTERS FOR DISEASE CONTROL AND PREVENTION/Nutional Center for Health Stdklics -—..—=-.=-=.-.‘,.- . ----. - . .- -,-- -.-- .--.,. -’ ‘ --- - –.--.------ ,-:-.-,J ----- ---------- ---P ------.-->- — .. ..- --. : _ U.S. DEPARTMENT OF HEALTH AND HUMAN SERVICES Publlc Health Service Centers for Disease Control and Prevention National Center for Health Statistics CDCcE141EmFonmEUEcoumoL WMEmmm Public Use Data Tape Documentation 1992 National Ambulatory Medical Care Survey U.S. DEPARTMENT OF HEALTH AND HUMAN SERVICES Public Health Service Centers for Disease Control and Prevention National Center for Health .SJatistics Hyattsville, Maryland November 1994 299 2 NAMcs MICRO-DATA TAPE Docum NTATION PAGE 1 ABSTRACT This material provides documentation for users of the Micro-Data tapes of the National Ambulatory Medical Care Suney (NAMCS) conducted by the National Center for Health Statistics. Section I, “Description of the National Ambulatory Medical Care Sumey,” includes information on the scope of the amm.rey,the sample, field activities, data collection procedures, medical coding procedures, population estimates, and sampling errors. Section II provides technical detaile of the tape (number of tracks, record length, etc.), and a detailed description of the contents of each data record by location. Section III contains marginal data or estimates for each item on the data record in Section II. The appendixes contain santplingerrors, instructions and definitions for completing the Patient Record Form, and list~ of codes used in the survey. TABLE OF CONTENTS PAGE I. Description of the National Ambulatory Medical Care SuNey 2-14 Distribution of physicians (Table I) 4 Population Figures (Table II) 6 Patient Log and Patient Record Form (Figure 1) 8 References 14 II. -

Valerian Root Valeriana Officinalis L., Radix
5 April 2016 EMA/152385/2016 Herbal medicine: summary for the public Valerian root Valeriana officinalis L., radix This is a summary of the scientific conclusions reached by the Committee on Herbal Medicinal Products (HMPC) on the medicinal uses of valerian root. The HMPC conclusions are taken into account by EU Member States when evaluating applications for the licensing of herbal medicines containing valerian root. This summary is not intended to provide practical advice on how to use medicines containing valerian root. For practical information about using valerian root medicines, patients should read the package leaflet that comes with the medicine or contact their doctor or pharmacist. What is valerian root? Valerian root is the common name for the underground parts of the plant Valeriana officinalis L. The HMPC conclusions only cover valerian root preparations which are obtained by drying and comminuting (reducing into tiny pieces) or powdering the underground parts of the plant, by expressing the juice of the fresh root, and as dry or liquid extracts. Extracts are prepared using a technique to extract compounds by putting the plant material in a solvent (such as ethanol, methanol or water) to dissolve compounds and form a liquid extract. For dry extracts, the solvent is then evaporated off. Herbal medicines containing comminuted valerian root are usually available as herbal tea to be drunk or as bath additives. The other herbal preparations of valerian root are available in solid or liquid form to be taken by mouth. Valerian root preparations may also be found in combination with other herbal substances in some herbal medicines. -

Drug and Medication Classification Schedule
KENTUCKY HORSE RACING COMMISSION UNIFORM DRUG, MEDICATION, AND SUBSTANCE CLASSIFICATION SCHEDULE KHRC 8-020-1 (11/2018) Class A drugs, medications, and substances are those (1) that have the highest potential to influence performance in the equine athlete, regardless of their approval by the United States Food and Drug Administration, or (2) that lack approval by the United States Food and Drug Administration but have pharmacologic effects similar to certain Class B drugs, medications, or substances that are approved by the United States Food and Drug Administration. Acecarbromal Bolasterone Cimaterol Divalproex Fluanisone Acetophenazine Boldione Citalopram Dixyrazine Fludiazepam Adinazolam Brimondine Cllibucaine Donepezil Flunitrazepam Alcuronium Bromazepam Clobazam Dopamine Fluopromazine Alfentanil Bromfenac Clocapramine Doxacurium Fluoresone Almotriptan Bromisovalum Clomethiazole Doxapram Fluoxetine Alphaprodine Bromocriptine Clomipramine Doxazosin Flupenthixol Alpidem Bromperidol Clonazepam Doxefazepam Flupirtine Alprazolam Brotizolam Clorazepate Doxepin Flurazepam Alprenolol Bufexamac Clormecaine Droperidol Fluspirilene Althesin Bupivacaine Clostebol Duloxetine Flutoprazepam Aminorex Buprenorphine Clothiapine Eletriptan Fluvoxamine Amisulpride Buspirone Clotiazepam Enalapril Formebolone Amitriptyline Bupropion Cloxazolam Enciprazine Fosinopril Amobarbital Butabartital Clozapine Endorphins Furzabol Amoxapine Butacaine Cobratoxin Enkephalins Galantamine Amperozide Butalbital Cocaine Ephedrine Gallamine Amphetamine Butanilicaine Codeine -

Interactions with Protease Inhibitors Charts Revised February 2018
www.hiv-druginteractions.org Interactions with Protease Inhibitors Charts revised February 2018. Full information available at www.hiv-druginteractions.org Page 1 of 4 Please note that if a drug is not listed it cannot automatically be assumed it is safe to coadminister. ATV Cobi DRV FPV IDV LPV RTV SQV TPV ATV Cobi DRV FPV IDV LPV RTV SQV TPV Anaesthetics & Muscle Relaxants Antibacterials (continued) Alcuronium Ertapenem Bupivacaine Erythromycin Cisatracurium Ethambutol Desflurane Ethionamide Dexmedetomidine Flucloxacillin Enflurane Gentamicin Ephedrine Imipenem/Cilastatin Halothane Isoniazid Isoflurane Kanamycin Ketamine Levofloxacin Linezolid Nitrous oxide Meropenem Propofol Metronidazole Rocuronium Moxifloxacin Sevoflurane Nitrofurantoin Sufentanil Ofloxacin Suxamethonium (succinylcholine) Para-aminosalicylic acid Tetracaine Penicillins Thiopental for distribution. for Pyrazinamide Tizanidine Rifabutin Vecuronium Rifampicin Analgesics Rifapentine Alfentanil Rifaximin Aspirin Spectinomycin Buprenorphine Streptomycin Celecoxib Sulfadiazine Codeine Telithromycin Tetracyclines