Presentation of Hypoxemia and Cardiorespiratory Compensation in COVID-19 Philip E
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Chapter 22 We Won't Do Much Anatomy Here (Left Column; 22.1-22.3)
Chapter 22 Marieb & Hoehn (2019), p. 8181 We won’t do much anatomy here (left column; 22.1-22.3). Main issues (in lecture and lab): mechanics and measurement of breathing (22.4-22.5), chemoreceptor control of ventilation (22.8), and a few respiratory disorders (22.10). *** Sections 22.6-22.7 were briefly covered in Chapter 17. 1 Ch. 22: Test Question Templates • Q1. If given an appropriate graph of volume of air in lung vs. time, estimate or calculate FEV1/FVC ratio, FVC, residual volume, TLC, tidal volume, and/or minute ventilation. • Example (from Winter 2019 exam): 2 Q1. There are multiple ways to do this. The key is to choose a respiratory rate (breaths per minute) and a tidal volume (milliliters of air per breath) that, when multiplied together, give you 4000 mL air/minute. For example, I can draw a curve to show a tidal volume of 400 mL and a respiratory rate of 10 breaths/minute. Minute ventilation = (tidal volume)*(respiratory rate) = (400 mL air/breath)*(10 breaths/min) = 4000 mL air/min. 2 • Q2. If given two of the three values, calculate the third one: minute ventilation, respiratory rate, and tidal volume. • Example: Lola takes 10 breaths per minute, and her minute ventilation is 6000 mL air per minute. What is her tidal volume? • Q3. If given spirometry data and reference values, determine whether the data are consistent with obstructive pulmonary disease, restrictive pulmonary disease, both, or neither. • Example [from Fall 2019 test]: Rik is put through various pulmonary function tests. At time 0 in the table below, he begins deflating his fully inflated lungs as forcefully and rapidly as he can. -

Hypothermia Brochure
Visit these websites for more water safety and hypothermia prevention in- formation. What is East Pierce Fire & Rescue Hypothermia? www.eastpiercefire.org Hypothermia means “low temperature”. Washington State Drowning When your body is exposed to cold tem- Prevention Coalition Hypothermia www.drowning-prevention.org perature, it tries to protect itself by keeping a normal body temperature of 98.6°F. It Children’s Hospital & tries to reduce heat loss by shivering and Regional Medical Center In Our Lakes moving blood from your arms and legs to www.seattlechildrens.org the core of your body—head, chest and and Rivers abdomen. Hypothermia Prevention, Recognition and Treatment www.hypothermia.org Stages of Hypothermia Boat Washington Mild Hypothermia www.boatwashington.org (Core body temperature of 98.6°— 93.2°F) Symptoms: Shivering; altered judg- ment; numbness; clumsiness; loss of Boat U.S. Foundation dexterity; pain from cold; and fast www.boatus.com breathing. Boat Safe Moderate Hypothermia www.boatsafe.com (Core body temperature of 93.2°—86°F) Symptoms: Semiconscious to uncon- scious; shivering reduced or absent; lips are blue; slurred speech; rigid n in muscles; appears drunk; slow Eve breathing; and feeling of warmth can occur. mer! Headquarters Station Sum Severe Hypothermia 18421 Old Buckley Hwy (Core body temperature below 86°F) Bonney Lake, WA 98391 Symptoms: Coma; heart stops; and clinical death. Phone: 253-863-1800 Fax: 253-863-1848 Email: [email protected] Know the water. Know your limits. Wear a life vest. By choosing to swim in colder water you Waters in Western Common Misconceptions Washington reduce your survival time. -

Job Hazard Analysis
Identifying and Evaluating Hazards in Research Laboratories Guidelines developed by the Hazards Identification and Evaluation Task Force of the American Chemical Society’s Committee on Chemical Safety Copyright 2013 American Chemical Society Table of Contents FOREWORD ................................................................................................................................................... 3 ACKNOWLEDGEMENTS ................................................................................................................................. 5 Task Force Members ..................................................................................................................................... 6 1. SCOPE AND APPLICATION ..................................................................................................................... 7 2. DEFINITIONS .......................................................................................................................................... 7 3. HAZARDS IDENTIFICATION AND EVALUATION ................................................................................... 10 4. ESTABLISHING ROLES AND RESPONSIBILITIES .................................................................................... 14 5. CHOOSING AND USING A TECHNIQUE FROM THIS GUIDE ................................................................. 17 6. CHANGE CONTROL .............................................................................................................................. 19 7. ASSESSING -

Airway Pressures and Volutrauma
Airway Pressures and Volutrauma Airway Pressures and Volutrauma: Is Measuring Tracheal Pressure Worth the Hassle? Monitoring airway pressures during mechanical ventilation is a standard of care.1 Sequential recording of airway pressures not only provides information regarding changes in pulmonary impedance but also allows safety parameters to be set. Safety parameters include high- and low-pressure alarms during positive pressure breaths and disconnect alarms. These standards are, of course, based on our experience with volume control ventilation in adults. During pressure control ventilation, monitoring airway pressures remains important, but volume monitoring and alarms are also required. Airway pressures and work of breathing are also important components of derived variables, including airway resistance, static compliance, dynamic compliance, and intrinsic positive end-expiratory pressure (auto-PEEP), measured at the bedside.2 The requisite pressures for these variables include peak inspiratory pressure, inspiratory plateau pressure, expiratory plateau pressure, and change in airway pressure within a breath. Plateau pressures should be measured at periods of zero flow during both volume control and pressure control ventilation. Change in airway pressure should be measured relative to change in volume delivery to the lung (pressure-volume loop) to elucidate work of breathing. See the related study on Page 1179. Evidence that mechanical ventilation can cause and exacerbate acute lung injury has been steadily mounting.3-5 While most of this evidence has originated from laboratory animal studies, recent clinical reports appear to support this concept.6,7 Traditionally, ventilator-induced lung injury brings to mind the clinical picture of tension pneumothorax. Barotrauma (from the root word baro, which means pressure) is typically associated with excessive airway pressures. -

Approach to Cyanosis in a Neonate.Pdf
PedsCases Podcast Scripts This podcast can be accessed at www.pedscases.com, Apple Podcasting, Spotify, or your favourite podcasting app. Approach to Cyanosis in a Neonate Developed by Michelle Fric and Dr. Georgeta Apostol for PedsCases.com. June 29, 2020 Introduction Hello, and welcome to this pedscases podcast on an approach to cyanosis in a neonate. My name is Michelle Fric and I am a fourth-year medical student at the University of Alberta. This podcast was made in collaboration with Dr. Georgeta Apostol, a general pediatrician at the Royal Alexandra Hospital Pediatrics Clinic in Edmonton, Alberta. Cyanosis refers to a bluish discoloration of the skin or mucous membranes and is a common finding in newborns. It is a clinical manifestation of the desaturation of arterial or capillary blood and may indicate serious hemodynamic instability. It is important to have an approach to cyanosis, as it can be your only sign of a life-threatening illness. The goal of this podcast is to develop this approach to a cyanotic newborn with a focus on these can’t miss diagnoses. After listening to this podcast, the learner should be able to: 1. Define cyanosis 2. Assess and recognize a cyanotic infant 3. Develop a differential diagnosis 4. Identify immediate investigations and management for a cyanotic infant Background Cyanosis can be further broken down into peripheral and central cyanosis. It is important to distinguish these as it can help you to formulate a differential diagnosis and identify cases that are life-threatening. Peripheral cyanosis affects the distal extremities resulting in blue color of the hands and feet, while the rest of the body remains pinkish and well perfused. -

Asphyxia Neonatorum
CLINICAL REVIEW Asphyxia Neonatorum Raul C. Banagale, MD, and Steven M. Donn, MD Ann Arbor, Michigan Various biochemical and structural changes affecting the newborn’s well being develop as a result of perinatal asphyxia. Central nervous system ab normalities are frequent complications with high mortality and morbidity. Cardiac compromise may lead to dysrhythmias and cardiogenic shock. Coagulopathy in the form of disseminated intravascular coagulation or mas sive pulmonary hemorrhage are potentially lethal complications. Necrotizing enterocolitis, acute renal failure, and endocrine problems affecting fluid elec trolyte balance are likely to occur. Even the adrenal glands and pancreas are vulnerable to perinatal oxygen deprivation. The best form of management appears to be anticipation, early identification, and prevention of potential obstetrical-neonatal problems. Every effort should be made to carry out ef fective resuscitation measures on the depressed infant at the time of delivery. erinatal asphyxia produces a wide diversity of in molecules brought into the alveoli inadequately com Pjury in the newborn. Severe birth asphyxia, evi pensate for the uptake by the blood, causing decreases denced by Apgar scores of three or less at one minute, in alveolar oxygen pressure (P02), arterial P02 (Pa02) develops not only in the preterm but also in the term and arterial oxygen saturation. Correspondingly, arte and post-term infant. The knowledge encompassing rial carbon dioxide pressure (PaC02) rises because the the causes, detection, diagnosis, and management of insufficient ventilation cannot expel the volume of the clinical entities resulting from perinatal oxygen carbon dioxide that is added to the alveoli by the pul deprivation has been further enriched by investigators monary capillary blood. -

CARBON MONOXIDE: the SILENT KILLER Information You Should
CARBON MONOXIDE: THE SILENT KILLER Information You Should Know Carbon monoxide is a silent killer that can lurk within fossil fuel burning household appliances. Many types of equipment and appliances burn different types of fuel to provide heat, cook, generate electricity, power vehicles and various tools, such as chain saws, weed eaters and leaf blowers. When these units operate properly, they use fresh air for combustion and vent or exhaust carbon dioxide. When fresh air is restricted, through improper ventilation, the units create carbon monoxide, which can saturate the air inside the structure. Carbon Monoxide can be lethal when accidentally inhaled in concentrated doses. Such a situation is referred to as carbon monoxide poisoning. This is a serious condition that is a medical emergency that should be taken care of right away. What Is It? Carbon monoxide, often abbreviated as CO, is a gas produced by burning fossil fuel. What makes it such a silent killer is that it is odorless and colorless. It is extremely difficult to detect until the body has inhaled a detrimental amount of the gas, and if inhaled in high concentrations, it can be fatal. Carbon monoxide causes tissue damage by blocking the body’s ability to absorb enough oxygen. In fact, poisoning from this gas is one of the leading causes of unintentional death from poison. Common Sources of CO Kerosene or fuel-based heaters Fireplaces Gasoline powered equipment and generators Charcoal grills Automobile exhaust Portable generators Tobacco smoke Chimneys, furnaces, and boilers Gas water heaters Wood stoves and gas stoves Properly installed and maintained appliances are safe and efficient. -

The Hazards of Nitrogen Asphyxiation US Chemical Safety and Hazard Investigation Board
The Hazards of Nitrogen Asphyxiation US Chemical Safety and Hazard Investigation Board Introduction • Nitrogen makes up 78% of the air we breath; because of this it is often assumed that nitrogen is not hazardous. • However, nitrogen is safe to breath only if it is mixed with an appropriate amount of oxygen. • Additional nitrogen (lower oxygen) cannot be detected by the sense of smell. Introduction • Nitrogen is used commercially as an inerting agent to keep material free of contaminants (including oxygen) that may corrode equipment, present a fire hazard, or be toxic. • A lower oxygen concentration (e.g., caused by an increased amount of nitrogen) can have a range of effects on the human body and can be fatal if if falls below 10% Effects of Oxygen Deficiency on the Human Body Atmospheric Oxygen Concentration (%) Possible Results 20.9 Normal 19.0 Some unnoticeable adverse physiological effects 16.0 Increased pulse and breathing rate, impaired thinking and attention, reduced coordination 14.0 Abnormal fatigue upon exertion, emotional upset, faulty coordination, poor judgment 12.5 Very poor judgment and coordination, impaired respiration that may cause permanent heart damage, nausea, and vomiting <10 Inability to move, loss of consciousness, convulsions, death Source: Compressed Gas Association, 2001 Statistics on Incidents CSB reviewed cases of nitrogen asphyxiation that occurred in the US between 1992 and 2002 and determined the following: • 85 incidents of nitrogen asphyxiation resulted in 80 deaths and 50 injuries. • The majority of -

Clinical Management of Severe Acute Respiratory Infections When Novel Coronavirus Is Suspected: What to Do and What Not to Do
INTERIM GUIDANCE DOCUMENT Clinical management of severe acute respiratory infections when novel coronavirus is suspected: What to do and what not to do Introduction 2 Section 1. Early recognition and management 3 Section 2. Management of severe respiratory distress, hypoxemia and ARDS 6 Section 3. Management of septic shock 8 Section 4. Prevention of complications 9 References 10 Acknowledgements 12 Introduction The emergence of novel coronavirus in 2012 (see http://www.who.int/csr/disease/coronavirus_infections/en/index. html for the latest updates) has presented challenges for clinical management. Pneumonia has been the most common clinical presentation; five patients developed Acute Respira- tory Distress Syndrome (ARDS). Renal failure, pericarditis and disseminated intravascular coagulation (DIC) have also occurred. Our knowledge of the clinical features of coronavirus infection is limited and no virus-specific preven- tion or treatment (e.g. vaccine or antiviral drugs) is available. Thus, this interim guidance document aims to help clinicians with supportive management of patients who have acute respiratory failure and septic shock as a consequence of severe infection. Because other complications have been seen (renal failure, pericarditis, DIC, as above) clinicians should monitor for the development of these and other complications of severe infection and treat them according to local management guidelines. As all confirmed cases reported to date have occurred in adults, this document focuses on the care of adolescents and adults. Paediatric considerations will be added later. This document will be updated as more information becomes available and after the revised Surviving Sepsis Campaign Guidelines are published later this year (1). This document is for clinicians taking care of critically ill patients with severe acute respiratory infec- tion (SARI). -

Respiratory and Gastrointestinal Involvement in Birth Asphyxia
Academic Journal of Pediatrics & Neonatology ISSN 2474-7521 Research Article Acad J Ped Neonatol Volume 6 Issue 4 - May 2018 Copyright © All rights are reserved by Dr Rohit Vohra DOI: 10.19080/AJPN.2018.06.555751 Respiratory and Gastrointestinal Involvement in Birth Asphyxia Rohit Vohra1*, Vivek Singh2, Minakshi Bansal3 and Divyank Pathak4 1Senior resident, Sir Ganga Ram Hospital, India 2Junior Resident, Pravara Institute of Medical Sciences, India 3Fellow pediatrichematology, Sir Ganga Ram Hospital, India 4Resident, Pravara Institute of Medical Sciences, India Submission: December 01, 2017; Published: May 14, 2018 *Corresponding author: Dr Rohit Vohra, Senior resident, Sir Ganga Ram Hospital, 22/2A Tilaknagar, New Delhi-110018, India, Tel: 9717995787; Email: Abstract Background: The healthy fetus or newborn is equipped with a range of adaptive, strategies to reduce overall oxygen consumption and protect vital organs such as the heart and brain during asphyxia. Acute injury occurs when the severity of asphyxia exceeds the capacity of the system to maintain cellular metabolism within vulnerable regions. Impairment in oxygen delivery damage all organ system including pulmonary and gastrointestinal tract. The pulmonary effects of asphyxia include increased pulmonary vascular resistance, pulmonary hemorrhage, pulmonary edema secondary to cardiac failure, and possibly failure of surfactant production with secondary hyaline membrane disease (acute respiratory distress syndrome).Gastrointestinal damage might include injury to the bowel wall, which can be mucosal or full thickness and even involve perforation Material and methods: This is a prospective observational hospital based study carried out on 152 asphyxiated neonates admitted in NICU of Rural Medical College of Pravara Institute of Medical Sciences, Loni, Ahmednagar, Maharashtra from September 2013 to August 2015. -

Effects of Anaesthesia Techniques and Drugs on Pulmonary Function
Review Article Effects of anaesthesia techniques and drugs on pulmonary function Address for correspondence: Vijay Saraswat Dr. Vijay Saraswat, Department of Anaesthesiology, Apollo Hospitals, Nashik, Maharashtra, India Apollo Hospitals, Nashik, Maharashtra, India. E‑mail: drvsaraswat@gmail. ABSTRACT com The primary task of the lungs is to maintain oxygenation of the blood and eliminate carbon dioxide through the network of capillaries alongside alveoli. This is maintained by utilising ventilatory reserve capacity and by changes in lung mechanics. Induction of anaesthesia impairs pulmonary functions by the loss of consciousness, depression of reflexes, changes in rib cage and haemodynamics. All drugs used during anaesthesia, including inhalational agents, affect pulmonary functions directly by acting on respiratory system or indirectly through their actions on other systems. Volatile anaesthetic agents have more pronounced effects on pulmonary functions compared to intravenous induction agents, leading to hypercarbia and hypoxia. The posture of the patient also leads to major changes in pulmonary functions. Anticholinergics and neuromuscular blocking agents have little effect. Analgesics and Access this article online sedatives in combination with volatile anaesthetics and induction agents may exacerbate Website: www.ijaweb.org their effects. Since multiple agents are used during anaesthesia, ultimate effect may be DOI: 10.4103/0019‑5049.165850 different from when used in isolation. Literature search was done using MeSH key words ‘anesthesia’, -
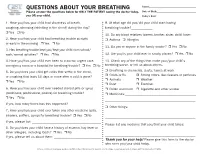
QUESTIONS ABOUT YOUR BREATHING Name:______Please Answer the Questions Below for ONLY the PATIENT Seeing the Doctor Today, Date of Birth:______You OR Your Child
QUESTIONS ABOUT YOUR BREATHING Name:_____________________________________ Please answer the questions below for ONLY THE PATIENT seeing the doctor today, Date of Birth:_______________________________ you OR your child. Today’s Date:_______________________________ 1. Have you/has your child had shortness of breath, 9. At what age did you/did your child start having coughing, wheezing (whistling in the chest) during the day? breathing trouble?_____________ r Yes r No 10. Do any blood relatives (parent, brother, sister, child) have: 2. Have you/has your child had breathing trouble at night r Asthma r Allergies or early in the morning r Yes r No 11. Do you or anyone in the family smoke? r Yes r No 3. Has breathing trouble kept you/kept your child from school/ work/normal activities? r Yes r No 12. Are you/is your child ever in smoky places? r Yes r No 4. Have you/has your child ever been to a doctor, urgent care, 13. Check any of the things that make your/your child’s emergency room or a hospital for breathing trouble? r Yes r No breathing worse, or tell us about others. 5. Do you/does your child get colds that settle in the chest, r Breathing in chemicals, dusts, fumes at work r Colds or flu r Strong odors, like cleaners or perfumes or coughing that lasts 10 days or more after a cold is gone? r Animals r Weather r Yes r No r Dust r Exercise 6. Have you/has your child ever needed steroid pills or syrup r Pollen and mold r Cigarette and other smoke (prednisone, prednisolone, prelone) for breathing trouble? r Medicines:___________________________________________ r Yes r No _______________________________________________________ If yes, how many times has this happened? ___________________ r Other things: 7.