Effects of Nonionic Contrast Media on Platelet Aggregation
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Pharmacologyonline 2: 727-753 (2010) Ewsletter Bradu and Rossini
Pharmacologyonline 2: 727-753 (2010) ewsletter Bradu and Rossini COTRAST AGETS - IODIATED PRODUCTS. SECOD WHO-ITA / ITA-OMS 2010 COTRIBUTIO O AGGREGATE WHO SYSTEM-ORGA CLASS DISORDERS AD/OR CLUSTERIG BASED O REPORTED ADVERSE REACTIOS/EVETS Dan Bradu and Luigi Rossini* Servizio Nazionale Collaborativo WHO-ITA / ITA-OMS, Università Politecnica delle Marche e Progetto di Farmacotossicovigilanza, Azienda Ospedaliera Universitaria Ospedali Riuniti di Ancona, Regione Marche, Italia Summary From the 2010 total basic adverse reactions and events collected as ADRs preferred names in the WHO-Uppsala Drug Monitoring Programme, subdivided in its first two twenty years periods as for the first seven iodinated products diagnostic contrast agents amidotrizoate, iodamide, iotalamate, iodoxamate, ioxaglate, iohexsol and iopamidol, their 30 WHO-system organ class disorders (SOCDs) aggregates had been compared. Their common maximum 97% levels identified six SOCDs only, apt to evaluate the most frequent single ADRs for each class, and their percentual normalization profiles for each product. The WILKS's chi square statistics for the related contingency tables, and Gabriel’s STP procedure applied to the extracted double data sets then produced profile binary clustering, as well as Euclidean confirmatory plots. They finally showed similar objectively evaluated autoclassificative trends of these products, which do not completely correspond to their actual ATC V08A A, B and C subdivision: while amidotrizoate and iotalamate, and respectively iohesol and iopamidol are confirmed to belong to the A and B subgroups, ioxaglate behaves fluctuating within A, B and C, but iodamide looks surprizingly, constantly positioned together with iodoxamate as binary/ternary C associated. In view of the recent work of Campillos et al (Science, 2008) which throws light on the subject, the above discrepancies do not appear anymore unexpected or alarming. -

ACR Manual on Contrast Media
ACR Manual On Contrast Media 2021 ACR Committee on Drugs and Contrast Media Preface 2 ACR Manual on Contrast Media 2021 ACR Committee on Drugs and Contrast Media © Copyright 2021 American College of Radiology ISBN: 978-1-55903-012-0 TABLE OF CONTENTS Topic Page 1. Preface 1 2. Version History 2 3. Introduction 4 4. Patient Selection and Preparation Strategies Before Contrast 5 Medium Administration 5. Fasting Prior to Intravascular Contrast Media Administration 14 6. Safe Injection of Contrast Media 15 7. Extravasation of Contrast Media 18 8. Allergic-Like And Physiologic Reactions to Intravascular 22 Iodinated Contrast Media 9. Contrast Media Warming 29 10. Contrast-Associated Acute Kidney Injury and Contrast 33 Induced Acute Kidney Injury in Adults 11. Metformin 45 12. Contrast Media in Children 48 13. Gastrointestinal (GI) Contrast Media in Adults: Indications and 57 Guidelines 14. ACR–ASNR Position Statement On the Use of Gadolinium 78 Contrast Agents 15. Adverse Reactions To Gadolinium-Based Contrast Media 79 16. Nephrogenic Systemic Fibrosis (NSF) 83 17. Ultrasound Contrast Media 92 18. Treatment of Contrast Reactions 95 19. Administration of Contrast Media to Pregnant or Potentially 97 Pregnant Patients 20. Administration of Contrast Media to Women Who are Breast- 101 Feeding Table 1 – Categories Of Acute Reactions 103 Table 2 – Treatment Of Acute Reactions To Contrast Media In 105 Children Table 3 – Management Of Acute Reactions To Contrast Media In 114 Adults Table 4 – Equipment For Contrast Reaction Kits In Radiology 122 Appendix A – Contrast Media Specifications 124 PREFACE This edition of the ACR Manual on Contrast Media replaces all earlier editions. -

Estonian Statistics on Medicines 2016 1/41
Estonian Statistics on Medicines 2016 ATC code ATC group / Active substance (rout of admin.) Quantity sold Unit DDD Unit DDD/1000/ day A ALIMENTARY TRACT AND METABOLISM 167,8985 A01 STOMATOLOGICAL PREPARATIONS 0,0738 A01A STOMATOLOGICAL PREPARATIONS 0,0738 A01AB Antiinfectives and antiseptics for local oral treatment 0,0738 A01AB09 Miconazole (O) 7088 g 0,2 g 0,0738 A01AB12 Hexetidine (O) 1951200 ml A01AB81 Neomycin+ Benzocaine (dental) 30200 pieces A01AB82 Demeclocycline+ Triamcinolone (dental) 680 g A01AC Corticosteroids for local oral treatment A01AC81 Dexamethasone+ Thymol (dental) 3094 ml A01AD Other agents for local oral treatment A01AD80 Lidocaine+ Cetylpyridinium chloride (gingival) 227150 g A01AD81 Lidocaine+ Cetrimide (O) 30900 g A01AD82 Choline salicylate (O) 864720 pieces A01AD83 Lidocaine+ Chamomille extract (O) 370080 g A01AD90 Lidocaine+ Paraformaldehyde (dental) 405 g A02 DRUGS FOR ACID RELATED DISORDERS 47,1312 A02A ANTACIDS 1,0133 Combinations and complexes of aluminium, calcium and A02AD 1,0133 magnesium compounds A02AD81 Aluminium hydroxide+ Magnesium hydroxide (O) 811120 pieces 10 pieces 0,1689 A02AD81 Aluminium hydroxide+ Magnesium hydroxide (O) 3101974 ml 50 ml 0,1292 A02AD83 Calcium carbonate+ Magnesium carbonate (O) 3434232 pieces 10 pieces 0,7152 DRUGS FOR PEPTIC ULCER AND GASTRO- A02B 46,1179 OESOPHAGEAL REFLUX DISEASE (GORD) A02BA H2-receptor antagonists 2,3855 A02BA02 Ranitidine (O) 340327,5 g 0,3 g 2,3624 A02BA02 Ranitidine (P) 3318,25 g 0,3 g 0,0230 A02BC Proton pump inhibitors 43,7324 A02BC01 Omeprazole -

EUROPEAN PHARMACOPOEIA 10.0 Index 1. General Notices
EUROPEAN PHARMACOPOEIA 10.0 Index 1. General notices......................................................................... 3 2.2.66. Detection and measurement of radioactivity........... 119 2.1. Apparatus ............................................................................. 15 2.2.7. Optical rotation................................................................ 26 2.1.1. Droppers ........................................................................... 15 2.2.8. Viscosity ............................................................................ 27 2.1.2. Comparative table of porosity of sintered-glass filters.. 15 2.2.9. Capillary viscometer method ......................................... 27 2.1.3. Ultraviolet ray lamps for analytical purposes............... 15 2.3. Identification...................................................................... 129 2.1.4. Sieves ................................................................................. 16 2.3.1. Identification reactions of ions and functional 2.1.5. Tubes for comparative tests ............................................ 17 groups ...................................................................................... 129 2.1.6. Gas detector tubes............................................................ 17 2.3.2. Identification of fatty oils by thin-layer 2.2. Physical and physico-chemical methods.......................... 21 chromatography...................................................................... 132 2.2.1. Clarity and degree of opalescence of -

Structure and Properties of X-Ray Contrast Media
STRUCTURE AND PROPERTIES OF X-RAY CONTRAST MEDIA Optimal use of CM in radiology requires a knowl- edge of the nature and relevant properties of the available substances. This chapter describes the properties of currently used and newly developed contrast-giving agents that infuence their behav- ior in the human body, their side effects, and their practical utility. The main X-ray contrast agents in use today are insoluble barium sulfate for the diagnostic evalu- ation of the GI tract and water-soluble CM for the radiological assessment of the different vascular systems, body cavities and organs. In addition, a water-soluble CM based on tri-iodobenzene is the alternative agent of choice for oral use when bari- um sulfate is contraindicated. Barium Sulfate Barium is used in the form of the insoluble sulfate for radiography of the GI tract. If perforation is suspected, however, only water-soluble, iodinated agents (Gastrografn, Ultravist-370) can be used since the body is virtually incapable of eliminating barium sulfate once it has entered the peritoneum. Barium sulfate is available either as a powder to be prepared directly before use or as a ready-to-use suspension. For double-contrast examinations (fll- ing of the lumen with gas, coating of the wall with barium sulfate), barium sulfate is either mixed with a carbon dioxide additive, or a gas-forming agent is taken in addition. © The Author(s) 2018 20 U. Speck, X-Ray Contrast Media, https://doi.org/10.1007/978-3-662-56465-3_3 Common to all barium preparations is concentra- tion of barium sulfate which may diluted according to the needs of the examination. -

Estonian Statistics on Medicines 2013 1/44
Estonian Statistics on Medicines 2013 DDD/1000/ ATC code ATC group / INN (rout of admin.) Quantity sold Unit DDD Unit day A ALIMENTARY TRACT AND METABOLISM 146,8152 A01 STOMATOLOGICAL PREPARATIONS 0,0760 A01A STOMATOLOGICAL PREPARATIONS 0,0760 A01AB Antiinfectives and antiseptics for local oral treatment 0,0760 A01AB09 Miconazole(O) 7139,2 g 0,2 g 0,0760 A01AB12 Hexetidine(O) 1541120 ml A01AB81 Neomycin+Benzocaine(C) 23900 pieces A01AC Corticosteroids for local oral treatment A01AC81 Dexamethasone+Thymol(dental) 2639 ml A01AD Other agents for local oral treatment A01AD80 Lidocaine+Cetylpyridinium chloride(gingival) 179340 g A01AD81 Lidocaine+Cetrimide(O) 23565 g A01AD82 Choline salicylate(O) 824240 pieces A01AD83 Lidocaine+Chamomille extract(O) 317140 g A01AD86 Lidocaine+Eugenol(gingival) 1128 g A02 DRUGS FOR ACID RELATED DISORDERS 35,6598 A02A ANTACIDS 0,9596 Combinations and complexes of aluminium, calcium and A02AD 0,9596 magnesium compounds A02AD81 Aluminium hydroxide+Magnesium hydroxide(O) 591680 pieces 10 pieces 0,1261 A02AD81 Aluminium hydroxide+Magnesium hydroxide(O) 1998558 ml 50 ml 0,0852 A02AD82 Aluminium aminoacetate+Magnesium oxide(O) 463540 pieces 10 pieces 0,0988 A02AD83 Calcium carbonate+Magnesium carbonate(O) 3049560 pieces 10 pieces 0,6497 A02AF Antacids with antiflatulents Aluminium hydroxide+Magnesium A02AF80 1000790 ml hydroxide+Simeticone(O) DRUGS FOR PEPTIC ULCER AND GASTRO- A02B 34,7001 OESOPHAGEAL REFLUX DISEASE (GORD) A02BA H2-receptor antagonists 3,5364 A02BA02 Ranitidine(O) 494352,3 g 0,3 g 3,5106 A02BA02 Ranitidine(P) -

Immediate Reactions Following Iodinated Contrast Media Injection: a Study of 38 Cases
European Journal of Radiology 77 (2011) 495–501 Contents lists available at ScienceDirect European Journal of Radiology journal homepage: www.elsevier.com/locate/ejrad Immediate reactions following iodinated contrast media injection: A study of 38 cases Pascale Dewachter a,∗, Dominique Laroche b,1, Claudie Mouton-Faivre c,2, Evelyne Bloch-Morot d,3, Jean-Pierre Cercueil e,4, Liliane Metge f,5, Marie-France Carette g,6, Marie-Claude Vergnaud h,7, Olivier Clément i,8 a Service d’Anesthésie-Réanimation Chirurgicale & SAMU de Paris, Hôpital Necker-Enfants Malades, AP-HP, Université Paris-Descartes, 149 Rue de Sèvres, 75015 Paris, France b Service de Biophysique, Centre Hospitalier Universitaire, Avenue de la Côte de Nacre, Caen, France c Pôle d’Anesthésie-Réanimation Chirurgicale, Centre Hospitalier Universitaire-Hôpital Central, Avenue du Maréchal de Lattre de Tassigny, Nancy, France d Service de Médecine Interne, Hôpital Européen Georges Pompidou, 20 Rue Leblanc, Paris, France e Département d’Imagerie Medicale, Centre Hospitalier Universitaire, Hôpital du Bocage, 2, Boulevard du Maréchal de Lattre de Tassigny, Dijon, France f Département d’Imagerie Médicale, Centre Hospitalier Universitaire Caremeau, Place du Pr Robert Debré, Nîmes, France g Service de Radiologie, Hôpital Tenon, 4 Rue de la Chine, Paris, France h Service de Médecine Polyvalente, Centre Hospitalier Universitaire, Avenue de la Côte de Nacre, Caen, France i Service de Radiologie, Hôpital Européen Georges Pompidou, AP-HP, Université Paris Descartes, 20 Rue Leblanc, Paris, France article info abstract Article history: Objectives: To investigate the pathomechanisms involved in cases of immediate hypersensitivity reactions Received 2 August 2009 occurring after the administration of iodinated contrast media. -

FDA Listing of Established Pharmacologic Class Text Phrases January 2021
FDA Listing of Established Pharmacologic Class Text Phrases January 2021 FDA EPC Text Phrase PLR regulations require that the following statement is included in the Highlights Indications and Usage heading if a drug is a member of an EPC [see 21 CFR 201.57(a)(6)]: “(Drug) is a (FDA EPC Text Phrase) indicated for Active Moiety Name [indication(s)].” For each listed active moiety, the associated FDA EPC text phrase is included in this document. For more information about how FDA determines the EPC Text Phrase, see the 2009 "Determining EPC for Use in the Highlights" guidance and 2013 "Determining EPC for Use in the Highlights" MAPP 7400.13. -
OMNIPAQUE™ (Iohexol) Injection
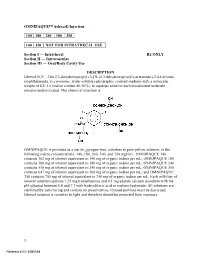
OMNIPAQUE™ (iohexol) Injection 140 180 240 300 350 140 350 NOT FOR INTRATHECAL USE Section I — Intrathecal Rx ONLY Section II — Intravascular Section III — Oral/Body Cavity Use DESCRIPTION Iohexol,N,N´ - Bis(2,3-dihydroxypropyl)-5-[N-(2,3-dihydroxypropyl)-acetamido]-2,4,6-triiodo- isophthalamide, is a nonionic, water-soluble radiographic contrast medium with a molecular weight of 821.14 (iodine content 46.36%). In aqueous solution each triiodinated molecule remains undissociated. The chemical structure is: OMNIPAQUE is provided as a sterile, pyrogen-free, colorless to pale-yellow solution, in the following iodine concentrations: 140, 180, 240, 300, and 350 mgI/mL. OMNIPAQUE 140 contains 302 mg of iohexol equivalent to 140 mg of organic iodine per mL; OMNIPAQUE 180 contains 388 mg of iohexol equivalent to 180 mg of organic iodine per mL; OMNIPAQUE 240 contains 518 mg of iohexol equivalent to 240 mg of organic iodine per mL; OMNIPAQUE 300 contains 647 mg of iohexol equivalent to 300 mg of organic iodine per mL; and OMNIPAQUE 350 contains 755 mg of iohexol equivalent to 350 mg of organic iodine per mL. Each milliliter of iohexol solution contains 1.21 mg tromethamine and 0.1 mg edetate calcium disodium with the pH adjusted between 6.8 and 7.7 with hydrochloric acid or sodium hydroxide. All solutions are sterilized by autoclaving and contain no preservatives. Unused portions must be discarded. Iohexol solution is sensitive to light and therefore should be protected from exposure. 1 Reference ID: 4080358 The available concentrations have the following physical properties: Absolute Concentration Osmolality* Osmolarity Viscosity Specific (mgI/mL) (mOsm/kg water) (mOsm/L) (cp) Gravity 20°C 37°C 37°C 140 322 273 2.3 1.5 1.164 180 408 331 3.1 2.0 1.209 240 520 391 5.8 3.4 1.280 300 672 465 11.8 6.3 1.349 350 844 541 20.4 10.4 1.406 * By vapor-pressure osmometry. -

Appendix B - Product Name Sorted by Applicant
JUNE 2021 - APPROVED DRUG PRODUCT LIST B - 1 APPENDIX B - PRODUCT NAME SORTED BY APPLICANT ** 3 ** 3D IMAGING DRUG * 3D IMAGING DRUG DESIGN AND DEVELOPMENT LLC AMMONIA N 13, AMMONIA N-13 FLUDEOXYGLUCOSE F18, FLUDEOXYGLUCOSE F-18 SODIUM FLUORIDE F-18, SODIUM FLUORIDE F-18 3M * 3M CO PERIDEX, CHLORHEXIDINE GLUCONATE * 3M HEALTH CARE INC AVAGARD, ALCOHOL (OTC) DURAPREP, IODINE POVACRYLEX (OTC) 3M HEALTH CARE * 3M HEALTH CARE INFECTION PREVENTION DIV SOLUPREP, CHLORHEXIDINE GLUCONATE (OTC) ** 6 ** 60 DEGREES PHARMS * 60 DEGREES PHARMACEUTICALS LLC ARAKODA, TAFENOQUINE SUCCINATE ** A ** AAA USA INC * ADVANCED ACCELERATOR APPLICATIONS USA INC LUTATHERA, LUTETIUM DOTATATE LU-177 NETSPOT, GALLIUM DOTATATE GA-68 AAIPHARMA LLC * AAIPHARMA LLC AZASAN, AZATHIOPRINE ABBVIE * ABBVIE INC ANDROGEL, TESTOSTERONE CYCLOSPORINE, CYCLOSPORINE DEPAKOTE ER, DIVALPROEX SODIUM DEPAKOTE, DIVALPROEX SODIUM GENGRAF, CYCLOSPORINE K-TAB, POTASSIUM CHLORIDE KALETRA, LOPINAVIR NIASPAN, NIACIN NIMBEX PRESERVATIVE FREE, CISATRACURIUM BESYLATE NIMBEX, CISATRACURIUM BESYLATE NORVIR, RITONAVIR SYNTHROID, LEVOTHYROXINE SODIUM ** TARKA, TRANDOLAPRIL TRICOR, FENOFIBRATE TRILIPIX, CHOLINE FENOFIBRATE ULTANE, SEVOFLURANE ZEMPLAR, PARICALCITOL ABBVIE ENDOCRINE * ABBVIE ENDOCRINE INC LUPANETA PACK, LEUPROLIDE ACETATE ABBVIE ENDOCRINE INC * ABBVIE ENDOCRINE INC LUPRON DEPOT, LEUPROLIDE ACETATE LUPRON DEPOT-PED KIT, LEUPROLIDE ACETATE ABBVIE INC * ABBVIE INC DUOPA, CARBIDOPA MAVYRET, GLECAPREVIR NORVIR, RITONAVIR ORIAHNN (COPACKAGED), ELAGOLIX SODIUM,ESTRADIOL,NORETHINDRONE ACETATE -

Investigating the Environmental Fate of Iodinated X-Ray Contrast
Investigating the Environmental Fate of Iodinated X-ray Contrast Media in the Urban Water Cycle: Identification, Characterization, and Occurrence of Biotransformation Products Dissertation Zur Erlangung des akademischen Grades eines Doktors der Naturwissenschaft Fachbereich 3: Mathematik/Naturwissenschaften Universität Koblenz-Landau Vorgelegt am 28.05.2010 von Jennifer Lynne Kormos, M.Sc. geb. am. 13.11.1979 in St. John’s, Canada Referent: PD Dr. Thomas A. Ternes Koreferent: Prof. Dr. Joachim Scholz 2 Acknowledgments This thesis is the result of a collaborative effort from many people! First of all I would like to thank the Marie Curie Research Training Network KEYBIOEFFECTS for funding this research and more importantly providing opportunities for me to network with other graduate students and research scientists in a number of scientific disciplines within Europe and internationally. I would like to thank and acknowledge Dr. Thomas Ternes, my supervisor, or as they say in German my “Doktor Vater,” for giving me the opportunity to complete my PhD in his research group at the Federal Institute of Hydrology (Bundesanstalt für Gewässerkunde, BfG). It was an honour for me to work with an internationally-known researcher investigating the occurrence and fate of emerging organic micropollutants. His dedication, guidance, support, enthusiasm and extensive knowledge are just a few of his qualities that helped me to strive in completing my PhD degree. I would like to thank Prof. Dr. Joachim Scholz for agreeing to be one of the evaluators of my PhD thesis and the University of Koblenz-Landau for allowing me to defend my dissertation in the Department of Chemistry. -

Iotrolan (BAN, USAN, Rinn) Description
1486 Contrast Media Iotrolan (BAN, USAN, rINN) Description. Meglumine iotroxate contains about 47.4% of I. Ioxaglic Acid (BAN, USAN, rINN) Iotrol; Iotrolán; Iotrolane; Iotrolanum; Iotrolum; Jotrolaani; Jotro- Adverse Effects, Treatment, and Precautions Acide ioxaglique; Ácido_ ioxáglico; Acidum ioxaglicum; Joksagliini- lan; ZK-39482. N,N′,N′′,N′′′-Tetrakis(2,3-dihydroxy-1-hydroxy- See under the amidotrizoates, p.1475. happo; Joksagliko rugštis; Joxaglinsav; Joxaglinsyra; Kyselina joxa- methylpropyl)-2,2′,4,4′,6,6′-hexaiodo-5,5′-(N,N′-dimethylmalo- glová; P-286. N-(2-Hydroxyethyl)-2,4,6-tri-iodo-5-[2′,4′,6′-tri- nyldi-imino)di-isophthalamide. Pharmacokinetics iodo-3′-(N-methylacetamido)-5′-methylcarbamoylhippuramido]- After intravenous injection, iotroxic acid binds to plasma pro- isophthalamic acid. Йотролан teins and is taken up by the liver; plasma-protein binding is about Йоксагловая Кислота C37H48I6N6O18 = 1626.2. 60 to 90%. It is excreted primarily unchanged in the bile; a small CAS — 79770-24-4. amount is metabolised and excreted in the urine. C24H21I6N5O8 = 1268.9. ATC — V08AB06. CAS — 59017-64-0. ATC Vet — QV08AB06. Uses and Administration ATC — V08AB03. Iotroxic acid is an ionic dimeric iodinated radiographic contrast ATC Vet — QV08AB03. medium (see p.1474); it is taken up by the liver and excreted in OH OH bile, and is used in cholecystography and cholangiography. IO OH OH OH Iotroxic acid is given intravenously as a solution containing HO 10.5% of the meglumine salt. The usual dose is 10.5 g of meglu- HO N O HN OH HN mine iotroxate (equivalent to about 5 g of iodine), given by infu- H I O I O sion over at least 15 minutes.