Pneumococcal Vaccine Coverage Among Children Less Than 2 Years of Age: Preliminary Findings of a Vaccine Coverage Survey in Lowe
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Organizational Presence in Union Councils of Sindh - ER - Floods 2011
Organizational presence in Union Councils of Sindh - ER - Floods 2011 Gilgit Baltistan China ! ! ! ! ! ! ! ! ! !! ! ! !! Khyber Pakhtun! khwa !! ! ! Azad Kashmi!r! Disputed Territory Afghanistan Fata ! 4 Punjab Tangwani Kashmore Thul Balochistan Kashmore India Jacobabad Jacobabad Iran Ubauro Kanhdkot Sindh Shikarpur Garhi Khairo Khanpur (Shikarpur) Ghotki Arabian sea Shahdadkot Shikarpur Qubo Saeed Khan Lakhi Daharki Garhi Yasin Pano Aqil Miro Khan Ghotki Ratodero Sukkur Mirpur Mathelo Kingri Qambar Shahdadkot Rohri Kambar Ali Khan Larkana Khairpur Khangarh Larkana Gambat Warah Bakrani Sukkur Kot Diji Salehpat Dokri Sobodhero Mehar Khairpur Nathan Shah Kandiaro Mirwah Ghulam Shah Bagrani Saeedpur Bhiria Naushahro Feroze Dadu Dadu Naushahro Feroze Faiz Ganj Khairpur Moro Nara Johi Kazi Ahmed Daur Shaheed Benazirabad Nawabshah Sehwan Sinjhoro Barhoon Sakrand Shahdadpur Sanghar Ashgarabad Sinjhoro Sindh Jaffar Khan Laghari Kurkali Jhatia Jhol Khipro Hala Manik ThaheemSyes Sughatullah Shaheed Manjhand Khori Tando Adam Sanghar Hatungo Matiari Jan Nawaz Ali Jamshoro Jhando Mari Matiari Dassori Khahi Mirabad Mirpur Khas Pithoro Thano Bula Khan Kotri Shadi pali Pithoro Saabho Qasimabad Tando Allah Yar Tando Allah Yar Umerkot Hyderabad City Hyderabad Sanjar Chang Dengan Dad Jarwar Samaro Umerkot Hyderabad Kot Ghulam Muhammad Latifabad MMirir pImuamr B uKx Hhadai Bsux Burgury padhario Tando Muhammad Khan Saeed Khan Lund Digri Chachro Matli Sufan Shah Kunri Mulakatyar Mir Khuda Buksh Saeed Matto Lakhat Tando Jan Mohammad Karachi City Thatta Malir -

Sindh Province - Flood Analysis (Flood Extent from 27 August 2010 to 07 September 2010)
Pakistan Floods: Sindh Province - Flood Analysis (Flood Extent from 27 August 2010 to 07 September 2010) Kashmore Taluka Thul Taluka Kashmore PUNJAB Jacobabad Taluka Kandhkot Taluka BALOCHISTAN Jaccobabad Ubauro Taluka Shikarpur Taluka Garhi Khairo Taluka Khanpur Taluka Ghotki Taluka Shikarpur Lakhi Taluka Garhi Yasin Taluka Shahdad Kot Taluka Pano Aqil Taluka Ghotki Daharki Taluka Miro Khan Taluka Sukkur Taluka Ratodero Taluka Kambar Ali Khan Taluka Mirpur Mathelo Taluka Kingri Taluka Rohri Taluka Qambar Shahdad kot Larkana Taluka Khairpur Taluka Khangarh Taluka Larkana Gambat Taluka Hamal Lake Warah Taluka Sukkur Dokri Taluka Kot Diji Taluka Salehpat Taluka Sobho Dero Taluka Mehar Taluka An estimated 7 million people are affected Khairpur Nathan Shah Taluka Kandiaro Taluka Mirwah Taluka 19 districts and 7,277 villages are affected. 1,098,720 houses are damaged Bhiria Taluka 199 deaths and 1,072 injuries are reported Naushahro Feroze (Source: NDMA, PDMA, GBDMA, FDMA as of 13092010) Dadu Khairpur Faiz Ganj Taluka Naushahro Feroze Taluka Dadu Taluka Moro Taluka Nara Taluka Johi Taluka Manchar Lake Daulat Pur Taluka Nawabshah Taluka Flood Water entered Jhanagar ! ! S.Banazirabad and Bajara towns as Manchar lake brusted as of 13 Sep 2010 Sehwan Taluka SINDH (UNOCHA Sit Rep # 24) Sakrand Taluka Shahdadpur Taluka Sanghar Taluka Water Supplies to Shewan tehsil I N D I A was cut down due to possible Sinjhoro Taluka contamination as of 13 Sep 2010 Sanghar Hala Taluka (UNOCHA Sit Rep # 24). Khipro Taluka Tando Adam Taluka Matiari Jam Nawaz -

Government of Sindh Finance Department
2021-22 Finance Department Government of Sindh 1 SC12102(102) GOVERNOR'S SECRETARIAT/ HOUSE Rs Charged: ______________ Voted: 51,652,000 ______________ Total: 51,652,000 ______________ ____________________________________________________________________________________________ GOVERNOR'S SECRETARIAT ____________________________________________________________________________________________ BUILDINGS ____________________________________________________________________________________________ P./ADP DDO Functional-Cum-Object Classification & Budget NO. NO. Particular Of Scheme Estimates 2021 - 2022 ____________________________________________________________________________________________ Rs 01 GENERAL PUBLIC SERVICE 011 EXECUTIVE & LEGISLATIVE ORGANS, FINANCAL 0111 EXECUTIVE AND LEGISLATIVE ORGANS 011103 PROVINCIAL EXECUTIVE KQ5003 SECRETARY (GOVERNOR'S SECRETARIAT/ HOUSE) ADP No : 0733 KQ21221562 Constt. of Multi-storeyed Flats Phase-II at Sindh Governor's 51,652,000 House, Karachi (48 Nos.) including MT-s A12470 Others 51,652,000 _____________________________________________________________________________ Total Sub Sector BUILDINGS 51,652,000 _____________________________________________________________________________ TOTAL SECTOR GOVERNOR'S SECRETARIAT 51,652,000 _____________________________________________________________________________ 2 SC12104(104) SERVICES GENERAL ADMIN & COORDINATION Rs Charged: ______________ Voted: 1,432,976,000 ______________ Total: 1,432,976,000 ______________ _____________________________________________________________________________ -

Notice Inviting Tender
Office of the Executive Engineer, Education Works Division, Sujawal School Education Department, Government of Sindh No.TC/G-55/EWDS/ at,I dated /0 .04.2017 NOTICE INVITING TENDER Sealed Bids for the works mentioned below are invited from the interested Bidders / Firms on Standard Bidding Documents of SPPRA under Sindh Public Procurement Regulatory Authority. Rules 2010 (amended to date) :- 2. bidding documents will be issued to all the interested Bidders on written request to the undersigned ton tirm's original letterhead and payment of bidding documents fee in cash as shown against each (non refundable). Programme for issuance / submission and openingof Bids In case of un-responded works S' Particulars I" Attempt No. rd Attempt _ of bidding From the date of publication in A Date of issuance From tk ' B ' 2017 and press and hoisting on website of documents at or before 2.00pm on SPPRA at or before 2.00pm on A.DU • 2017 IA %..• 2017 B Dead line for submission of bids ?x......6.....2017 up to 3.00pm N 4.1.1.5..2017 up to 2.00pm in in the office of the undersigned the office of the undersigned C Venue, time and date of bids ''6.— 6. —...2017 at 4.00pm in 1. .a S.A....2017 at 3.00pm in opening the office of the undersigned the office of the undersigned 3. Bidding is open to all interested bidders. 4. Method of procurement i.e Single Stage — Single Envelope. 5. Bid Validity Period is (90) Ninety days. of Works Estimated Bidding Bid Completion Document S. -

(RNA) Monsoon Rains
Rapid Need Assessment Report (RNA) Monsoon Rains Thatta, Sujawal and Hyderabad th th 24 – 27 August 2020 Thatta Sujjawal Hyderabad Prepared by: Health And Nutrition Development Society (HANDS) Address: Plot #158, Off M9 (Karachi – Hyderabad) Motorway, Gadap Road, Karachi, Pakistan, Ph: (0092-21) 32120400-9 , +92-3461117771 Web: www.hands.org.pk Email: [email protected] Table of Contents 1. Introduction ......................................................................................................................................... 3 1.1. Background ................................................................................................................................. 3 1.2. Objectives .................................................................................................................................... 4 1.3. Methodology ................................................................................................................................ 4 1.4. Limitations ................................................................................................................................... 4 1.5. Summary of Findings ................................................................................................................. 4 1.6. Sectoral Need Priority Ranking................................................................................................. 6 2. Key Findings District Thatta .............................................................................................................. -

Provincial Assembly of Sindh 4Th Assembly (12Th
PROVINCIAL ASSEMBLY OF SINDH 4TH ASSEMBLY (12TH SEPTEMBER 1953 TO 26TH MARCH 1955 S.NO. NAME CONSTITUENCY 01. Honourable Mir Ghulam Ali Khan Mir Haji Bandeh Ali Guni North Khan Talpur took oath on 11th September,1953 before His Excellency the Governor, at Governor House. 02. Mr. Abdullah Haji Mohammad Ismail Mahesar Kakar Mehar Joint 03. Mr. Abdul Fatah Wali Mohammad Memon Warah West 04. Mr. Abdul Hamid Kadiir Bakhsh Jatoi Kakar 05. Mr.Abdul Majid khan Karim Bakhsh Khan Jatoi Mehar 06. Honourable, Abdul Manan Abdul Rahman Kazi Miro Khan 07. Abdul Khair alias Bashir Ahmed Khan Fateh Ubauro Mohammad Khan, Jam 08. Mir. Ahmed Khan Haji Abdullah Khan Talpur Nagarparkar 09. Mr. Ahmed Khan Fateh Khan Rajpar Naushahro Feroze (South) 10. Mr. Ahmed Khan Rasul Bakhsh Bhutto Ratodero 11. Mir. Ahmed Khan Shah Passand Khan Shikarpur(Central) 12. Mr. Aidansing Nagji Sodho Tharparkar-Nagarparkar 13. Begum Aishah Mohammad Abdul Aziz Arain Muslim Women Central 14. Mr. Ali Asghar Shah Chandmir Shah Shirazi Mirpur Sakro 15. Mir Haji Ali Ahmed Khan Mir Haji Nabi Bakhsh Khan Hyderabad Taluka South Talpur 16. Mr. Ali Bilawal Khan Shah Ali Khan Domki Kashmore 17. Mr. Ali Gohar Khan Haji Mahar Rohri West 18. Mr. Ali Gohar Khan Mohammad Khuhro Larkana East 19. Mr. Ali Hassan Mohammad Ibrahim Mangi New Sukkur North 20. Honorurable Pir Ali Mohammad Rashdi Rohri West 21. Mr. Ali Nawaz Khan Ali Murad Khan Dharejo Pano Akil 22. Honourable Mir Ali Nawaz Khan Talpur Guni (South) 23. Pir Ali Shah Bhawan Ali Shah Jillani Badin North 24. Mir. Allah Bachayo Khan Haji Fateh Khan Talpur Digri 25. -
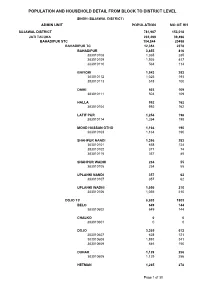
Sujawal Blockwise
POPULATION AND HOUSEHOLD DETAIL FROM BLOCK TO DISTRICT LEVEL SINDH (SUJAWAL DISTRICT) ADMIN UNIT POPULATION NO OF HH SUJAWAL DISTRICT 781,967 153,018 JATI TALUKA 202,299 39,496 BAHADIPUR STC 104,844 20458 BAHADIPUR TC 12,354 2378 BAHADIPUR 3,855 816 383010108 1,365 285 383010109 1,926 417 383010110 564 114 BHIYORI 1,543 293 383010112 1,025 193 383010113 518 100 DAIKI 503 109 383010111 503 109 HALLA 992 162 383010104 992 162 LATIF PUR 1,254 198 383010114 1,254 198 MOHD HASSAN OTHO 1,164 190 383010103 1,164 190 SHAHPUR NANDI 1,396 283 383010101 658 124 383010102 371 74 383010115 367 85 SHAHPUR WADHI 234 55 383010105 234 55 UPLANKI NANDI 357 62 383010107 357 62 UPLANKI WADHI 1,056 210 383010106 1,056 210 DOJO TC 8,803 1803 BELO 649 144 383010602 649 144 CHALKO 0 0 383010601 0 0 DOJO 3,365 612 383010607 628 121 383010608 1,891 341 383010609 846 150 DUHAR 1,129 256 383010605 1,129 256 HETMAN 1,265 278 Page 1 of 30 POPULATION AND HOUSEHOLD DETAIL FROM BLOCK TO DISTRICT LEVEL SINDH (SUJAWAL DISTRICT) ADMIN UNIT POPULATION NO OF HH 383010603 324 78 383010604 941 200 MUHARO 756 178 383010606 756 178 TANGO 1,639 335 383010610 943 191 383010611 696 144 KOTHI TC 24,856 4786 ACH 1,452 253 383010413 1,452 253 ATHARIA 2,389 487 383010406 2,389 487 CHAMAI 881 171 383010411 881 171 CHARKI 193 31 383010404 193 31 CHO BANDI 1,450 307 383010401 1,450 307 DOHO 1,856 350 383010408 1,856 350 HUR 2,230 376 383010402 2,230 376 KHADHI 1,238 238 383010403 1,238 238 KOTHI 2,194 354 383010412 2,194 354 MIRPUR SATAH 1,778 354 383010407 1,778 354 RAJAR 1,493 293 383010409 -

List of Dehs in Sindh
List of Dehs in Sindh S.No District Taluka Deh's 1 Badin Badin 1 Abri 2 Badin Badin 2 Achh 3 Badin Badin 3 Achhro 4 Badin Badin 4 Akro 5 Badin Badin 5 Aminariro 6 Badin Badin 6 Andhalo 7 Badin Badin 7 Angri 8 Badin Badin 8 Babralo-under sea 9 Badin Badin 9 Badin 10 Badin Badin 10 Baghar 11 Badin Badin 11 Bagreji 12 Badin Badin 12 Bakho Khudi 13 Badin Badin 13 Bandho 14 Badin Badin 14 Bano 15 Badin Badin 15 Behdmi 16 Badin Badin 16 Bhambhki 17 Badin Badin 17 Bhaneri 18 Badin Badin 18 Bidhadi 19 Badin Badin 19 Bijoriro 20 Badin Badin 20 Bokhi 21 Badin Badin 21 Booharki 22 Badin Badin 22 Borandi 23 Badin Badin 23 Buxa 24 Badin Badin 24 Chandhadi 25 Badin Badin 25 Chanesri 26 Badin Badin 26 Charo 27 Badin Badin 27 Cheerandi 28 Badin Badin 28 Chhel 29 Badin Badin 29 Chobandi 30 Badin Badin 30 Chorhadi 31 Badin Badin 31 Chorhalo 32 Badin Badin 32 Daleji 33 Badin Badin 33 Dandhi 34 Badin Badin 34 Daphri 35 Badin Badin 35 Dasti 36 Badin Badin 36 Dhandh 37 Badin Badin 37 Dharan 38 Badin Badin 38 Dheenghar 39 Badin Badin 39 Doonghadi 40 Badin Badin 40 Gabarlo 41 Badin Badin 41 Gad 42 Badin Badin 42 Gagro 43 Badin Badin 43 Ghurbi Page 1 of 142 List of Dehs in Sindh S.No District Taluka Deh's 44 Badin Badin 44 Githo 45 Badin Badin 45 Gujjo 46 Badin Badin 46 Gurho 47 Badin Badin 47 Jakhralo 48 Badin Badin 48 Jakhri 49 Badin Badin 49 janath 50 Badin Badin 50 Janjhli 51 Badin Badin 51 Janki 52 Badin Badin 52 Jhagri 53 Badin Badin 53 Jhalar 54 Badin Badin 54 Jhol khasi 55 Badin Badin 55 Jhurkandi 56 Badin Badin 56 Kadhan 57 Badin Badin 57 Kadi kazia -

List of Institutes Where Diploma in Commerce Is Being Offered
LIST OF INSTITUTES WHERE DIPLOMA IN COMMERCE IS BEING OFFERED 1. Banking with Computer 2. Accounts with Computer 3. Office Secretarial Practicewith English Shorthand &Typing (ES&T) 4. Insurance with Computer 5. Salesmanship with Computer S.# Region Name Of Institutions Address 1 GIB & CE, Azizabad Azizabad No. 2, Karachi 2 GIB & CE, Gulistan-e-Jauhar Block-12, Near Telephone Exchange, Gulistan-e-Jauhar, Karachi Karachi 3 GIB & CE, Lyari Plot No. 2593, Rangiwara, Lyari, Karachi 4 GIB & CE, Malir Saudabad, Near Urdu Nagar, Malir, Karachi 5 GIB & CE, Orangi Town Sector 11 1/2 Orangi Town, Karachi 1 GIB & CE, Digri Govt. Boys High School Digri 2 GIB & CE, Mirpurkhas Sattelite Town Mirpurkhas 3 GIB & CE, Khipro Near Sanghar Bye pass Khipro 4 Mirpurkhas GIB & CE, Sanghar Bakhoro Road Sanghar 5 GIB & CE, Tando Adam Near Bye Pass Tando Adam 6 GIB & CE, Mithi Near Al Mehdi Hospital, Naukot Road, Mithi 7 GIB & CE, Umerkot Near Grid Station Mirpurkhas Road Umerkot 1 GIB & CE, Jacobabad Near Shahbaz Air Base, Jacobabad 2 GIB & CE, Mirokhan Near Taluka Hospital, Mirokhan 3 GIB & CE, Shahdadkot Near Grid Station, Shahdadkot 4 Larkana GIB & CE, Kandhkot Government High School, Gulsher Muhalla 5 GIB & CE, Larkana Near Main Dari Police Station, Bakrani Road, Larkana 6 GIB & CE, Lakhi Near Water Cantt, Lakhi 7 GIB & CE, Shikarpur Near Lakhi Dar, Shikarpur 1 GIB & CE, Badin Near Total Petrol Pump, Hyderabad Road, Badin 2 GIB & CE, Dadu Court Road, Dadu 3 GIB & CE, Mehar Near Degree College, Mehar 4 GIB & CE, Latifabad Behind BISE, Latifabad-9, Hyderabad -

Sindh Bank Limited List of Operational Branches
SINDH BANK LIMITED LIST OF OPERATIONAL BRANCHES S.No. Branch Code Branch Name KARACHI BRANCHES 1 5303 ALLAMA SHABBIR AHMED USMANI ROAD (ISLAMIC) Shop No.2,3, & 4, Shaheen Heights, Block-7, KDA Scheme No.24, Gulshan-e-Iqbal, Karachi 2 0329 BUFFERZONE NAGAN CHOWRANGI BRANCH Plot No. 32, Sector 11-H, North Karachi Township Scheme, Karachi 3 0364 BHAINS COLONY BRANCH Plot No. 217, Block-A, Cattle (Bhains) Colony Landhi, Karachi 4 0366 BAHRIA COMPLEX-II BRANCH Plot # Misc.-2, Bahria Complex-II M.T. Khan Road, Karachi 5 0375 BOHRAPIR BRANCH Shop No.3 & 4, Plot Survey No.88, RC.12 Ranchore Line Quarter, Karachi 6 0391 BALDIA TOWN BRANCH Plot No.667, Anjam Colony, Badia Town, Karachi 7 0302 CLIFTON BRANCH Ground Floor, St-28, Block-5, Federation House, Clifton, Karachi 8 0303 COURT ROAD BRANCH Ground floor, G-5-A, Court View Apartments, Opposite Sindh Assembly, Karachi 9 0318 CLOTH MARKET BRANCH Shop No.28, Ground Floor, Cochinwala Market, Bunder Road Quarters, Karachi 10 0369 CIVIC CENTER BRANCH Ground Floor, Civic Center, Gulshan-e-Iqbal, Karachi 11 0325 DHORAJEE BRANCH Plot # 35/243, Block 7&8, C.P. Berar Cooperative Housing Society, Dhorajee Colony, Karachi 12 0357 DHA PHASE-II BRANCH Plot No. 13-C, Commercial Area “A”, DHA Phase-II, Karachi 13 0338 DHA Phase-IV Shop # 1,2,3, and 4, Plot No.III 9th Commercial Street, Phase-IV, DHA, Clifton Cantonment, Karachi 14 0304 DHA 26th STREET BRANCH Plot No.14-E, 26th Street Phase 5 Ext. D.H.A, Karachi 15 0372 DR. -

Sindh Through History and Representations: French
SINDH through History SINDH and Representations French Contributions to through History Sindhi Studies i Edited by Michel Boivin and Representations The book aims to make available to English readers internationally research studies carried French Contributions to out by French scholars and advanced students. The topics cover the main periods of Sindh's Sindhi Studies history, literature, architecture and anthropology and the authors seek to provide a wide-ranging and comprehensive survey of Sindh's legacy. The work provides a fresh perspective on Sindhi culture, and its interaction with the legacies of other provinces of South Asia. Contributors Michel Boivin ^^Snnabelle Collinet Frangoise Cousin Laurent Gayer Dominique-Sila Khan Pierre Lachaier Frangoise Mallison Claude Markovits Delphine Maucort OXFORD ISBN 978-0-19-547503-6 UNIVERSITY PRESS www.oup.com www.oup.com/pk RS 550 OXJORD SINDH THROUGH HISTORY AND RfPRESENTATIONS FRENCH CONTRIBUTIONS TO SINDHI STUDIES EDITED BY MICHEL BOIVIN . OXFORDUNIVERSITY PRESS OXFORDUNIVERSITY PRESS Great Clarendon Street, Oxford ox2 6DP Oxford University Press is a department of the University of Oxford. It furthers the University's objective of excellence in research, scholarship, and education by_ publishing worldwide in Oxford New York Auckland Cape Town Dar es Salaam Hong Kong Karachi Kuala Lumpur Madrid Melbourne Mexico City Nairobi New Delhi Shanghai Taipei Toronto with offices in Argentina Austria Brazil Chile Czech Republic France Greece Guatemala Hungary Italy Japan Poland Portugal Singapore South Korea Switzerland Turkey Ukraine Vietnam t Oxford is a registered trade mark of Oxford University Press in the UK and in certain other countries © Oxford University Press 2008 The moral rights of the author have been asserted First published 2008 All rights reserved. -
PAKISTAN, FOURTH QUARTER 2020: Update on Incidents According to the Armed Conflict Location & Event Data Project (ACLED) Compiled by ACCORD, 25 March 2021
PAKISTAN, FOURTH QUARTER 2020: Update on incidents according to the Armed Conflict Location & Event Data Project (ACLED) compiled by ACCORD, 25 March 2021 Number of reported incidents with at least one fatality Number of reported fatalities National borders: GADM, 6 May 2018a; administrative divisions: GADM, 6 May 2018b (ACCORD amended the geodata to reflect the merging of NWFP and FATA into Khyber Pakhtunkhwa); China/India border status: CIA, 2006; Kashmir border status: CIA, 2004; geodata of disputed borders: GADM, 6 May 2018a; Natural Earth, nodate; incident data: ACLED, 12 March 2021; coastlines and inland waters: Smith and Wessel, 1 May 2015 PAKISTAN, FOURTH QUARTER 2020: UPDATE ON INCIDENTS ACCORDING TO THE ARMED CONFLICT LOCATION & EVENT DATA PROJECT (ACLED) COMPILED BY ACCORD, 25 MARCH 2021 Contents Conflict incidents by category Number of Number of reported fatalities 1 Number of Number of Category incidents with at incidents fatalities Number of reported incidents with at least one fatality 1 least one fatality Protests 2139 0 0 Conflict incidents by category 2 Battles 87 46 158 Development of conflict incidents from December 2018 to December 2020 2 Riots 50 5 11 Explosions / Remote Methodology 3 35 20 75 violence Conflict incidents per province 4 Violence against civilians 29 22 27 Strategic developments 8 0 0 Localization of conflict incidents 4 Total 2348 93 271 Disclaimer 6 This table is based on data from ACLED (datasets used: ACLED, 12 March 2021). Development of conflict incidents from December 2018 to December 2020 This graph is based on data from ACLED (datasets used: ACLED, 12 March 2021).