Measurement of Cystatin C in Dried Blood Spot Specimens
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

A Guide to Transthyretin Amyloidosis
A Guide to Transthyretin Amyloidosis Authored by Teresa Coelho, Bo-Goran Ericzon, Rodney Falk, Donna Grogan, Shu-ichi Ikeda, Mathew Maurer, Violaine Plante-Bordeneuve, Ole Suhr, Pedro Trigo 2016 Edition Edited by Merrill Benson, Mathew Maurer What is amyloidosis? Amyloidosis is a systemic disorder characterized by extra cellular deposition of a protein-derived material, known as amyloid, in multiple organs. Amyloidosis occurs when native or mutant poly- peptides misfold and aggregate as fibrils. The amyloid deposits cause local damage to the cells around which they are deposited leading to a variety of clinical symptoms. There are at least 23 different proteins associated with the amyloidoses. The most well-known type of amyloidosis is associated with a hematological disorder, in which amyloid fibrils are derived from monoclonal immunoglobulin light-chains (AL amyloidosis). This is associated with a clonal plasma cell disorder, closely related to and not uncommonly co-existing with multiple myeloma. Chronic inflammatory conditions such as rheumatoid arthritis or chronic infections such as bronchiectasis are associated with chronically elevated levels of the inflammatory protein, serum amyloid A, which may misfold and cause AA amyloidosis. The hereditary forms of amyloidosis are autosomal dominant diseases characterized by deposition of variant proteins, in dis- tinctive tissues. The most common hereditary form is transthyretin amyloidosis (ATTR) caused by the misfolding of protein monomers derived from the tetrameric protein transthyretin (TTR). Mutations in the gene for TTR frequently re- sult in instability of TTR and subsequent fibril formation. Closely related is wild-type TTR in which the native TTR protein, particu- larly in the elderly, can destabilize and re-aggregate causing non- familial cases of TTR amyloidosis. -

Frequency of Renal Monitoring – Creatinine and Cystatin C): an Observational Cohort Study of Primary Care Patients with Reduced Egfr
Accepted Manuscript British Journal of General Practice FORM-2C (Frequency of Renal Monitoring – Creatinine and Cystatin C): An observational cohort study of primary care patients with reduced eGFR Fleming, Susannah; Perera, Rafael; Taylor, Kathryn; Jones, Louise; Hobbs, FD Richard; James, Tim; O’Callaghan, Chris; Shine, Brian; Verbakel, Jan ; Stevens, Richard; Bankhead, Clare DOI: https://doi.org/10.3399/BJGP.2020.0940 To access the most recent version of this article, please click the DOI URL in the line above. Received 19 October 2020 Revised 15 March 2021 Accepted 07 April 2021 © 2021 The Author(s). This is an Open Access article distributed under the terms of the Creative Commons Attribution 4.0 License (http://creativecommons.org/licenses/by/4.0/). Published by British Journal of General Practice. For editorial process and policies, see: https://bjgp.org/authors/bjgp-editorial-process-and-policies When citing this article please include the DOI provided above. Author Accepted Manuscript This is an ‘author accepted manuscript’: a manuscript that has been accepted for publication in British Journal of General Practice, but which has not yet undergone subediting, typesetting, or correction. Errors discovered and corrected during this process may materially alter the content of this manuscript, and the latest published version (the Version of Record) should be used in preference to any preceding versions Title page FORM-2C (Frequency of Renal Monitoring – Creatinine and Cystatin C): An observational cohort study of primary care patients -

Distinct Human Prolactin (Hprl) and Growth Hormone (Hgh)
Available online at www.sciencedirect.com Journal of Biotechnology 133 (2008) 27–35 Distinct human prolactin (hPRL) and growth hormone (hGH) behavior under bacteriophage lambda PL promoter control: Temperature plays a major role in protein yields C.R.J. Soares ∗, E.K.M. Ueda, T.L. Oliveira, F.I.C. Gomide, S.R. Heller, P. Bartolini Biotechnology Department, IPEN-CNEN, Av. Lineu Prestes, 2242 Cidade Universit´aria, 05508-900 S˜ao Paulo, Brazil Received 6 February 2007; received in revised form 21 August 2007; accepted 24 August 2007 Abstract When producing recombinant protein for therapy, it is desirable not only to obtain substantial amounts of the protein, but also to make sure that potential contaminants such as inducing agents are not present in the final product. To prevent this, one can use expression systems in which the promoter (PL) is activated by a temperature shift that denatures a repressor (e.g., cIts). In this manner, hGH was successfully expressed and −1 −1 ◦ secreted in Escherichia coli periplasm, with specific yields well above 1 gml A600, after a temperature shift from 30 to 42 C. However, attempts −1 −1 to express a related hormone, human prolactin, employing the same protocol were unsuccessful, providing 0.03 gml A600 at the most. A process is described in which this labile protein is obtained from a cIts− strain under optimized temperature condition (37 ◦C). The highest periplasmic ± −1 −1 ∼ secretions of prolactin ever reported were thus obtained: 0.92 0.10 gml A600 at an optical density of 3A600 units in shake flask cultures and ∼ −1 −1 1 gml A600,atanODof35A600 units, via a rapid and flexible batch feed process in laboratory bioreactor. -

Cystatin C: a Potential Target for Alzheimers Treatment
Editorial Cystatin C: a potential target for Alzheimer’s treatment Expert Rev. Neurotherapeutics 8(5), 687–689 (2008) Efrat Levy “…cystatin C binds soluble Aβ and inhibits Aβ oligomerization Departments of and amyloidogenesis, protecting the brain against Psychiatry & Pharmacology, amyloid-induced toxicity.” New York University School of Medicine, Alzheimer's disease is one of the most in familial Alzheimer’s disease in the Nathan S. Kline prevalent chronic diseases of the aging brains of mice results in amyloid plaque Institute, 140 Old population. Neuropathologically, the deposition. Some proteins associated Orangeburg Road, Orangeburg, disease is characterized by neurodegener- with amyloid lesions may have a role in NY 10962, USA ation and the presence of two patho- the pathological processes leading to Tel.: +1 845 398 5540 logical features, amyloid plaques and amyloidogenesis and neuronal degenera- Fax: +1 845 398 5422 neurofibrillary tangles. Amyloid-β (Aβ) tion, and others may bind secondarily to [email protected] is the major constituent of the amyloid amyloid deposits. It was demonstrated plaques. It is a ubiquitously expressed that cystatin C binds to the Aβ region soluble peptide that can form aggregates, within full-length amyloid precursor pro- either oligomeric or fibrillar, that are tein and that this association does not neurotoxic. Extensive research focuses on affect Aβ generation either in vitro [10] or prevention of Aβ aggregation as a possi- in vivo [11]. The association of cystatin C ble therapy for the disease. Recent stud- with the amyloid precursor protein was ies have shown that the endogenous pro- recently confirmed by in vivo mapping of tein cystatin C binds soluble Aβ and protein interactions in intact mouse inhibits Aβ oligomerization and amyloido- tissue [12]. -
Higher Plasma Cystatin C Is Associated with Mortality After Acute
Hendrickson et al. Critical Care (2020) 24:416 https://doi.org/10.1186/s13054-020-03111-1 RESEARCH Open Access Higher plasma cystatin C is associated with mortality after acute respiratory distress syndrome: findings from a Fluid and Catheter Treatment Trial (FACTT) substudy Carolyn M. Hendrickson1* , Yuenting D. Kwong2, Annika G. Belzer3, Michael G. Shlipak4,5, Michael A. Matthay6,7 and Kathleen D. Liu6,7 Abstract Background: Cystatin C is a well-validated marker of glomerular filtration rate in chronic kidney disease. Higher plasma concentrations of cystatin C are associated with worse clinical outcomes in heterogenous populations of critically ill patients and may be superior to creatinine in identifying kidney injury in critically ill patients. We hypothesized that elevated levels of plasma cystatin C in patients with acute respiratory distress syndrome (ARDS) would be associated with mortality risk. Methods: In a retrospective study, cystatin C was measured by nephelometry on plasma obtained at enrollment from 919 patients in the Fluid and Catheter Treatment Trial. Multivariable logistic regression was performed testing the association between quartiles of cystatin C and 60-day mortality. Analyses were stratified by acute kidney injury (AKI) status identified in the first 7 days after enrollment by Kidney Disease: Improving Global Outcomes (KDIGO) criteria. Results: Cystatin C was significantly higher among those patients who died compared to those who survived to 60 days [1.2 (0.9–1.9) mg/L vs. 0.8 (0.6–1.2) mg/L, p < 0.001]. Compared to the lower three quartiles, subjects in the highest quartile of cystatin C had a significantly higher odds of death at 60 days [OR 1.8 (1.2–2.6), p = 0.003 in adjusted analyses]; the odds of death incrementally rose in higher cystatin C quartiles compared to the lowest quartile (OR 1.1, 1.8, and 2.5). -

Clinical Utility of Serum Cystatin C in Predicting Coronary Artery Disease
Cardiology Journal 2010, Vol. 17, No. 4, pp. 374–380 Copyright © 2010 Via Medica ORIGINAL ARTICLE ISSN 1897–5593 Clinical utility of serum cystatin C in predicting coronary artery disease Mevlut Koc, Mustafa Kemal Batur, Osman Karaarslan, Gülcan Abali Adana Numune Education and Research Hospital, Department of Cardiology, Adana, Turkey Abstract Background: There is limited data regarding the clinical utility of cystatin C in patients with stable coronary artery disease (CAD). The aim of this study was to determine the predictive value of cystatin C for the presence and severity of CAD and the association between this protein and other biochemical risk factors for atherosclerosis in patients with suspected CAD. Methods: Ninety-four patients with CAD, and 92 patients without CAD but with cardiovascu- lar risk factors, were included in this study. Echocardiography and other pertinent laboratory examinations were performed. Subjects were divided into four groups according to their cystatin C quartile. Cystatin C groups were analyzed for the association with CAD characteristics. Results: The number of patients with CAD increased as the quartile of cystatin C increased, and there was a remarkable difference between quartiles (p < 0.001). Logistic regression analy- sis revealed independent predictors of incident CAD as cystatin C, hs-CRP, eGFR, HDL choles- terol and SBP (p = 0.005, p = 0.027, p = 0.017, p = 0.014 and p = 0.001, respectively). Moreover, cystatin C concentration was significantly correlated with CAD severity score (b = 0.258, p < 0.01). A cut-off value of 0.82 mg/L for cystatin C predicted incident CAD with a sensitivity and specificity of 75.5% and 75.0% respectively. -

Molecular Mechanisms in Amyloid Disorders. Novel Treatment Options in Hereditary Cystatin C Amyloid Angiopathy
Molecular Mechanisms in Amyloid Disorders. Novel Treatment Options in Hereditary Cystatin C Amyloid Angiopathy. Östner, Gustav 2013 Link to publication Citation for published version (APA): Östner, G. (2013). Molecular Mechanisms in Amyloid Disorders. Novel Treatment Options in Hereditary Cystatin C Amyloid Angiopathy. Division of Clinical Chemistry and Pharmacology, Faculty of Medicine, Lund University. Total number of authors: 1 General rights Unless other specific re-use rights are stated the following general rights apply: Copyright and moral rights for the publications made accessible in the public portal are retained by the authors and/or other copyright owners and it is a condition of accessing publications that users recognise and abide by the legal requirements associated with these rights. • Users may download and print one copy of any publication from the public portal for the purpose of private study or research. • You may not further distribute the material or use it for any profit-making activity or commercial gain • You may freely distribute the URL identifying the publication in the public portal Read more about Creative commons licenses: https://creativecommons.org/licenses/ Take down policy If you believe that this document breaches copyright please contact us providing details, and we will remove access to the work immediately and investigate your claim. LUND UNIVERSITY PO Box 117 221 00 Lund +46 46-222 00 00 Molecular Mechanisms in Amyloid Disorders Novel Treatment Options in Hereditary Cystatin C Amyloid Angiopathy GUSTAV RANHEIMER ÖSTNER Clinical Chemistry Department of Laboratory Medicine Lund University, Sweden DOCTORAL DISSERTATION by due permission of the Faculty of Medicine, Lund University, Sweden, to be defended at Wallenberg Neurocenter, Segerfalksalen, Sölvegatan 17, Lund, Saturday 14th of September 2013 at 9.15 a.m. -

Cystatin C, Other Markers of Kidney Disease, and Incidence of Age-Related Cataract
EPIDEMIOLOGY Cystatin C, Other Markers of Kidney Disease, and Incidence of Age-Related Cataract Barbara E. K. Klein, MD, MPH; Michael D. Knudtson, MS; Peter Brazy, MD; Kristine E. Lee, MS; Ronald Klein, MD, MPH Objective: To investigate the 15-year incidence of 3 spe- dence interval [CI], 1.09-1.41) and posterior subcapsu- cific types of age-related cataract as related to cystatin C lar (OR, 1.24; 95% CI, 1.02-1.50) cataracts. One SD and other measures of kidney function. increase in the logarithm of blood urea nitrogen and cre- atinine were associated with 15-year incidence of pos- Methods: Examinations of a population-based cohort terior subcapsular cataract (OR, 1.22; 95% CI, 1.04- (n=4926) occurred at 5-year intervals for 15 years. As- 1.42 and OR, 1.26; 95% CI, 1.03-1.54, respectively). sessment of medical history, examination, and photo- graphs of the lens after pupil dilation were performed at Conclusion: Increased levels of cystatin C are associ- each examination. Protocols for photography and grad- ated with increased risk of specific types of age-related ing were used. Laboratory measures were from speci- cataract. Whether the associations are due to the meta- mens collected at baseline. bolic changes associated with decreased renal function, common genes, or both awaits further research. Results: In multivariable analyses, a 1-SD increase in the logarithm of cystatin C was associated with 15-year in- cidence of cortical (odds ratio [OR], 1.24; 95% confi- Arch Ophthalmol. 2008;126(12):1724-1730 ATARACTS, THE MOST COM- lected in the urine and does not reappear mon cause of visual impair- in the blood. -

Serum Cystatin C-Immunoglobulin High-Molecular-Weight Complexes in Kidney and Liver Transplant Patients
Kidney International, Vol. 60 (2001), pp. 1561–1564 Serum cystatin C-immunoglobulin high-molecular-weight complexes in kidney and liver transplant patients JESU´ S HERMIDA,RAFAEL ROMERO, and J. CARLOS TUTOR Laboratorio Central y Servicio de Nefrologı´a, Hospital Clı´nico Universitario de Santiago de Compostela, Santiago de Compostela, Spain Serum cystatin C-immunoglobulin high-molecular-weight com- results obtained for renal transplant patients are still plexes in kidney and liver transplant patients. very limited [8] and even contradictory. Background. It has been suggested recently that the glomer- ular filtration rate (GFR) in renal transplant patients is under- Some authors found that serum cystatin C was a good estimated by serum cystatin C due to an impaired filtration of marker for GFR in renal transplant patients, and that it complexed cystatin C with immunoglobulins. Consequently, was clearly superior to the commonly used serum creati- serum cystatin C may not be a reliable marker of GFR in these nine [9–12]. However, others believe that cystatin C in patients. Our study was designed to determine whether this these cases would lead to a significant underestimation supposition is correct. Methods. In 87 serum samples from patients with various of the GFR [13–15] and, consequently, that it is not a kidney diseases, 182 samples from renal transplant patients, reliable marker in patients after renal transplantation and 72 samples from liver transplant patients, the concentra- [15]. Boke¨nkamp et al, after rejecting other possible tions of cystatin C and creatinine were determined, as well as causes (analytical interference of immunosuppressors, the residual concentration of cystatin C after precipitation of metabolic changes caused by immunosuppression, and macromolecules with polyethylene glycol (PEG; 6000 molecu- lar weight). -
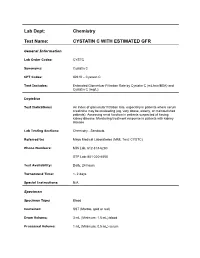
Cystatin C with Estimated Gfr
Lab Dept: Chemistry Test Name: CYSTATIN C WITH ESTIMATED GFR General Information Lab Order Codes: CYSTC Synonyms: Cystatin C CPT Codes: 82610 – Cystatin C Test Includes: Estimated Glomerluar Filtration Rate by Cystatin C (mL/min/BSA) and Cystatin C (mg/L). Logistics Test Indications: An index of glomerular filtration rate, especially in patients where serum creatinine may be misleading (eg, very obese, elderly, or malnourished patients). Assessing renal function in patients suspected of having kidney disease. Monitoring treatment response in patients with kidney disease. Lab Testing Sections: Chemistry - Sendouts Referred to: Mayo Medical Laboratories (MML Test: CYSTC) Phone Numbers: MIN Lab: 612-813-6280 STP Lab: 651-220-6550 Test Availability: Daily, 24 hours Turnaround Time: 1- 2 days Special Instructions: N/A Specimen Specimen Type: Blood Container: SST (Marble, gold or red) Draw Volume: 3 mL (Minimum: 1.5 mL) blood Processed Volume: 1 mL (Minimum: 0.5 mL) serum Collection: Routine blood collection Special Processing: Lab Staff: Centrifuge specimen, remove serum aliquot and place into a screw-capped, round bottom, plastic vial. Ship and store at refrigerated temperatures. Forward promptly. Patient Preparation: N/A Sample Rejection: Gross hemolysis; mislabeled or unlabeled specimens Interpretive Reference Range: CYSTATIN C (mg/L) Males: 0 days – 22 years No reference values established 23 – 29 years 0.60 – 1.03 mg/L 30 – 39 years 0.64 – 1.12 mg/L 40 – 49 years 0.68 – 1.22 mg/L 50 – 59 years 0.72 – 1.32 mg/L 60 – 69 years 0.77 – 1.42 mg/L 70 – 79 years 0.82 – 1.52 mg/L >79 years No reference values established Females: 0 days – 22 years No reference values established 23 – 29 years 0.57 – 0.90 mg/L 30 – 39 years 0.59 – 0.98 mg/L 40 – 49 years 0.62 – 1.07 mg/L 50 – 59 years 0.64 – 1.17 mg/L 60 – 69 years 0.66 – 1.26 mg/L 70 – 80 years 0.68 – 1.36 mg/L 81 – 86 years 0.70 – 1.45 mg/L >86 years No reference values established eGFR (all ages >18 years) >60 mL/min/BSA Note: eGFR will not be calculated for patients under 18 years. -
Natural Modulators of Amyloid Formation in Alzheimer's Disease
Natural modulators of amyloid formation in Alzheimer’s disease Sirwan M. Amin Al-Jaf A Thesis Submitted for the degree of Doctors of Philosophy July 2016 University of Sheffield Department of Molecular Biology and Technology For Sirwan’s Family; Mother, father, wife, children, brothers and sisters. Abstract Alzheimer’s disease (AD) is the most common cause of dementia, and the deposition of amyloid β (Aβ) peptide in the AD brains is a hallmark of the disease. Other amyloidogenic proteins like Transthyretin (TTR) and human Cystatin C (hCC) can modulate the aggregation of Aβ. These two proteins are proposed to play a role in the pathophysiology of AD as they are found co-deposited in amyloid deposits in the brains of AD patients, most notably at the cell surface. Animal models and cell line assays showed protective roles for TTR and hCC against Aβ-induced toxicity, and Aβ fibril formation is inhibited through interaction with TTR and hCC. This study investigated the mechanism of in vitro interaction of TTR with Aβ. The ability of WT TTR to inhibit Aβ fibrillisation in the presence of Aβ binding surfaces was higher than in the presence of non-binding surfaces. Then, the interaction between different TTR mutants with different multimeric stabilities and different alloforms of Aβ showed that TTRs with less stable tetramers and unfolded monomers are the best inhibitors of Aβ fibrillisation. Analysing the thioflavin T curves of Aβ aggregation in the presence of TTRs and the interaction of TTRs with different forms of Aβ showed that the interaction between the two proteins occurs mainly through binding to early nucleating species of Aβ rather than to the monomer. -

Cytotoxic Properties of Amyloidogenic L68Q Cystatin C
Cytotoxic properties of amyloidogenic L68Q cystatin C A search for therapeutic agents Indíana Elín Ingólfsdóttir Thesis for the degree of Master of Science University of Iceland Faculty of Medicine School of Health Sciences Eitrunareiginleikar mýlildismyndandi L68Q Cystatin C - Leit að verndandi þáttum - Indíana Elín Ingólfsdóttir Ritgerð til meistaragráðu í Líf- og læknavísindum Leiðbeinandi: Finnbogi Rútur Þormóðsson Umsjónarkennari: Elías Ólafsson Meistaranámsnefnd: Bjarni Ásgeirsson Læknadeild Heilbrigðisvísindasvið Háskóla Íslands Maí 2013 Cytotoxic properties of amyloidogenic L68Q cystatin C A search for therapeutic agents Indíana Elín Ingólfsdóttir Thesis for the degree of Master of Science Supervisor: Finnbogi Rútur Þormóðsson Masters committee: Elías Ólafsson and Bjarni Ásgeirsson Faculty of Medicine School of Health Sciences May 2013 Ritgerð þessi er til meistaragráðu í líf- og læknavísindum og er óheimilt að afrita ritgerðina á nokkurn hátt nema með leyfi rétthafa. © Indíana Elín Ingólfsdóttir, 2013 Prentun: Prentsmiðja, Samskipti Reykjavík, Ísland, 2013 Ágrip Mýlildis sjúkdómar einkennast af villu í umbroti á utanfrumu próteinum sem veldur uppsöfnun þeirra og útfellingu í torleysanlega þræði. Eftir því sem meira safnast upp af þessu torleysanlega efni verður vaxandi starfstruflun í þeim vefjum þar sem mýlildið (amyloid) safnast fyrir. Hér er fjallað um tvo mýlildissjúkdóma; arfgeng heilablæðingu (HCHWA-I) og Alzheimers sjúkdóminn (AD). Arfgeng heilablæðing, sem erfist ríkjandi og ókynbundið, einskorðast við Ísland. Það er punktstökkbreyting í stöðu 68 í cystatin C próteininu sem veldur því að glútamín amínósýra kemur í staðinn fyrir leusín. Þetta veldur uppsöfnun próteinsins og útfellingum innan veggja heilaslagæða sjúklinga. Þessi uppsöfnun veikir æðaveggina sem veldur blæðingu og heilablóðfalli langt fyrir aldur fram. Alzheimer´s sjúkdómur er heilahrörnunar sjúkdómur sem veldur vitglöpum fyrir aldur fram.