Dietary Glycemic Index and Load and the Risk of Type 2 Diabetes: Assessment of Causal Relations
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Cell Function the Hyperbolic Correction Richard N
Accurate Assessment of -Cell Function The Hyperbolic Correction Richard N. Bergman, Marilyn Ader, Katrin Huecking, and Gregg Van Citters Only in the last decade did modeling studies predict, and knockout experiments confirm, that type 2 diabetes is a “2-hit” disease in which insulin resistance is necessarily efective function of the pancreatic -cells is accompanied by -cell defect(s) preventing the compen- now accepted to be a hallmark of type 1 and satory upregulation of insulin secretion. This long- type 2 diabetes. The importance of the -cells in delayed insight was associated with the development of type 1 diabetes has long been accepted. On the a constant, the “disposition index,” describing the D contrary, the necessity of a pancreatic defect in type 2 -cell sensitivity-secretion relationship as a rectangular hyperbola. Shifts in insulin sensitivity are accompanied diabetes has only recently been widely appreciated (1,2). by compensatory alterations in -cell sensitivity to For many years, it was considered that insulin resistance glucose. Insulin-sensitive subjects do not require a alone could engender hyperglycemia in those without massive insulin response to exogenous glucose to main- immune etiology of disease (3,4). Results based on mod- tain a normal blood glucose. But if their insulin sensi- eling indicating that -cell upregulation would compensate tivity decreases by 80%, as in late pregnancy, they need for even severe insulin resistance and not result in fasting a fivefold greater insulin response to achieve an identi- hyperglycemia (5) were recently supported by the labora- cal disposition index. Women with gestational diabetes tory of C.R. -

Methods for Measuring Risk for Type 2 Diabetes in Youth: the Oral Glucose Tolerance Test
Methods for Measuring Risk for Type 2 Diabetes in Youth: The Oral Glucose Tolerance Test (OGTT) Melinda E. Chen, MD1, Rebecca S. Aguirre, MD, PhD2, and Tamara S. Hannon, MD, MS 1University of Nebraska Medical Center; 2Indiana University School of Medicine Corresponding Author: Tamara S. Hannon 705 Riley Hospital Drive, Room 5960, Indianapolis, IN 46202 Email: [email protected] Keywords: insulin sensitivity; β-cell function; prediabetes; adolescent; pediatric Abstract Purpose of review: The oral glucose tolerance test (OGTT) is used both in clinical practice and research to assess glucose tolerance. In addition, the OGTT is utilized for surrogate measures of insulin sensitivity and the insulin response to enteral glucose, and has been widely applied in the evaluation of β-cell dysfunction in obesity, prediabetes, and type 2 diabetes. Here we review the use of the OGTT and the OGTT-derived indices for measurement of risk markers for type 2 diabetes in youth. Recent findings: Advantages of using the OGTT for measures of diabetes risk include its accessibility and the incorporation of physiological contributions of the gut-pancreas axis in the measures of insulin response to glucose. Mathematical modeling expands the potential gains from the OGTT in physiology and clinical research. Disadvantages include individual differences in the rate of glucose absorption that modify insulin responses, imperfect control of the glycemic stimulus, and poor intraindividual reproducibility. ___________________________________________________________________ This is the author's manuscript of the article published in final edited form as: Chen, M. E., Aguirre, R. S., & Hannon, T. S. (2018). Methods for Measuring Risk for Type 2 Diabetes in Youth: the Oral Glucose Tolerance Test (OGTT). -

GRAINS of TRUTH for DIABETES by Jeanne Brown, RD,CDE, LD
GRAINS OF TRUTH FOR DIABETES By Jeanne Brown, RD,CDE, LD Avoiding pasta to lower your blood sugar? Wondering how to identify whole grains? Does the glycemic index (GI) of grains matter? Here are some grains of truth for diabetes. Whole grains provide fiber, vitamins, minerals, antioxidants and in general have a lower GI which reduces the risk of diabetes. Researchers have found a 30 % lower risk of diabetes with high fiber diets from grains. People who eat at least 2 servings per week of brown rice have a 11% lower risk of Type 2 Diabetes than those that eat less. The risk of getting Type 2 Diabetes was 2 ½ times greater for people who had the highest glycemic load and lowest fiber intake in the study. The GI measures how a carbohydrate- containing food raises blood sugar. The GI ranges from 0 to 100. The higher the number, the more likely it will raise blood sugars. The GI is also affected by how the food is processed, how it is cooked and the ripeness of fruit. Pasta cooked just until it is firm and chewy has a lower GI than overcooked pasta. A ripe banana will spike blood sugar more than an unripe banana. Tips: Look for the word “WHOLE” grain. “Whole” ensures they used the entire grain which includes the fiberous bran, and nutrient dense germ. “Wheat bread” or “wheat flour” is not necessarily whole grain unless it states “whole wheat" in the beginning of the ingredient list. Products such as: 100% whole wheat bread, shredded wheat cereal and Triscuit crackers are 100 % whole grains. -

A Dozen Tips for Better Blood Sugar Control: Glycemic Index And
A Dozen Tips for Better Blood Sugar Control: Glycemic Index and Glycemic Load Human bodies depend on a steady supply of glucose (blood sugar) as their principal fuel, in order for muscles to stretch and contract, nerves to fire, brains to function—and so much more. Glucose comes from carbohydrates, so the quality and quantity of carbohydrates we eat hugely impacts our energy levels and overall health. Too little glucose, and we starve many bodily functions (especially the brain, which uses 11–20% of the glucose we produce). Too much, and our body scrambles to produce enough insulin to process all that blood sugar—and we may develop heart disease, eye, kidney, and nerve damage. Ideally, our food delivers a steady stream of just the right amount of glucose. But how do we distinguish foods, meals, and diets that raise our blood sugar too high and too fast from those that dole out their fuel slowly and steadily to support good health? Understanding glycemic index, glycemic load and glycemic response can help. Glycemic Index (GI) ranks the quality of individual carbohydrate-rich foods on a scale of 1–100 by measuring how glucose levels rise after someone eats an amount of that food containing 50 grams of carbohydrate. Foods with a low GI score (under 55) provide steady fuel to support energy levels and overall health, while those with a high GI score (70 and up) are likely to provide an unhealthy quick rush of blood sugar followed by a sharp crash. Glycemic Load (GL) combines quality and quantity, allowing us to rank how the typical serving size of a food affects blood sugar. -

Effect of Glycemic Index and Glycemic Load on Type 2 Diabetes Mellitus
International Journal of Health Sciences and Research www.ijhsr.org ISSN: 2249-9571 Review Article Effect of Glycemic Index and Glycemic Load on Type 2 Diabetes Mellitus Towhid Hasan1, Marjia Sultana1, Lincon Chandra Shill1, Nafisa Habib Purba1, Sara Sultana2 1Department of Food Technology and Nutrition Science, Noakhali Science and Technology University, Noakhali-3814, Bangladesh 2Department of Pharmacy, University of Dhaka, Dhaka-1000, Bangladesh Corresponding Author: Marjia Sultana ABSTRACT Worldwide diabetes mellitus especially type 2 diabetes mellitus (T2DM) has become a common and rapidly growing chronic non-communicable disease with potentially devastating complications, posing major public health and socioeconomic challenges. The role of glycemic index (GI) and glycemic load (GL) in the control of the T2DM remain controversial. However, a number of mechanisms have been proposed through which dietary GI and/or GL can reduce the risk of T2DM, but all are suggestive. So, the present review is aimed to investigate the current understanding of the effect of GI and/or GL on the risk of T2DM.PubMed, Google Scholar, Cochrane library and several other databases were searched up to December 2018 to identify and select relevant studies. Research conducted using human are only considered eligible. Among the eighteen prospective cohort studies, eight have found no significant association of dietary GI and/or GL with T2DM risk, six studies revealed an association and four studies identified positive association only with GI but not with the GL. Among the ten interventional studies, only two indicated that the risk of T2DM increased with the increment of GI and GL. In conclusion, research on the glycemic response of foods needs to be expanded in order to get a broad and clear knowledge which will provide assurance that how dietary GI and/or GL have play role on the risk of T2DM. -

Dietary Glycemic Index, Glycemic Load, Fiber, Simple Sugars, and Insulin Resistance the Inter99 Study
Pathophysiology/Complications ORIGINAL ARTICLE Dietary Glycemic Index, Glycemic Load, Fiber, Simple Sugars, and Insulin Resistance The Inter99 study 1,2 1,4 CATHRINE LAU, MSC OLUF PEDERSEN, MD, DMSC he rising prevalence of disorders as- 1,2 1 KRISTINE FÆRCH, MSC BENDIX CARSTENSEN, MSC sociated with insulin resistance, 1,3 3 CHARLOTTE GLUMER¨ , MD, PHD TORBEN JØRGENSEN, MD, DMSC 2 1 including type 2 diabetes, cardio- NGE ETENS MSC, PHD NUT ORCH OHNSEN MD, DMSC T I T , K B -J , vascular disease, and the metabolic syn- drome, is commonly attributed to changes over time in dietary patterns and physical activity levels (1–4). Preventive strategies against these disorders, therefore, often in- OBJECTIVE — To examine the relationship between daily glycemic index, daily glycemic corporate dietary recommendations. How- load, simple sugars, dietary fiber, and the prevalence of a measure of insulin resistance in 30- to 60-year-old nondiabetic Danish men and women. ever, only few observational studies have investigated the independent effects of car- RESEARCH DESIGN AND METHODS — The Inter99 study is a nonpharmacological bohydrate-related dietary factors and obe- intervention study. We used baseline data and examined cross-sectional associations between sity on the degree of insulin resistance. The carbohydrate-related dietary factors and an estimate of insulin resistance in 5,675 subjects at official carbohydrate-related recommen- 30–60 years. The dietary intake was estimated from a self-administered food frequency ques- dations are high intake of fiber-rich car- tionnaire, and insulin resistance was estimated using the homeostasis model assessment of bohydrates (Ͼ55 E% [energy percent] insulin resistance (HOMA-IR). -

POTATOES and the GLYCEMIC INDEX How to Reduce the GI of Potatoes and Gain the Benefits of Resistant Starch
POTATOES AND THE GLYCEMIC INDEX How to reduce the GI of potatoes and gain the benefits of resistant starch Potatoes are a highly nutritious wholefood. They contribute a range of nutrients associated with good health, including fibre, vitamin B6, vitamin C, potassium and phytonutrients. You might also be surprised to know that potatoes can have a lower glycemic index (GI) than you might think. What is the Glycemic Index? The GI is a measure of the speed at which a food makes blood sugar rise. AT A GLANCE GI is calculated by measuring the change in blood glucose (BGL) over a The GI of potatoes is two-hour period after eating a 50 gram carbohydrate portion of a single food relative to the change in blood glucose after eating a 50g carbohydrate influenced by: portion of a reference food (glucose or white bread). • Variety of potato (and its carbohydrate, fibre and When it is not possible to measure this directly, GI tables are used to provide polyphenol content) an estimate of BGL response, however, there are large fluctuations in BGL response to foods both within and between individuals. • Serving size The lower a food’s GI, the slower BGLs rise after eating that food. There are • Cooking method/preparation many factors affecting GI in nuts and potatoes. GI less than 55 is considered and storage low, 56-69 moderate and 70+ high. • Fibre and resistant starch content (higher amounts = To better understand a food’s effect on BGLs, you need to know how quickly lower GI, leave the skin on) its glucose enters the bloodstream and how much glucose per serving it can deliver. -

Low–Glycemic Index Diets in the Management of Diabetes a Meta-Analysis of Randomized Controlled Trials
Clinical Care/Education/Nutrition ORIGINAL ARTICLE Low–Glycemic Index Diets in the Management of Diabetes A meta-analysis of randomized controlled trials 1 2 JENNIE BRAND-MILLER, PHD PETER PETOCZ, PHD ticularly with regard to the glycemic in- 2 3 SUSAN HAYNE, BSC STEPHEN COLAGIURI, MD dex (GI) of foods (5). Current dietary recommendations emphasize the quantity rather than the quality of carbohydrate, despite the fact that carbohydrate source and nature pro- OBJECTIVE — The use of diets with low glycemic index (GI) in the management of diabetes foundly influence postprandial glycemia is controversial, with contrasting recommendations around the world. We performed a meta- (6,7). Research on GI indicates that even analysis of randomized controlled trials to determine whether low-GI diets, compared with conventional or high-GI diets, improved overall glycemic control in individuals with diabetes, as when foods contain the same amount of assessed by reduced HbA or fructosamine levels. carbohydrate (i.e., carbohydrate ex- 1c changes), there are up to fivefold differ- RESEARCH DESIGN AND METHODS — Literature searches identified 14 studies, ences in glycemic impact (8). In addition, comprising 356 subjects, that met strict inclusion criteria. All were randomized crossover or several prospective observational studies parallel experimental design of 12 days’ to 12 months’ duration (mean 10 weeks) with modifi- have found that the overall GI and glyce- cation of at least two meals per day. Only 10 studies documented differences in postprandial mic load (GI ϫ g carbohydrate) of the glycemia on the two types of diet. diet, but not total carbohydrate content, are independently related to the risk of RESULTS — Low-GI diets reduced HbA by 0.43% points (CI 0.72–0.13) over and above 1c developing type 2 diabetes (9,10), cardio- that produced by high-GI diets. -

Adjusting Glucose-Stimulated Insulin Secretion for Adipose Insulin
Diabetes Care 1 Steven K. Malin,1,2 Sangeeta R. Kashyap,3 Adjusting Glucose-Stimulated Jeff Hammel,1 Yoshi Miyazaki,4 CLIN CARE/EDUCATION/NUTRITION/PSYCHOSOCIAL Ralph A. DeFronzo,4 and Insulin Secretion for Adipose John P. Kirwan1,2,5 Insulin Resistance: An Index of b-Cell Function in Obese Adults DOI: 10.2337/dc13-3011 OBJECTIVE The hyperbolic relationship between insulin secretion and sensitivity has been used to assess in vivo b-cell function (i.e., the disposition index). The disposition index emphasizes the importance of taking into account both skeletal muscle and hepatic insulin resistance to depict insulin secretion. However, we propose that adipose tissue insulin resistance also needs to be accounted for when character- izing glucose-stimulated insulin secretion (GSIS) because elevated plasma free fatty acids (FFAs) impair b-cell function. RESEARCH DESIGN AND METHODS To characterize the adipose disposition index, we used [1-14C] palmitate infusion to determine basal FFA turnover rate/adipose insulin resistance and an oral glu- cose tolerance test to characterize the first (i.e., 0–30 min) and second phase (i.e., 60–120 min) of GSIS. We validated a simplified version of the tracer infusion calculation as the product of (1/plasma FFA concentration 3 plasma insulin con- centration) 3 GSIS in 44 obese insulin-resistant subjects. RESULTS The plasma FFA and palmitate tracer infusion calculations of the first- and second- phase disposition index were strongly correlated (r = 0.86, P < 0.000001 and r = 0.89, P < 0.000001, respectively). The first- and second-phase adipose disposition 1Department of Pathobiology, Lerner Research index derived from plasma FFA also was tightly associated with fasting hypergly- Institute, Cleveland Clinic, Cleveland, OH 2 cemia (r = 20.87, P < 0.00001 and r = 20.89, P < 0.00001, respectively) and 2-h Department of Nutrition, School of Medicine, r 2 P < r 2 P < Case Western Reserve University, Cleveland, OH glucose concentrations ( = 0.86, 0.00001 and = 0.90, 0.00001). -

Dietary Patterns, Foods and Nutrients, and Health Outcomes What Is The
Appendix E-2.27: Evidence Portfolio Appendix E2.27: Evidence Portfolio Part D. Chapter 2: Dietary Patterns, Foods and Nutrients, and Health Outcomes What is the relationship between dietary patterns and measures of body weight or obesity? Conclusion Statement: The DGAC concurs with the 2013 AHA/ACC/TOS Guideline for the Management of Overweight and Obesity1 that strong evidence demonstrates that, preferably as part of a comprehensive lifestyle intervention carried out by multidisciplinary teams of professionals or nutrition professionals, overweight and obese adults can achieve weight loss through a variety of dietary patterns that achieve an energy deficit. Clinically meaningful weight losses that were achieved ranged from 4 to 12 kg at 6-month follow-up. Thereafter, slow weight regain is observed, with total weight loss at 1 year of 4 to 10 kg and at 2 years of 3 to 4 kg. However, some dietary patterns may be more beneficial in the long-term for cardiometabolic health. DGAC Grade: Strong The DGAC concurs with the NEL Dietary Patterns Systematic Review Project2 that moderate evidence indicates dietary patterns that are higher in vegetables, fruits, and whole grains; include seafood and legumes; are moderate in dairy products (particularly low and non-fat dairy) and alcohol; lower in meats (including red and processed meats), and low in sugar-sweetened foods and beverages, and refined grains are associated with favorable outcomes related to healthy body weight (including lower BMI, waist circumference, or percent body fat) or risk of obesity. Components of the dietary patterns associated with these favorable outcomes include higher intakes of unsaturated fats and lower intakes of saturated fats, cholesterol, and sodium. -
Glycemic Index
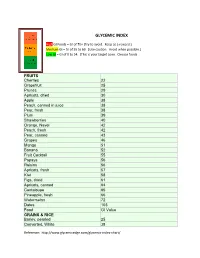
GLYCEMIC INDEX High GI Foods = GI of 70+ (Try to avoid. Keep as a reward.) Medium GI = GI of 55 to 69. (Use caution. Avoid when possible.) Low GI = GI of 0 to 54. (This is your target zone. Choose foods FRUITS Cherries 22 Grapefruit 25 Prunes 29 Apricots, dried 30 Apple 38 Peach, canned in juice 38 Pear, fresh 38 Plum 39 Strawberries 40 Orange, Navel 42 Peach, fresh 42 Pear, canned 43 Grapes 46 Mango 51 Banana 52 Fruit Cocktail 55 Papaya 56 Raisins 56 Apricots, fresh 57 Kiwi 58 Figs, dried 61 Apricots, canned 64 Cantaloupe 65 Pineapple, fresh 66 Watermelon 72 Dates 103 Food GI Value GRAINS & RICE Barley, pearled 25 Converted, White 38 Reference: http://www.glycemicedge.com/glycemic-index-chart/ Long grain, White 44 Buckwheat 54 Brown 55 Basmati 58 Couscous 65 Cornmeal 68 Aborio 69 Short grain, White 72 Instant, White 87 Wild rice 87 Glutinous (Sticky) 98 BEANS & PEAS GI Value Chana Dal 8 Chickpeas, dried 28 Kidney Beans, dried 28 Lentils 29 Lima Beans (frozen) 32 Yellow Split Peas 32 Chickpeas, canned 42 Blackeyed Peas, canned 42 Baked Beans 48 Kidney Beans, canned 52 VEGETABLES Broccoli 10 Cabbage 10 Lettuce 10 Mushrooms 10 Onions 10 Red Peppers 10 Carrots 49 Green peas 48 Corn, fresh 60 Beets 64 Pumpkin 75 Parsnips 97 DAIRY Yogurt, artificially sweetened 14 Whole milk 31 Skim milk 32 Yogurt, sweetened 33 Ice cream, premium 38 Reference: http://www.glycemicedge.com/glycemic-index-chart/ Ice cream, low fat 43 SWEETNER Glucose 96 Fructose 22 Lactose 46 Sucrose (white sugar) 64 Brown sugar 64 Barley malt syrup 42 Brown rice syrup 25 Raw honey 30 Agave syrup 15 High fructose corn syrup 62 Stevia less than 1 Sugar cane juice 43 Evaporated cane juice 55 Maple syrup 54 Black strap molasses 55 The materials and content contained on this form are for general holistic nutrition information only to help support and enhance the body’s own healing properties and are not intended to be a substitute for professional medical advice, diagnosis or treatment for any medical condition. -

A Review of the Relationship Between Dietary Glycemic Index and Glycemic Load and Type 2 Diabetes
eISSN: 2476-7425 pISSN: 2476-7417 JNFS 2016; 1 (1): 73-79 Website: jnfs.ssu.ac.ir A Review of the Relationship between Dietary Glycemic Index and Glycemic Load and Type 2 Diabetes 1,2 3 4 Fahime Zeinali; MSc , Hadis Asadi Samani; BSc , Omid Toupchian; PhD , Shima Abdollahi; MSc1,2 & Mehnoosh Samadi; MSc*3 1 Nutrition and Food Security Research Center, Shahid Sadoughi University of Medical Sciences, Yazd, Iran. 2 Department of Nutrition, School of Public Health, Shahid Sadoughi University of Medical Sciences, Yazd, Iran. 3 Student Research Committee, Ahvaz Jundishapur University of Medical Sciences, Ahvaz, Iran 4 Department of Cellular and Molecular Nutrition, School of Nutritional Sciences and Dietetics, Tehran University of Medical Sciences, Tehran, Iran. ARTICLE INFO ABSTRACT REVIEW ARTICLE Background: In recent decades, studies on type 2 diabetes (T2D), have adopted a new approach to the field of a more complete collection of variables Article history: related to the lifestyles and diet of people. Diet is an important factor in Received: 9 Apr 2016 increasing the rate of T2D among individuals. Considering the consumption of Revised: 5 Jun 2016 a high-carbohydrate diet, little attention has been paid to the type of Accepted: 24 Jul 2016 carbohydrates consumed in the incidence of T2D. The present study aimed to review the literature on the relationship between the glycemic index (GI), the glycemic load, (GL) and T2D, it also targets at evaluating and comparing the *Corresponding author: results of similar studies in other countries Methods: Using search engines, Downloaded from jnfs.ssu.ac.ir at 11:48 IRST on Saturday October 2nd 2021 Student Research Committee, including PubMed, Science Direct, Embase and Scopus, and key words such Ahvaz Jundishapur University as GI, GL, diabetes; articles with cross-sectional, clinical trial, Prospective and of Medical Sciences, Ahvaz, retrospective cohort designs between 2000 to 2016 were selected.