Artibeus Jamaicensis) with Tacaribe Virus Ann C
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Food Choice in Frugivorous Bats
Food Choice in Frugivorous Bats Lauren Riegler Department of Biology, Trinity University ABSTRACT Frugivorous bats are important dispersers for many tropical plants and their conservation depends on furthering knowledge in their foraging behaviors and food preferences (Brosset et al. 1996). This study investigated a possible fruit preference of five frugivorous bat species (Carollia brevicauda, Artibeus lituratus, Artibeus jamaicensis, Artibeus toltecus and Platyrrhinus vittatus) found in Monteverde, Costa Rica among three wild fruit species (Solanum umbellatum, Solanum aphyodendron and Ficus pertusa) and two cultivated fruit species (Musa accuminata and Carica papaya). Fruits were presented to the bats in the Bat Jungle of Monteverde, where the foraging of bats can be closely observed. Artibeus toltecus showed a slight trend of preference for Solanum umbellatum over Solanum aphyodendron. However, due to small sample size and pseudoreplication there was no significant preference for any of the fruits by any of the bat species. RESUMEN Los murciélagos frugívoros son dispersores importantes de muchas plantas tropicales y su conservación depende del incremento de nuestro conocimiento de su comportamiento de forrajeo y preferencias dietéticas (Brosset et al. 1996). Este estudio investigó la posible predilección de cinco murciélagos frugívoros (Carollia brevicauda, Artibeus lituratus, Artibeus jamaicensis, Artibeus toltecus y Platyrrhinus vittatus) por tres especies silvestres de frutas Solanum umbellatum, Solanum aphyodendron y Ficus pertusa) y dos especies de frutas cultivadas (Musa accuminata y Carica papaya) en Monteverde, Costa Rica. Las frutas fueron presentadas a los murciélagos en la Jungla de Murciélagos de Monteverde, donde fue posible observar detenidamente el compartimiento de los murciélagos. Artibeus toltecus mostró una tendencia leve de preferencia por Solanum umbellatum. -

<I>Artibeus Jamaicensis</I>
University of Nebraska - Lincoln DigitalCommons@University of Nebraska - Lincoln Mammalogy Papers: University of Nebraska State Museum Museum, University of Nebraska State 6-1-2007 Phylogenetics and Phylogeography of the Artibeus jamaicensis Complex Based on Cytochrome-b DNA Sequences Peter A. Larsen Texas Tech University, [email protected] Steven R. Hoofer Matthew C. Bozeman Scott C. Pedersen South Dakota State University, [email protected] Hugh H. Genoways University of Nebraska - Lincoln, [email protected] See next page for additional authors Follow this and additional works at: https://digitalcommons.unl.edu/museummammalogy Part of the Biodiversity Commons, Molecular Genetics Commons, and the Zoology Commons Larsen, Peter A.; Hoofer, Steven R.; Bozeman, Matthew C.; Pedersen, Scott C.; Genoways, Hugh H.; Phillips, Carleton J.; Pumo, Dorothy E.; and Baker, Robert J., "Phylogenetics and Phylogeography of the Artibeus jamaicensis Complex Based on Cytochrome-b DNA Sequences" (2007). Mammalogy Papers: University of Nebraska State Museum. 53. https://digitalcommons.unl.edu/museummammalogy/53 This Article is brought to you for free and open access by the Museum, University of Nebraska State at DigitalCommons@University of Nebraska - Lincoln. It has been accepted for inclusion in Mammalogy Papers: University of Nebraska State Museum by an authorized administrator of DigitalCommons@University of Nebraska - Lincoln. Authors Peter A. Larsen, Steven R. Hoofer, Matthew C. Bozeman, Scott C. Pedersen, Hugh H. Genoways, Carleton J. Phillips, Dorothy E. Pumo, and Robert J. Baker This article is available at DigitalCommons@University of Nebraska - Lincoln: https://digitalcommons.unl.edu/ museummammalogy/53 Journal of Mammalogy, 88(3):712–727, 2007 PHYLOGENETICS AND PHYLOGEOGRAPHY OF THE ARTIBEUS JAMAICENSIS COMPLEX BASED ON CYTOCHROME-b DNA SEQUENCES PETER A. -

Artibeus Jamaicensis
Available online at www.sciencedirect.com R Hearing Research 184 (2003) 113^122 www.elsevier.com/locate/heares Hearing in American leaf-nosed bats. III: Artibeus jamaicensis Rickye S. He¡ner Ã, Gimseong Koay, Henry E. He¡ner Department of Psychology, University of Toledo, Toledo, OH 43606, USA Received 10 March 2003; accepted 23 July 2003 Abstract We determined the audiogram of the Jamaican fruit-eating bat (Phyllostomidae: Artibeus jamaicensis), a relatively large (40^50 g) species that, like other phyllostomids, uses low-intensity echolocation calls. A conditioned suppression/avoidance procedure with a fruit juice reward was used for testing. At 60 dB SPL the hearing range of A. jamaicensis extends from 2.8 to 131 kHz, with an average best sensitivity of 8.5 dB SPL at 16 kHz. Although their echolocation calls are low-intensity, the absolute sensitivity of A. jamaicensis and other ‘whispering’ bats does not differ from that of other mammals, including other bats. The high-frequency hearing of A. jamaicensis and other Microchiroptera is slightly higher than expected on the basis of selective pressure for passive sound localization. Analysis suggests that the evolution of echolocation may have been accompanied by the extension of their high-frequency hearing by an average of one-half octave. With respect to low-frequency hearing, all bats tested so far belong to the group of mammals with poor low-frequency hearing, i.e., those unable to hear below 500 Hz. ß 2003 Elsevier B.V. All rights reserved. Key words: Audiogram; Chiroptera; Echolocation; Evolution; Mammal 1. Introduction As part of a survey of hearing abilities in bats, we have been examining the hearing of phyllostomids With over 150 species, the family of American leaf- (Koay et al., 2002, 2003). -

BATS of the Golfo Dulce Region, Costa Rica
MURCIÉLAGOS de la región del Golfo Dulce, Puntarenas, Costa Rica BATS of the Golfo Dulce Region, Costa Rica 1 Elène Haave-Audet1,2, Gloriana Chaverri3,4, Doris Audet2, Manuel Sánchez1, Andrew Whitworth1 1Osa Conservation, 2University of Alberta, 3Universidad de Costa Rica, 4Smithsonian Tropical Research Institute Photos: Doris Audet (DA), Joxerra Aihartza (JA), Gloriana Chaverri (GC), Sébastien Puechmaille (SP), Manuel Sánchez (MS). Map: Hellen Solís, Universidad de Costa Rica © Elène Haave-Audet [[email protected]] and other authors. Thanks to: Osa Conservation and the Bobolink Foundation. [fieldguides.fieldmuseum.org] [1209] version 1 11/2019 The Golfo Dulce region is comprised of old and secondary growth seasonally wet tropical forest. This guide includes representative species from all families encountered in the lowlands (< 400 masl), where ca. 75 species possibly occur. Species checklist for the region was compiled based on bat captures by the authors and from: Lista y distribución de murciélagos de Costa Rica. Rodríguez & Wilson (1999); The mammals of Central America and Southeast Mexico. Reid (2012). Taxonomy according to Simmons (2005). La región del Golfo Dulce está compuesta de bosque estacionalmente húmedo primario y secundario. Esta guía incluye especies representativas de las familias presentes en las tierras bajas de la región (< de 400 m.s.n.m), donde se puede encontrar c. 75 especies. La lista de especies fue preparada con base en capturas de los autores y desde: Lista y distribución de murciélagos de Costa Rica. Rodríguez -

Artibeus Jamaicensis (Jamaican Fruit Bat) Family: Phyllostomidae (Leaf-Nosed Bats) Order: Chiroptera (Bats) Class: Mammalia (Mammals)
UWI The Online Guide to the Animals of Trinidad and Tobago Ecology Artibeus jamaicensis (Jamaican Fruit Bat) Family: Phyllostomidae (Leaf-nosed Bats) Order: Chiroptera (Bats) Class: Mammalia (Mammals) Fig. 1. Jamaican fruit bat, Atribeus jamaicensis. [http://www.aquablog.ca/2014/08/featured-animal-the-jamaican-fruit-bat/ downloaded 4 March 2015] TRAITS. These are medium sized species of bats, which weigh between 40-60g and grow to a length of 75-85mm with a wing span that varies between 48-67mm. The back of their body is covered with an ashy shade of brown, greyish or black, short, soft, pleasant smelling fur with white hair roots that gives the bat a faintly hoary (frosted) appearance (Fig. 1). Their ventral underfur is usually paler in colour than its dorsal underfur and back fur (Rafferty 2011). Their genus is recognized by their four pale white facial stripes above and below their eyes (Fleming et al. 1972). Their wings are broad and displays a dark grey or black colour. They have an interfemoral membrane that is thin, hairless and has a short calcar. They have a protruding nose leaf and lacks an external tail. Their ears are small, pointed and rigid with a jagged tragus. Their bottom lip is covered in warts and has a large one in the middle (Ortega and Castro-Arellano 2001). Both the bottom and top lips of the Jamaican fruit bat has sebaceous glands (Dalquest et al. 1952). Both males and females are alike (Morrison 2011). UWI The Online Guide to the Animals of Trinidad and Tobago Ecology DISTRIBUTION. -

Redalyc.Olfaction in the Fruit-Eating Bats Artibeus Lituratus and Carollia
Anais da Academia Brasileira de Ciências ISSN: 0001-3765 [email protected] Academia Brasileira de Ciências Brasil PAROLIN, LAYS C.; MIKICH, SANDRA B.; BIANCONI, GLEDSON V. Olfaction in the fruit-eating bats Artibeus lituratus and Carollia perspicillata: an experimental analysis Anais da Academia Brasileira de Ciências, vol. 87, núm. 4, octubre-diciembre, 2015, pp. 2047-2053 Academia Brasileira de Ciências Rio de Janeiro, Brasil Available in: http://www.redalyc.org/articulo.oa?id=32743236012 How to cite Complete issue Scientific Information System More information about this article Network of Scientific Journals from Latin America, the Caribbean, Spain and Portugal Journal's homepage in redalyc.org Non-profit academic project, developed under the open access initiative Anais da Academia Brasileira de Ciências (2015) 87(4): 2047-2053 (Annals of the Brazilian Academy of Sciences) Printed version ISSN 0001-3765 / Online version ISSN 1678-2690 http://dx.doi.org/10.1590/0001-3765201520140519 www.scielo.br/aabc Olfaction in the fruit-eating bats Artibeus lituratus and Carollia perspicillata: an experimental analysis LAYS C. PAROLIN1, 2, 3, SANDRA B. MIKICH1 and GLEDSON V. BIANCONI4,5 1Laboratório de Ecologia, Embrapa Florestas, Estrada da Ribeira, km 111, 83411-000 Colombo, PR, Brasil 2 Departamento de Zoologia e Botânica, Universidade Estadual Paulista “Júlio de Mesquita Filho”, Rua Cristóvão Colombo, 2265, 15054-000 São José do Rio Preto, SP, Brasil 3Escola de Saúde e Biociências, Pontifícia Universidade Católica do Paraná, Rua Imaculada Conceição, 1155, 80215-182 Curitiba, PR, Brasil 4Instituto Neotropical: Pesquisa e Conservação, Rua Purus, 33, 82520-750 Curitiba, PR, Brasil 5Instituto Federal do Paraná, Campus Pinhais, Rua Humberto de Alencar Castelo Branco, 1575, 83330-200 Pinhais, PR, Brasil Manuscript received on September 30, 2014; accepted for publication on January 19, 2015 ABSTRACT Studies suggest that frugivorous bats search and select fruit mainly by olfaction so that they can be attracted by smell alone. -
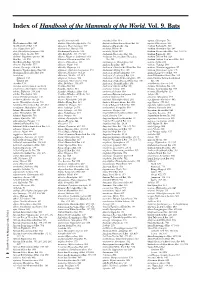
Index of Handbook of the Mammals of the World. Vol. 9. Bats
Index of Handbook of the Mammals of the World. Vol. 9. Bats A agnella, Kerivoula 901 Anchieta’s Bat 814 aquilus, Glischropus 763 Aba Leaf-nosed Bat 247 aladdin, Pipistrellus pipistrellus 771 Anchieta’s Broad-faced Fruit Bat 94 aquilus, Platyrrhinus 567 Aba Roundleaf Bat 247 alascensis, Myotis lucifugus 927 Anchieta’s Pipistrelle 814 Arabian Barbastelle 861 abae, Hipposideros 247 alaschanicus, Hypsugo 810 anchietae, Plerotes 94 Arabian Horseshoe Bat 296 abae, Rhinolophus fumigatus 290 Alashanian Pipistrelle 810 ancricola, Myotis 957 Arabian Mouse-tailed Bat 164, 170, 176 abbotti, Myotis hasseltii 970 alba, Ectophylla 466, 480, 569 Andaman Horseshoe Bat 314 Arabian Pipistrelle 810 abditum, Megaderma spasma 191 albatus, Myopterus daubentonii 663 Andaman Intermediate Horseshoe Arabian Trident Bat 229 Abo Bat 725, 832 Alberico’s Broad-nosed Bat 565 Bat 321 Arabian Trident Leaf-nosed Bat 229 Abo Butterfly Bat 725, 832 albericoi, Platyrrhinus 565 andamanensis, Rhinolophus 321 arabica, Asellia 229 abramus, Pipistrellus 777 albescens, Myotis 940 Andean Fruit Bat 547 arabicus, Hypsugo 810 abrasus, Cynomops 604, 640 albicollis, Megaerops 64 Andersen’s Bare-backed Fruit Bat 109 arabicus, Rousettus aegyptiacus 87 Abruzzi’s Wrinkle-lipped Bat 645 albipinnis, Taphozous longimanus 353 Andersen’s Flying Fox 158 arabium, Rhinopoma cystops 176 Abyssinian Horseshoe Bat 290 albiventer, Nyctimene 36, 118 Andersen’s Fruit-eating Bat 578 Arafura Large-footed Bat 969 Acerodon albiventris, Noctilio 405, 411 Andersen’s Leaf-nosed Bat 254 Arata Yellow-shouldered Bat 543 Sulawesi 134 albofuscus, Scotoecus 762 Andersen’s Little Fruit-eating Bat 578 Arata-Thomas Yellow-shouldered Talaud 134 alboguttata, Glauconycteris 833 Andersen’s Naked-backed Fruit Bat 109 Bat 543 Acerodon 134 albus, Diclidurus 339, 367 Andersen’s Roundleaf Bat 254 aratathomasi, Sturnira 543 Acerodon mackloti (see A. -

Bats of the Grenadine Islands, West Indies, and Placement of Koopman's Line
University of Nebraska - Lincoln DigitalCommons@University of Nebraska - Lincoln Mammalogy Papers: University of Nebraska State Museum Museum, University of Nebraska State 7-2010 Bats of the Grenadine Islands, West Indies, and Placement of Koopman's Line Hugh H. Genoways University of Nebraska - Lincoln, [email protected] Gary G. Kwiecinski University of Scranton Peter A. Larsen Texas Tech University, [email protected] Scott C. Pedersen South Dakota State University, [email protected] Roxanne J. Larsen Texas Tech University, [email protected] See next page for additional authors Follow this and additional works at: https://digitalcommons.unl.edu/museummammalogy Part of the Biodiversity Commons, Other Ecology and Evolutionary Biology Commons, and the Zoology Commons Genoways, Hugh H.; Kwiecinski, Gary G.; Larsen, Peter A.; Pedersen, Scott C.; Larsen, Roxanne J.; Hoffman, Justin D.; de Silva, Mark; Phillips, Carleton J.; and Baker, Robert J., "Bats of the Grenadine Islands, West Indies, and Placement of Koopman's Line" (2010). Mammalogy Papers: University of Nebraska State Museum. 129. https://digitalcommons.unl.edu/museummammalogy/129 This Article is brought to you for free and open access by the Museum, University of Nebraska State at DigitalCommons@University of Nebraska - Lincoln. It has been accepted for inclusion in Mammalogy Papers: University of Nebraska State Museum by an authorized administrator of DigitalCommons@University of Nebraska - Lincoln. Authors Hugh H. Genoways, Gary G. Kwiecinski, Peter A. Larsen, Scott C. Pedersen, Roxanne J. Larsen, Justin D. Hoffman, Mark de Silva, Carleton J. Phillips, and Robert J. Baker This article is available at DigitalCommons@University of Nebraska - Lincoln: https://digitalcommons.unl.edu/ museummammalogy/129 Chiroptera Neotropical 16(1), July 2010 BATS OF THE GRENADINE ISLANDS, WEST INDIES, AND PLACEMENT OF KOOPMAN’S LINE Hugh H. -

Mammals of Central Mexico Juan Cruzado Cortes and Venkat Sankar (Author; [email protected]) August 5-10, 2019
Venkat Sankar 2019 1 Mammals of Central Mexico Juan Cruzado Cortes and Venkat Sankar (author; [email protected]) August 5-10, 2019 Beautiful scenery at Barrancas de Aguacatitla; Mexican Volcano Mouse; Mexican Ground Squirrel Introduction While searching for mammals in Oaxaca this March, Juan told me that a mammalogist friend of his in Tabasco, Dr. Rafael Avila Flores, had found some amazing bats in an area of karst near the state’s border with Chiapas. These included a number of impressive and distinctive species I’ve long wanted to see, like the Sword-nosed Bat and White-winged Vampire Bat. I had to visit, and with few breaks this summer thanks to academic commitments, this was the perfect choice for a long weekend’s trip. Juan suggested we spend a few days in Mexico City with another biologist friend, Melany Aguilar Lopez, to find several endemics of the Mexican Plateau, and then connect to Tabasco. And so a plan was formed! Itinerary 8/5/19: Mexico City—RB Barrancas de Metztitlan (O/N UMA Santana) 8/6/19: RB Barrancas de Metztitlan—PN el Chico (O/N Mineral de Chico) 8/7/19: PN el Chico—Tlaxco—Area Communitaria Milpa Alta (O/N San Pablo Oztotepec) 8/8/19: Milpa Alta—Villahermosa (flight)—Ejido Poana (O/N Tacotalpa) 8/9/19: Full day exploring Ejido Poana (O/N Tacotalpa) 8/10/19: Early deparature from Villahermosa Key sites RB Barrancas de Metztitlan This scenic area of deep canyons spans a diverse range of habitats from dry pine-oak forest on the rim, into high desert, and eventually tropical deciduous forest on the canyon floor. -

Bioacoustical Characterization of Phyllostomidae Bats in Colombian Low Montane Rain Forest
Rev. Biodivers. Neotrop. ISSN 2027-8918 e-ISSN 2256-5426 Abril-Junio 2017; 7 (2): 119-33 119 DOI: http://dx.doi.org/10.18636/bioneotropical.v7i2.600 Bioacoustical characterization of Phyllostomidae bats in Colombian low montane rain forest Caracterización bioacústica de murciélagos Filostómidos en un bosque húmedo montano bajo colombiano Paula Catalina Pinilla-Cortés1, Abelardo Rodríguez-Bolaños2 Abstract The emission of ultrasound allows bats make decisive tasks associated with the interpretation of their su- rroundings, displacement, orientation and obtaining food. In the case of Phyllostomidae bats, the emissions show high frequencies and low intensities, similarly they complement largely by the sense of smell and in a less proportion, by sight. Objective: This study presents the characterization of bioacoustics emissions for seven species: Artibeus jamaicensis (Leach, 1821) Carollia brevicauda (Schinz, 1821), Carollia pers- picillata (Linnaeus, 1758), Phyllostomus hastatus (Pallas, 1767), Phyllostomus discolor (Wagner, 1843) Sturnira luisi (Davis, 1980), Sturnira lilium (E.Geoffroy, 1810). Methodology: The acoustic records have been reported in a humid forest in San Francisco,Cundinamarca, Colombia, using the autonomous recorder Song Meter SM2 Bat (Wild Life Acoustics). The emissions were obtained applying closed recording booth space flight method and after, they were visualized using Sonobat 2.9.4 Software.Results: Spectrograms were obtained and a consensus among the spectral values recorded by each specie, with the mean and the standard deviation, then some values are contrasted. Conclusion: Recognition of modulated structures, numerous harmonics and high frequencies. Likewise, after making contrast of spectral values, which are mainly referred to the high or initial frequency (Hif), low or initial frequency (Lof) and duration (ms), with different authors, it study recognizes the need to expand studies that take into account characteristics of Phyllostomidae individuals in field or under controlled conditions. -

Check out the Listing of Mammal Species Found
30 MP EPN TMN HV Taxa Colloquial name R P R ORDER: ARTIODACTYLA Family: Cervidae X V, Mazama americana Red Brocket Deer WC Mazama pandora Gray Brocket Deer X V, Odocoileus virginianus truei White-tailed Deer MM Family: Tayassuidae X V, Pecari tajacu Collared Peccary WC Tayassu pecari White-lipped Peccary X WC ORDER: Carnivora Family: Canidae Canis latrans goldmani Coyote V? Urocyon cinereoargenteus X V, fraterculus Gray Fox WC Family: Felidae X V, Leopardus pardalis pardalis Ocelot WC X V, Leopardus wiedii yucatanicus Margay WC X V, Panthera onca hernandesii Jaguar WC X X, Puma concolor mayensis Puma MM Puma yagouaroundi fossata Jaguarundi x V Family: Mephitidae Conepatus leuconotus American Hog-nosed Skunk Conepatus semistriatus WC yucatanesis Striped Hog-nosed Skunk Spilogale angustifrons Southern Spotted Skunk MM, Eira barbara senex Tayra V, Galictis vittata canaster Grison V X V, Lontra longicaudis annectens Neotropical Otter WC Mustela frenata perda Long-tailed Weasel X MM, Hidden Valley Management Plan 2010 – 2015 Volume 2 31 MP EPN TMN HV Taxa Colloquial name R P R V, Family: Procyonidae Bassariscus sumichrasti Ringtail / Cacomistle WC Nasua narica Coatimundi X V Potos flavus chiriquensis Kinkajou X Procyon lotor shufeldti Raccon X WC ORDER: CHIROPTERA Family: Emballonuridae Balantiopteryx io Least Sac-winged Bat Centronycteris centralis Thomas' Bat Diclidurus albus Northern Ghost Bat MM Peropteryx kappleri Greater Dog-like Bat MM Peropteryx macrotis Lesser Dog-like Bat MM Rhynchonycteris naso Proboscis Bat Saccopteryx bilineata -

Ecomorphological Analysis of the Masticatory Apparatus in the Seed-Eating Bats, Genus Chiroderma (Chiroptera: Phyllostomidae)
J. Zool., Lond. (2005) 266, 355–364 C 2005 The Zoological Society of London Printed in the United Kingdom doi:10.1017/S0952836905007053 Ecomorphological analysis of the masticatory apparatus in the seed-eating bats, genus Chiroderma (Chiroptera: Phyllostomidae) Marcelo R. Nogueira1*, Leandro R. Monteiro2, Adriano L. Peracchi1 and Alexandre F. B. de Araujo´ 3 1 Laboratorio´ de Mastozoologia – IB, Universidade Federal Rural do Rio de Janeiro, 23890-000, Seropedica,´ RJ, Brazil 2 Laboratorio´ de Cienciasˆ Ambientais – CBB, Universidade Estadual do Norte Fluminense, 28013-600, Campos dos Goytacazes, RJ, Brazil 3 Laboratorio´ de Ecologia de Vertebrados, IB, Universidade Federal Rural do Rio de Janeiro, Brazil (Accepted 5 January 2005) Abstract Recent data have shown that owing to their seed-predator capacity Chiroderma doriae and Chiroderma villosum trophically depart from all previously studied species within the canopy fruit-bat ensemble. In this paper, the hypothesis that morphological adaptations related to granivory have evolved in these bats is investigated and discussed. A canonical variate analysis was used to search for possible divergent trends between the masticatory apparatus of Chiroderma and other stenodermatines currently recognized in the same ensemble. A total of 142 specimens representative of eight species was included in the analysis. Species of Chiroderma can be discriminated from all other species in the sample based on the increased development of masseter-related variables (height of the anterior zygomatic arch, masseter moment arm, and masseter volume), which, in conjunction with other morphological characteristics (dentition and gape angle) discussed herein, corroborates the evolution of durophagy in this group. A complementary analysis based on a Mantel test revealed that the pattern of morphological differentiation that emerged from the canonical variate analysis does not agree with the one expected based solely on the phylogenetic relationships adopted for the canopy fruit-bats studied here.