In Southwest Nigeria: Realities and People's Perceptions and Perspectives
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Comparative Analysis of Personnel Distributions in the Local Government Service in Ekiti-State, Nigeria, for Service Delivery Olaniyan Joseph Olawale A, Ademuyiwa A
I.J. Mathematical Sciences and Computing, 2019, 2, 44-53 Published Online April 2019 in MECS (http://www.mecs-press.net) DOI: 10.5815/ijmsc.2019.02.04 Available online at http://www.mecs-press.net/ijmsc Comparative Analysis of Personnel Distributions in the Local Government Service in Ekiti-State, Nigeria, for Service Delivery Olaniyan Joseph Olawale a, Ademuyiwa A. Justus b a Department of Mathematics and Statistics, Federal Polytechnic Ado-Ekiti, Ado-Ekiti, 360231, Nigeria b Department of Statistics, Federal Polytechnic Ile-Oluji, Ile-Oluji, 3751110, Nigeria Received: 15 March 2017; Accepted: 13 February 2019; Published: 08 April 2019 Abstract It’s is no longer news that the Local Government (Third-tier of government in Nigeria) has not been able to optimally discharge its responsibilities according to its mandate. This had raised serious policy and research concerns that resulted to several reformative approaches in a bid to restructuring the system for efficient service delivery in the past decade. One major unpopular reason for inefficient service delivery was poor administration in the Local Government as a result of unbalanced distribution of personnel by cadre and gender in each local government in the state. This had not only hampered local government administration but also impeded adequate provision of expected services to local populace in line with its mandate as enshrined in the fourth schedule of the 1999 Constitution of the Federal Republic of Nigeria. Application of Statistical analysis using Chi-square Test of Independence showed that distribution of employees by cadre depends on local government in post in the year under study. -

INFORMATION KIT on EKITI STATE GOVERNORSHIP ELECTION Map
_________ INEC Info Kit for Ekiti Governorship Election (June 21, 2014) ________ INFORMATION KIT ON EKITI STATE GOVERNORSHIP ELECTION Map of Ekiti State Brief on Ekiti State Ekiti State is in the Southwest geo-political zone of Nigeria, with Ado- Ekiti as the state capital. The state was created on October 1, 1996 from the old Ondo State. It comprises 16 local government areas, namely: Ado-Ekiti, Efon, Ekiti East, Ekiti South-West, Ekiti West, Emure, Gbonyin, Ido-Osi, Ijero and Ikere. Others are Ikole, Ilejemeje, Irepodun/Ifelodun, Ise/Orun, Moba and Oye. 1 _________ INEC Info Kit for Ekiti Governorship Election (June 21, 2014) ________ The state shares boundaries with Kwara State to the north, Osun State to the west, Kogi State to the east and Ondo State to the south. Ekiti State has a land area of 6, 353 sq. km. The State is mainly an upland zone, rising over 250 meters above sea level. Besides the state capital, Ado-Ekiti, major towns in the state include Efon Alaye, Ijero, Otun, Iye, Ido, Oye, Ikole, Ode, Emure, Ikere and Ilawe. State Electoral Statistics The Independent National Electoral Commission (INEC) has fixed the Ekiti State Governorship Election for Saturday, June 21, 2014, and everything has been put in place by the Commission to make the election free, fair and credible. Relevant statistics pertaining to Ekiti State and the election are as follows: Ø No. of Local Government Areas – 16 Ø Senatorial Districts: (i) Ekiti North, (ii) Ekiti Central, (iii) Ekiti South Ø Federal Constituencies: (i) Ekiti North I, (ii) Ekiti North II, (iii) Ekiti Central I, (iv) Ekiti Central II, (v) Ekiti South I, (vi) Ekiti South II Ø No. -

Factors Influencing the Acceptance of Routine Immunization Among Ebira People in Selected Areas of Ado Ekiti, Ekiti State, Nigeria
IOSR Journal of Nursing and Health Science (IOSR-JNHS) e-ISSN: 2320–1959.p- ISSN: 2320–1940 Volume 9, Issue 3 Ser. VI (May - June 2020), PP 09-16 www.iosrjournals.org Factors Influencing The Acceptance Of Routine Immunization Among Ebira People In Selected Areas Of Ado Ekiti, Ekiti State, Nigeria. Olakanmi-Falade Bukola Abiodun1 (RN, RM, RPHN), AJAO Ezekiel Olasunkanmi2 (RN, PhD, FWACN), MAITANMI Julius Olatade3 (RN, MSc). 1(Department of Nursing, Ekiti State University Teaching Hospital) 2(Department of Community/Public health Nursing, School of Nursing, Babcock University) 3(Department of Community/Public health Nursing, School of Nursing, Babcock University) Abstract: Background: Despite government actions and policy to scale up routine immunization in Nigeria, the uptake in Nigeria and many Africa nations remains low when compared with more advanced countries. This study aimed at examining factors influencing acceptability of routine immunization among married Ebira women in selected communities of Ekiti State. Material and Methods: The study is a descriptive research and it employed cross-sectional design. Data was gathered from 361 women who had a minimum of two year-old children as at the time of survey, from selected communities in Ado Local Government such as Erinfun, Ukewo and Ago corner. Ethical approval was sought for from Research and Ethic Committee, Babcock University, Ilishan-Remo Ogun State. In addition, respondents were consented for full participation. Result: The study found that majority (96%) of the respondents utilized routine immunization for their children. It was also revealed that a substantial number (97%) of husbands accepted the immunization to be administered to their children. -

Consolidated Accounts of the Local Governments of Ekiti State, Nigeria
EKITI STATE OF NIGERIA REPORT OF THE AUDITOR-GENERAL FOR LOCAL GOVERNMENTS ON THE CONSOLIDATED ACCOUNTS OF THE LOCAL GOVERNMENTS OF EKITI STATE, NIGERIA FOR THE YEAR ENDED 31ST DECEMBER, 2018 1 YEAR 2018 GENERAL PURPOSE FINANCIAL STATEMENTS TABLE OF CONTENTS PAGES 1. Table of contents ………………………………………………………………….. 2 2. Audit Certificate:……………………………………………………………………. 3 3. Report of Auditor-General for the year 2018 …………………………… 4-19 4. Consolidated General Purpose Financial Statement for the year 2018 20-61 Fiscal operation report (FOR) for the year ………………………………… 62-66 5. Date of submission of General Purpose Financial Statement by Local Governments 67 6. Position of Accounts ……………………………………………………………… 68 7. Final Budget for the 16 Local Governments ……………………………. 69 8. Position of Current Audit Queries …………………………………………… 70-81 9. General Purpose Financial Statement of individual Local Governments i. Ado Local Government ………………………………… 82-96 ii. Efon “ ………………………………… 97-117 iii Emure “ …………………………………. 118-126 iv Ekiti East “ ……………………………… 127-137 v. Ekiti South West “ ………………………………… 138-150 vi. Ekiti West “ ……………………………….. 151-167 vii Gbonyin “ ………………………………… 168-180 viii Ido/Osi “ ……………………………….. 181-196 ix Ijero “ ……………………………….. 197-205 x. Ikere “ ……………………………….. 206-220 xi Ikole “ ……………………………….. 221-229 xii Ilejemeje “ ……………………………….. 230-240 xiii Irepodun/Ifelodun “ ………………………………… 241-254 xiv Ise/Orun “ ……………………………….. 255-270 xv Moba “ ………………………………… 271-284 xvi Oye “ ……………………………….. 285-294 2 AUDIT CERTIFICATE I have examined the General Purpose Financial Statements of all the Sixteen Local Governments of Ekiti State as at 31st December, 2018 in accordance with Sections 123(2) of the Constitution of the Federal Republic of Nigeria 1989; 316(1) of the Constitution of the Federal Republic of Nigeria 1999, 32 (2) of the Local Government Administration Law No 2 of 1999, and section 26(26) of Ekiti State Audit Law 2014. -
States and Lcdas Codes.Cdr
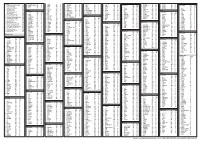
PFA CODES 28 UKANEFUN KPK AK 6 CHIBOK CBK BO 8 ETSAKO-EAST AGD ED 20 ONUIMO KWE IM 32 RIMIN-GADO RMG KN KWARA 9 IJEBU-NORTH JGB OG 30 OYO-EAST YYY OY YOBE 1 Stanbic IBTC Pension Managers Limited 0021 29 URU OFFONG ORUKO UFG AK 7 DAMBOA DAM BO 9 ETSAKO-WEST AUC ED 21 ORLU RLU IM 33 ROGO RGG KN S/N LGA NAME LGA STATE 10 IJEBU-NORTH-EAST JNE OG 31 SAKI-EAST GMD OY S/N LGA NAME LGA STATE 2 Premium Pension Limited 0022 30 URUAN DUU AK 8 DIKWA DKW BO 10 IGUEBEN GUE ED 22 ORSU AWT IM 34 SHANONO SNN KN CODE CODE 11 IJEBU-ODE JBD OG 32 SAKI-WEST SHK OY CODE CODE 3 Leadway Pensure PFA Limited 0023 31 UYO UYY AK 9 GUBIO GUB BO 11 IKPOBA-OKHA DGE ED 23 ORU-EAST MMA IM 35 SUMAILA SML KN 1 ASA AFN KW 12 IKENNE KNN OG 33 SURULERE RSD OY 1 BADE GSH YB 4 Sigma Pensions Limited 0024 10 GUZAMALA GZM BO 12 OREDO BEN ED 24 ORU-WEST NGB IM 36 TAKAI TAK KN 2 BARUTEN KSB KW 13 IMEKO-AFON MEK OG 2 BOSARI DPH YB 5 Pensions Alliance Limited 0025 ANAMBRA 11 GWOZA GZA BO 13 ORHIONMWON ABD ED 25 OWERRI-MUNICIPAL WER IM 37 TARAUNI TRN KN 3 EDU LAF KW 14 IPOKIA PKA OG PLATEAU 3 DAMATURU DTR YB 6 ARM Pension Managers Limited 0026 S/N LGA NAME LGA STATE 12 HAWUL HWL BO 14 OVIA-NORTH-EAST AKA ED 26 26 OWERRI-NORTH RRT IM 38 TOFA TEA KN 4 EKITI ARP KW 15 OBAFEMI OWODE WDE OG S/N LGA NAME LGA STATE 4 FIKA FKA YB 7 Trustfund Pensions Plc 0028 CODE CODE 13 JERE JRE BO 15 OVIA-SOUTH-WEST GBZ ED 27 27 OWERRI-WEST UMG IM 39 TSANYAWA TYW KN 5 IFELODUN SHA KW 16 ODEDAH DED OG CODE CODE 5 FUNE FUN YB 8 First Guarantee Pension Limited 0029 1 AGUATA AGU AN 14 KAGA KGG BO 16 OWAN-EAST -

Estimation of Potential Load Demand of Local Government Areas of Ekiti State, Nigeria
American Journal of Engineering Research (AJER) 2014 American Journal of Engineering Research (AJER) e-ISSN : 2320-0847 p-ISSN : 2320-0936 Volume-03, Issue-06, pp-101-106 www.ajer.org Research Paper Open Access Estimation of Potential Load Demand of Local Government Areas of Ekiti State, Nigeria Oluwatosin Samuel, Adeoye Oluwatosin Samuel Adeoye is with Electrical and Electronic Engineering Department, Federal University of Technology,Akure, Nigeria. Abstract: - The estimation of the potential load demand of local government areas in Ekiti State, Nigeria, was carried out using per capita demand estimate of a fully electrified urban area and population data. The pessimistic load demands of the local government areas were calculated through the use of per capita of a rural community in Ekiti state. This was achieved through the injected powers and the State’s zonal population. The study demonstrated that there is wide difference between the projected load demands and the actual supply; thus impairing rural electrification of the State. Keywords: - injected power, load centers, load demand, power balance. I. INTRODUCTION Efficient power management is prerequisite in maintaining consumer confidence. One form of maintaining or at least controlling power is by injecting sizeable power into the zone substation. Often this form of power augmentation is needed for relatively short period where substations supply large load components. A small quantity of about 3 to 4 MW was released by the Akure injection substation at night periods, when the entire state depended on 132/33kV injection substation at Akure.[1] The zone substation has been supplied from a long transmission from Oshogho axis. -

Bayowa Et Al
Ife Journal of Science vol. 16, no. 3 (2014) 353 INTEGRATION OF HYDROGEOPHYSICAL AND REMOTE SENSING DATA IN THE ASSESSMENT OF GROUNDWATER POTENTIAL OF THE BASEMENT COMPLEX TERRAIN OF EKITI STATE, SOUTHWESTERN NIGERIA. 1Bayowa O.G., 2Olorunfemi M.O., 3Akinluyi F.O., and 4Ademilua O.L 1Department of Earth Sciences, Ladoke Akintola University of Technology, Ogbomoso, Nigeria. 2Department of Geology, Obafemi Awolowo University, Ile-Ife, Nigeria. 3Department of Remote Sensing and GIS, Federal University of Technology, Akure, Nigeria. 4Department of Geology, Ekiti State University, Ado-Ekiti, Nigeria. Corresponding Author E-mail:[email protected]; [email protected] (Received: 8th August, 2014; Accepted: 12th August, 2014) ABSTRACT Hydrogeophysical investigation as well as analyses of hydrogeomorphological, geologic/hydrogeologic, electrical resistivity and borehole data had been carried out in the Basement Complex terrain of Ekiti State, Southwestern Nigeria. This was with a view to classifying the area into different groundwater potential zones. The VES interpretation results were used for aquifer identification; aquifer geoelectric parameter determination and for the calculation of the overburden coefficient of anisotropy. Hydrogeomorphological, lineament density, lineament intersection density and overburden coefficient of anisotropy thematic maps were produced and integrated for the classification of the study area into different groundwater potential zones. The reliability of the groundwater potential map was checked with the existing groundwater yield data. The weathered and fractured basement constituted the main aquifer units. The groundwater yields of boreholes located within quartzitic rocks had a mean of 1.56 l/s while the mean groundwater yield from metasediment (schist) was 1.14 l/s. The study area was characterized into five different groundwater potential zones which were very low, low, moderate, high and very high. -

Spatial Distribution of Infrastructural Facilities in Ekiti State
IOSR Journal Of Humanities And Social Science (IOSR-JHSS) Volume 25, Issue 1, Series. 2 (January. 2020) 01-12 e-ISSN: 2279-0837, p-ISSN: 2279-0845. www.iosrjournals.org Spatial Distribution of Infrastructural Facilities in Ekiti State. Fashoto Busayo*. Adeniyi Peter Department of Geography, University of Lagos Corresponding Author: Fashoto Busayo ABSTRACT: One of the major problems inhibiting the development process in Nigeria is the inadequate provision of infrastructural facilities which is further compounded by the lack of reliable information of their number and spatial distribution. Hence this paper was aimed toassess the spatial pattern and distribution of existing infrastructure in Ekiti state.An inventory of the existing infrastructure such education, administration, commercial, public utility, transportation, health, recreation and communication.Mean deviation, location quotient and nearest neighbour analysis to evaluate the distribution of these facilities.The result of the analysis shows that disparity exists among the LGAs.It was observed that LGAs like Efon, Ikere, Irepodun and Moba are lagging in education infrastructure, while other LGAs has these facilities more than expected.Virtually all the LGAs has public utility but Ikere LGA is less privileged while commercial facility such as bank is less expected in all the LGAs expect Ado LGA. This paper concludes by suggesting that future researches should examine in more detail the role of rural infrastructure on social development of rural areas by laying emphasis on the quality of the infrastructure rather than quantity, so as to figure out the true dimension of the development. KEYWORDS: Infrastructural Facility,under-served areas,GIS ----------------------------------------------------------------------------------------------------------------------------- ---------- Date of Submission: 27-12-2019 Date of Acceptance: 10-01-2020 ----------------------------------------------------------------------------------------------------------------------------- ---------- I. -

221 SHORT COMMUNICATION Occurrence of Diarrhoea Among Infants and Children in Ekiti State, Nigeria: a Retrospective Study
Malaysian Journal of Microbiology, Vol 6(2) 2010, pp. 221-224 SHORT COMMUNICATION Occurrence of diarrhoea among infants and children in Ekiti State, Nigeria: A retrospective study David, O. M. 1, Oluyege, A. O. 1 and Famurewa, O. 1,2 * 1Department of Microbiology, University of Ado-Ekiti, Nigeria. 2College of Science, Engineering and Technology, Osun State University, Osogbo, Nigeria. E-mail: [email protected] Received 9 December 2010; received in revised form 10 February 2010; accepted 24 February 2010 _______________________________________________________________________________________________ ABSTRACT A six-year retrospective study of the prevalence of diarrhoea among infants and children in 64 health care facilities including 48 basic health centers and 16 comprehensive health centers in Ekiti State, Nigeria was carried out as a preliminary determination of the rate of diarrhoea among children. Data in the medical records in the healthcare facilities between the years 2002–2007 were extracted to determine the rate of diarrhoea in the state. Prospective study is recommended for Local Government with the highest prevalence rate of infantile diarrhoea. Ikere Local Government Area recorded the highest prevalent with 265 cases made up of 131 male and 134 female followed by Gboyin Local Government Area with 130 and 118 cases in male and female, respectively. Ilejemeje and Moba Local Government Areas had the least cases of dysentery, within the period of the study, with 75 and 95, respectively. The highest cases of diarrhea were recorded in 2006; 380 male and 358 female, followed by 2007 with 588 cases. Year 2002 had the least number of cases of diarrhea, with 110 and 81 in males and females respectively. -

Nigeria Security Situation
Nigeria Security situation Country of Origin Information Report June 2021 More information on the European Union is available on the Internet (http://europa.eu) PDF ISBN978-92-9465-082-5 doi: 10.2847/433197 BZ-08-21-089-EN-N © European Asylum Support Office, 2021 Reproduction is authorised provided the source is acknowledged. For any use or reproduction of photos or other material that is not under the EASO copyright, permission must be sought directly from the copyright holders. Cover photo@ EU Civil Protection and Humanitarian Aid - Left with nothing: Boko Haram's displaced @ EU/ECHO/Isabel Coello (CC BY-NC-ND 2.0), 16 June 2015 ‘Families staying in the back of this church in Yola are from Michika, Madagali and Gwosa, some of the areas worst hit by Boko Haram attacks in Adamawa and Borno states. Living conditions for them are extremely harsh. They have received the most basic emergency assistance, provided by our partner International Rescue Committee (IRC) with EU funds. “We got mattresses, blankets, kitchen pots, tarpaulins…” they said.’ Country of origin information report | Nigeria: Security situation Acknowledgements EASO would like to acknowledge Stephanie Huber, Founder and Director of the Asylum Research Centre (ARC) as the co-drafter of this report. The following departments and organisations have reviewed the report together with EASO: The Netherlands, Ministry of Justice and Security, Office for Country Information and Language Analysis Austria, Federal Office for Immigration and Asylum, Country of Origin Information Department (B/III), Africa Desk Austrian Centre for Country of Origin and Asylum Research and Documentation (ACCORD) It must be noted that the drafting and review carried out by the mentioned departments, experts or organisations contributes to the overall quality of the report, but does not necessarily imply their formal endorsement of the final report, which is the full responsibility of EASO. -

A Module on Market Condition and Regional Development Planning in Ekiti-State, South Western Nigeria
Research on Humanities and Social Sciences www.iiste.org ISSN (Paper)2224-5766 ISSN (Online)2225-0484 (Online) Vol.6, No.17, 2016 A Module on Market Condition and Regional Development Planning in Ekiti-State, South Western Nigeria Okosun, Senator .Endurance 1 Ehisuoria, Solomon E 2 Olamiju, Oluwadara, I 1 Akande, Deborah Omoyemi, C 3 Dairo, Omolola E 4 Adeyemi, Alarape Ola-Omole, Motunrayo 1 Ige, Victor Ayobami 1 1. Department of Urban and Regional Planning School of Environmental Technology. Federal University of Technology Akure, Nigeria 2. Department of Geography and Regional Planning, School of Social Sciences, Ambrose Alli University, Ekpoma, Nigeria 3. Department of Urban and Regional Planning, School of Environmental Studies. Auchi Polytechnic, Auchi, Nigeria 4. Department of Estate Management, School of Environmental Studies. Crown Polytechnic, Ado Ekiti, Nigeria Abstract A market place is a geographical space that facilitates trade and enables the distribution and allocation of resources in a society, whereby parties engage in exchange of goods and services which promotes production, promotion, distribution, and consumption activities and improve the welfare and social life of the people. The purpose of the study was is to assess the types and conditions of the markets facilities in Ikere, Ise/Orun and Emure region of Ekiti state, Nigeria with a view to enhancing the economic development of the study area. This study adopted the survey research method, and used three different questionnaires to collect research data from the authority in Ikere, Ise/Orun and Emure Local Government Councils of Ekiti State, Market authorities in Ikere, Ise/Orun and Emure LG Councils of Ekiti State and the market traders in the study area which is the main focus of this study. -

The Effectiveness of Insecticide Treated Net (Itn) in the Control of Malaria
J. Basic. Appl. Sci. Res., 2(1)908-911, 2012 ISSN 2090-4304 Journal of Basic and Applied © 2012, TextRoad Publication Scientific Research www.textroad.com THE EFFECTIVENESS OF INSECTICIDE TREATED NET (ITN) IN THE CONTROL OF MALARIA. Adewole, S.O. Department of Zoology, Ekiti State University, p.m.b. 5363, Ado-Ekiti, Ekiti State, Nigeria. ABSTRACT Studies on the effectiveness of the use of Insecticide Treated Net (ITN) in the control of malaria was carried out in hospitals in Ekiti State. A total of 2,000 questionnaire were administered and 1,977 copies of these questionnaire were returned by the respondents. Of the 1,977 questionnaire collected, 176 respondents representing 8.9% confirmed the effectiveness of ITN in the control of malaria. Female has the highest prevalence of malaria with 71.9% while the male has the least prevalence of malaria with 28.1%. There was a significant difference (t = 2.17; P<0.05) in the percentage prevalence of malaria between males and females. However, there was no significant difference (t = 1.07; P>0.05) between frequency of use of ITN in once and twice a year among the patients. Of the sixteen Local Government Areas sampled, Ado-Ekiti Local Government Area has the highest percentage 22(17.6%) distribution of ITN while Ise and Ilejemeje Local Government Areas have the least percentage 5(4%) distribution of ITN. Low use of ITN was widely reported by the respondents. KEY WORDS: Insecticide Treated Net (ITN), Hospital(s), patients, malaria and questionnaire. INTRODUCTION Malaria is a wide spread disease and it is of important public health concern in Nigeria because of its impact on children and maternal health (Orimadegun, et al, 2007).