Artery of the Superior Orbital Fissure: an Undescribed Branch from the Pterygopalatine Segment of the Maxillary Artery to the Or
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

MR Imaging of the Orbital Apex
J Korean Radiol Soc 2000;4 :26 9-0 6 1 6 MR Imaging of the Orbital Apex: An a to m y and Pat h o l o g y 1 Ho Kyu Lee, M.D., Chang Jin Kim, M.D.2, Hyosook Ahn, M.D.3, Ji Hoon Shin, M.D., Choong Gon Choi, M.D., Dae Chul Suh, M.D. The apex of the orbit is basically formed by the optic canal, the superior orbital fis- su r e , and their contents. Space-occupying lesions in this area can result in clinical d- eficits caused by compression of the optic nerve or extraocular muscles. Even vas c u l a r changes in the cavernous sinus can produce a direct mass effect and affect the orbit ap e x. When pathologic changes in this region is suspected, contrast-enhanced MR imaging with fat saturation is very useful. According to the anatomic regions from which the lesions arise, they can be classi- fied as belonging to one of five groups; lesions of the optic nerve-sheath complex, of the conal and intraconal spaces, of the extraconal space and bony orbit, of the cav- ernous sinus or diffuse. The characteristic MR findings of various orbital lesions will be described in this paper. Index words : Orbit, diseases Orbit, MR The apex of the orbit is a complex region which con- tains many nerves, vessels, soft tissues, and bony struc- Anatomy of the orbital apex tures such as the superior orbital fissure and the optic canal (1-3), and is likely to be involved in various dis- The orbital apex region consists of the optic nerve- eases (3). -

Branches of the Maxillary Artery of the Dromedary, Camelus Dromedarius
Table 3.5: Branches of the Maxillary Artery of the Dromedary, Camelus dromedarius Artery Origin Course Distribution Departs from common trunk with the deep temporal vessels, close to mandibular foramen; traverses mandibular canal, supplying Mandibular dentition; lower lip; Inferior Alveolar Maxillary Artery mandibular dentition. Terminates as mental anastomoses freely with ventral ramus artery after exiting at mental foramen, of the facial artery. whereupon supplies skin, mucosa, and muscle of the lower lip. Single deep temporal vessel is first major dorsal branch of the MA; ascends deep to the coronoid Deep Temporal Maxillary Artery Temporalis muscle process and fans out on the deep surface of the temporalis muscle. Lower lateral branch of deep temporal artery; passes through the mandibular incisure and Masseteric Deep Temporal Artery Masseter muscle curves rostrally to pierce the internal surface of the masseter muscle. Proximal to the foramen orbitorotundum and optic foramen, numerous rami anastomotica connect the maxillary artery to the carotid rete. Carotid rete, ophthalmic rete, external Ramus anastomoticus Maxillary Artery The network in the dromedary is extensive, ophthalmic artery; intracranial cavity forming a plexus between the carotid and ophthalmic retia, and giving rise to the external ophthalmic artery. Condenses from a dense retial mat (composed of maxillary rami, the extradural/extracranial portion of the carotid rete, and the ophthalmic Extraocular muscles, periorbita, External Ophthalmic MA/CR/OR rete). Perfuses the majority of the periorbita, lacrimal gland including branches to the extraocular muscles and the lacrimal gland Lateral branch of the MA, begins opposite the rami anastomotica; traverses parenchyma orbital Supplies the buccal fat pad, Buccal MA fossa, between malar and anterior border of buccinator; contributes ventral coronoid process. -

Gross and Micro-Anatomical Study of the Cavernous Segment of the Abducens Nerve and Its Relationships to Internal Carotid Plexus: Application to Skull Base Surgery
brain sciences Article Gross and Micro-Anatomical Study of the Cavernous Segment of the Abducens Nerve and Its Relationships to Internal Carotid Plexus: Application to Skull Base Surgery Grzegorz Wysiadecki 1,* , Maciej Radek 2 , R. Shane Tubbs 3,4,5,6,7 , Joe Iwanaga 3,5,8 , Jerzy Walocha 9 , Piotr Brzezi ´nski 10 and Michał Polguj 1 1 Department of Normal and Clinical Anatomy, Chair of Anatomy and Histology, Medical University of Lodz, ul. Zeligowskiego˙ 7/9, 90-752 Łód´z,Poland; [email protected] 2 Department of Neurosurgery, Spine and Peripheral Nerve Surgery, Medical University of Lodz, University Hospital WAM-CSW, 90-549 Łód´z,Poland; [email protected] 3 Department of Neurosurgery, Tulane Center for Clinical Neurosciences, Tulane University School of Medicine, New Orleans, LA 70112, USA; [email protected] (R.S.T.); [email protected] (J.I.) 4 Department of Neurosurgery and Ochsner Neuroscience Institute, Ochsner Health System, New Orleans, LA 70433, USA 5 Department of Neurology, Tulane Center for Clinical Neurosciences, Tulane University School of Medicine, New Orleans, LA 70112, USA 6 Department of Anatomical Sciences, St. George’s University, Grenada FZ 818, West Indies 7 Department of Surgery, Tulane University School of Medicine, New Orleans, LA 70112, USA 8 Department of Anatomy, Kurume University School of Medicine, 67 Asahi-machi, Kurume, Fukuoka 830-0011, Japan Citation: Wysiadecki, G.; Radek, M.; 9 Department of Anatomy, Jagiellonian University Medical College, 33-332 Kraków, Poland; Tubbs, R.S.; Iwanaga, J.; Walocha, J.; [email protected] Brzezi´nski,P.; Polguj, M. -

The Anatomic Analysis of the Vidian Canal and the Surrounding
Braz J Otorhinolaryngol. 2019;85(2):136---143 Brazilian Journal of OTORHINOLARYNGOLOGY www.bjorl.org ORIGINAL ARTICLE The anatomic analysis of the vidian canal and the surrounding structures concerning vidian neurectomy ଝ using computed tomography scans a,∗ a b Gülay Ac¸ar , Aynur Emine C¸ic¸ekcibas¸ı , ˙Ibrahim C¸ukurova , c a d Kemal Emre Özen , Muzaffer ¸ekerS , ˙Ibrahim Güler a Necmettin Erbakan University, Meram Faculty of Medicine, Department of Anatomy, Konya, Turkey b Health Sciences University, Izmir Tepecik Trainig and Research Hospital, Department of Otolaryngology-Head and Neck Surgery, Izmir, Turkey c Katip C¸elebi University, Faculty of Medicine, Department of Anatomy, Izmir, Turkey d Selcuk University, Faculty of Medicine, Department of Radiology, Konya, Turkey Received 15 September 2017; accepted 8 November 2017 Available online 26 December 2017 KEYWORDS Abstract Intrasphenoid Introduction: The type of endoscopic approach chosen for vidian neurectomy can be specified septum; by evaluating the vidian canal and the surrounding sphenoid sinus structures. Morphometric Objective: The variations and morphometry of the vidian canal were investigated, focusing on analysis; the functional correlations between them which are crucial anatomical landmarks for preoper- Pterygoid process ative planning. pneumatization; Methods: This study was performed using paranasal multidetector computed tomography Vidian canal; images that were obtained with a section thickening of 0.625 mm of 250 adults. Vidian neurectomy Results: The distributions of 500 vidian canal variants were categorized as follows; Type 1, within the sphenoid corpus (55.6%); Type 2, partially protruding into the sphenoid sinus (34.8%); Type 3, within the sphenoid sinus (9.6%). The pneumatization of the pterygoid process is mostly seen in vidian canal Type 2 (72.4%) and Type 3 (95.8%) (p < 0.001). -

Entrapment Neuropathy of the Central Nervous System. Part II. Cranial
Entrapment neuropathy of the Cranial nerves central nervous system. Part II. Cranial nerves 1-IV, VI-VIII, XII HAROLD I. MAGOUN, D.O., F.A.A.O. Denver, Colorado This article, the second in a series, significance because of possible embarrassment considers specific examples of by adjacent structures in that area. The same entrapment neuropathy. It discusses entrapment can occur en route to their desti- nation. sources of malfunction of the olfactory nerves ranging from the The first cranial nerve relatively rare anosmia to the common The olfactory nerves (I) arise from the nasal chronic nasal drip. The frequency of mucosa and send about twenty central proces- ocular defects in the population today ses through the cribriform plate of the ethmoid bone to the inferior surface of the olfactory attests to the vulnerability of the optic bulb. They are concerned only with the sense nerves. Certain areas traversed by of smell. Many normal people have difficulty in each oculomotor nerve are pointed out identifying definite odors although they can as potential trouble spots. It is seen perceive them. This is not of real concern. The how the trochlear nerves are subject total loss of smell, or anosmia, is the significant to tension, pressure, or stress from abnormality. It may be due to a considerable variety of causes from arteriosclerosis to tu- trauma to various bony components morous growths but there is another cause of the skull. Finally, structural which is not usually considered. influences on the abducens, facial, The cribriform plate fits within the ethmoid acoustic, and hypoglossal nerves notch between the orbital plates of the frontal are explored. -

Endovascular Approach to Ruptured Sphenopalatine Artery: a Case Report and Literature Review
J Spine Res Surg 2021; 3 (2): 037-044 DOI: 10.26502/fjsrs0028 Case Report Endovascular Approach to Ruptured Sphenopalatine Artery: A Case Report and Literature Review Ram Saha1, Abu Bakar Siddik2, Masum Rahman3, Samar Ikram3, Cecile Riviere-cazaux4, Abdullah Alamgir5, Badrul Alam Mondal6, Quazi Deen Mohammad6, Sirajee Shafiqul Islam 7* 1Department of Neurology, Virginia Commonwealth University, VA, USA 2Department of Pain Medicine, Mayo Clinic, Jacksonville, Florida, USA 3Department of Neurological Surgery, Mayo Clinic, MN, USA 4Mayo Clinic Alix school of medicine, Rochester, MN, USA 5Department of Neurosurgery, National Institute of Neurosciences & Hospital, Dhaka, Bangladesh 6Department of Neurology, National Institute of Neurosciences & Hospital, Dhaka, Bangladesh 7Department of Interventional Neurology, National Institute of Neurosciences & Hospital, Dhaka, Bangladesh *Corresponding Author: Dr. Sirajee Shafiqul Islam, Associate Professor, Department of Interventional Neurology, National Institute of Neurosciences & Hospital, Dhaka, Bangladesh Received: 14 May 2021; Accepted: 25 May 2021; Published: 31 May 2021 Citation: Ram Saha, Abu Bakar Siddik, Masum Rahman, Samar Ikram, Cecile Riviere-cazaux, Abdullah Alamgir, Badrul Alam Mondal, Quazi Deen Mohammad, Sirajee Shafiqul Islam. Endovascular Approach to Ruptured Sphenopalatine Artery: A Case Report and Literature Review. Journal of Spine Research and Surgery 3 (2021): 037- 044. Abstract Epistaxis is a rare complication following the endonasal skull-base chordoma through an endonasal approach. approach of skull base surgery. Conservative methods An endovascular catheter digital subtraction angiogram like anterior and posterior nasal packing can be useful, identified the cause of epistaxis as a rupture of the left but when these fail, a neuro-interventional technique sphenopalatine artery branch of the left external carotid can be used as a last-resort measure in cases of severe artery. -

Morfofunctional Structure of the Skull
N.L. Svintsytska V.H. Hryn Morfofunctional structure of the skull Study guide Poltava 2016 Ministry of Public Health of Ukraine Public Institution «Central Methodological Office for Higher Medical Education of MPH of Ukraine» Higher State Educational Establishment of Ukraine «Ukranian Medical Stomatological Academy» N.L. Svintsytska, V.H. Hryn Morfofunctional structure of the skull Study guide Poltava 2016 2 LBC 28.706 UDC 611.714/716 S 24 «Recommended by the Ministry of Health of Ukraine as textbook for English- speaking students of higher educational institutions of the MPH of Ukraine» (minutes of the meeting of the Commission for the organization of training and methodical literature for the persons enrolled in higher medical (pharmaceutical) educational establishments of postgraduate education MPH of Ukraine, from 02.06.2016 №2). Letter of the MPH of Ukraine of 11.07.2016 № 08.01-30/17321 Composed by: N.L. Svintsytska, Associate Professor at the Department of Human Anatomy of Higher State Educational Establishment of Ukraine «Ukrainian Medical Stomatological Academy», PhD in Medicine, Associate Professor V.H. Hryn, Associate Professor at the Department of Human Anatomy of Higher State Educational Establishment of Ukraine «Ukrainian Medical Stomatological Academy», PhD in Medicine, Associate Professor This textbook is intended for undergraduate, postgraduate students and continuing education of health care professionals in a variety of clinical disciplines (medicine, pediatrics, dentistry) as it includes the basic concepts of human anatomy of the skull in adults and newborns. Rewiewed by: O.M. Slobodian, Head of the Department of Anatomy, Topographic Anatomy and Operative Surgery of Higher State Educational Establishment of Ukraine «Bukovinian State Medical University», Doctor of Medical Sciences, Professor M.V. -

LETTERS to the EDITOR. Middle Cerebral Artery Tortuosity Associated
J Neurosurg 130:1763–1788, 2019 Neurosurgical Forum LETTERS TO THE EDITOR Middle cerebral artery tortuosity tective factors against aneurysm formation.” Nevertheless, according to that explanation, it can be inferred that the associated with aneurysm incidence of aneurysms in patients with local tortuosity development should be decreased rather than increased. Therefore, it would be better for the authors to provide an in-depth ex- planation about the above results and arguments. TO THE EDITOR: We read with great interest the ar- Second, the authors stated, “There are a few rare ge- ticle by Kliś et al.2 (Kliś KM, Krzyżewski RM, Kwinta netic syndromes that are linked to the presence of vessel BM, et al: Computer-aided analysis of middle cerebral tortuosity, such as artery tortuosity syndrome or Loeys- artery tortuosity: association with aneurysm develop- Dietz syndrome.” The genetic syndromes they mention ment. J Neurosurg [epub ahead of print May 18, 2018; are systemic lesions involving multiple parts of vessels DOI: 10.3171/2017.12.JNS172114]). The authors conclude of the body and therefore often involve multiple intracra- that “an increased deviation of the middle cerebral artery nial aneurysms.1,3,5 However, this article did not provide (MCA) from a straight axis (described by relative length detailed information on the characteristics of intracranial [RL]), a decreased sum of all MCA angles (described by aneurysms, for example, the incidence of multiple aneu- sum of angle metrics [SOAM]), a local increase of the rysms, the specific sites of the MCA aneurysms (M1, M2, MCA angle heterogeneity, and an increase in changes in M3, M4), and the size of the aneurysms, etc. -
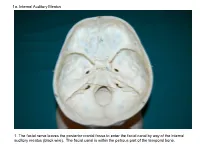
1A. Internal Auditory Meatus
1a. Internal Auditory Meatus 1. The facial nerve leaves the posterior cranial fossa to enter the facial canal by way of the internal auditory meatus (black wire). The facial canal is within the petrous part of the temporal bone. 1b. Internal Auditory Meatus The facial nerve leaves the posterior cranial fossa to enter the facial canal by way of the internal auditory meatus (black wire). 2. Hiatus of the Canal and Groove for the Greater Superficial Petrosal Nerve The greater superficial petrosal nerve leaves the facial canal to enter the middle cranial fossa by way of the hiatus of the canal for the greater superficial petrosal nerve (black wire). 3. Pterygoid Canal at Anterior Lip of the Lacerate Foramen The greater superficial petrosal nerve is joined by the deep petrosal nerve to form the nerve of the pterygoid canal (black and red wire). This nerve leaves the middle cranial fossa to enter the pterygopalatine fossa by way of the pterygoid canal. The posterior opening of the pterygoid canal is at the anterior lip of the lacerate foramen. The greater superficial nerve and the deep petrosal nerve travel within the cavernous sinus. 4. Pterygopalatine Fossa Seen Through the Pterygomaxillary Fissure The anterior opening of the pterygoid canal is into the pterygopalatine fossa (black wire). The pterygopalatine fossa is located medial to the pterygomaxillary fissure and contains the pterygopalatine ganglion. 5. External Auditory Meatus The chorda tympani nerve leaves the facial canal and crosses the middle ear (black wire). It then leaves the middle ear to arrive in the infratemporal fossa by way of the petrotympanic fissure. -

Dissection and Exposure of the Whole Course of Deep Nerves in Human Head Specimens After Decalcification
Hindawi Publishing Corporation International Journal of Otolaryngology Volume 2012, Article ID 418650, 7 pages doi:10.1155/2012/418650 Research Article Dissection and Exposure of the Whole Course of Deep Nerves in Human Head Specimens after Decalcification Longping Liu, Robin Arnold, and Marcus Robinson Discipline of Anatomy and Histology, University of Sydney, Anderson Stuart Building F13, Sydney, NSW 2006, Australia Correspondence should be addressed to Marcus Robinson, [email protected] Received 29 July 2011; Revised 10 November 2011; Accepted 12 December 2011 AcademicEditor:R.L.Doty Copyright © 2012 Longping Liu et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited. The whole course of the chorda tympani nerve, nerve of pterygoid canal, and facial nerves and their relationships with surrounding structures are complex. After reviewing the literature, it was found that details of the whole course of these deep nerves are rarely reported and specimens displaying these nerves are rarely seen in the dissecting room, anatomical museum, or atlases. Dissections were performed on 16 decalcified human head specimens, exposing the chorda tympani and the nerve connection between the geniculate and pterygopalatine ganglia. Measurements of nerve lengths, branching distances, and ganglia size were taken. The chorda tympani is a very fine nerve (0.44 mm in diameter within the tympanic cavity) and approximately 54 mm in length. The mean length of the facial nerve from opening of internal acoustic meatus to stylomastoid foramen was 52.5 mm. -

MBB: Head & Neck Anatomy
MBB: Head & Neck Anatomy Skull Osteology • This is a comprehensive guide of all the skull features you must know by the practical exam. • Many of these structures will be presented multiple times during upcoming labs. • This PowerPoint Handout is the resource you will use during lab when you have access to skulls. Mind, Brain & Behavior 2021 Osteology of the Skull Slide Title Slide Number Slide Title Slide Number Ethmoid Slide 3 Paranasal Sinuses Slide 19 Vomer, Nasal Bone, and Inferior Turbinate (Concha) Slide4 Paranasal Sinus Imaging Slide 20 Lacrimal and Palatine Bones Slide 5 Paranasal Sinus Imaging (Sagittal Section) Slide 21 Zygomatic Bone Slide 6 Skull Sutures Slide 22 Frontal Bone Slide 7 Foramen RevieW Slide 23 Mandible Slide 8 Skull Subdivisions Slide 24 Maxilla Slide 9 Sphenoid Bone Slide 10 Skull Subdivisions: Viscerocranium Slide 25 Temporal Bone Slide 11 Skull Subdivisions: Neurocranium Slide 26 Temporal Bone (Continued) Slide 12 Cranial Base: Cranial Fossae Slide 27 Temporal Bone (Middle Ear Cavity and Facial Canal) Slide 13 Skull Development: Intramembranous vs Endochondral Slide 28 Occipital Bone Slide 14 Ossification Structures/Spaces Formed by More Than One Bone Slide 15 Intramembranous Ossification: Fontanelles Slide 29 Structures/Apertures Formed by More Than One Bone Slide 16 Intramembranous Ossification: Craniosynostosis Slide 30 Nasal Septum Slide 17 Endochondral Ossification Slide 31 Infratemporal Fossa & Pterygopalatine Fossa Slide 18 Achondroplasia and Skull Growth Slide 32 Ethmoid • Cribriform plate/foramina -

Anatomy of the Ophthalmic Artery: Embryological Consideration
REVIEW ARTICLE doi: 10.2176/nmc.ra.2015-0324 Neurol Med Chir (Tokyo) 56, 585–591, 2016 Online June 8, 2016 Anatomy of the Ophthalmic Artery: Embryological Consideration Naoki TOMA1 1Department of Neurosurgery, Mie University Graduate School of Medicine, Tsu, Mie, Japan Abstract There are considerable variations in the anatomy of the human ophthalmic artery (OphA), such as anom- alous origins of the OphA and anastomoses between the OphA and the adjacent arteries. These anatomi- cal variations seem to attribute to complex embryology of the OphA. In human embryos and fetuses, primitive dorsal and ventral ophthalmic arteries (PDOphA and PVOphA) form the ocular branches, and the supraorbital division of the stapedial artery forms the orbital branches of the OphA, and then numerous anastomoses between the internal carotid artery (ICA) and the external carotid artery (ECA) systems emerge in connection with the OphA. These developmental processes can produce anatomical variations of the OphA, and we should notice these variations for neurosurgical and neurointerventional procedures. Key words: ophthalmic artery, anatomy, embryology, stapedial artery, primitive maxillary artery Introduction is to elucidate the anatomical variation of the OphA from the embryological viewpoint. The ophthalmic artery (OphA) consists of ocular and orbital branches. The ocular branches contribute to Embryology and Anatomy the blood supply of the optic apparatus, namely, the of the OphA optic nerve and the retina, and the orbital branches supply the optic adnexae, such