Advancing Health
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Maryland Hospitals by County 2014
Maryland Hospital Association 2014 Member Hospitals by County 57 6 Allegany 43 Garrett 31 Cecil Washington Carroll 36 8 Harford Baltimore 54 46 12 Frederick 11 1340 34 53 23 Baltimore Kent Howard City 50 16 Montgomery 26 44 1 2 20 Queen 39 Anne Anne's 33 15 9 Arundel 3 42 56 32 24 37 Caroline 21 41 Prince George's Talbot 52 10 27 29 49 Calvert Baltimore City Charles 7 51 48 45 19 Dorchester 30 18 5 55 17 Wicomico 47 14 4 38 St. Mary's 28 35 25 Worcester Somerset Hospital Name Number Hospital Name Number Hospital Name Number 22 Adventist Behavioral Health 1 Levindale Hebrew Geriatric Center & Hospital 21 Sinai Hospital of Baltimore 41 Adventist Rehabilitation Hospital of Maryland 2 McCready Foundation 22 Suburban Hospital 42 Anne Arundel Medical Center 3 MedStar Franklin Square Medical Center 23 Union Hospital 43 Atlantic General Hospital 4 MedStar Good Samaritan Hospital 24 Univ of MD Baltimore Washington Medical Ctr 44 Bon Secours Baltimore Health System 5 MedStar Harbor Hospital 25 Univ of MD Charles Regional Medical Center 45 Univ of MD Harford Memorial Hospital 46 Brook Lane 6 MedStar Montgomery Medical Center 26 Calvert Memorial Hospital 7 MedStar Southern Maryland Hospital Center 27 University of Maryland Medical Center 47 Univ of MD Medical Center Midtown Campus 48 Carroll Hospital Center 8 MedStar St. Mary’s Hospital 28 Doctors Community Hospital 9 MedStar Union Memorial Hospital 29 Univ of MD Rehabilitation & Orthopaedic Inst 49 Fort Washington Center Medical Center 10 Mercy Medical Center 30 Univ of MD Shore Medical Ctr at Chestertown 5050 Frederick Regional Health System 11 Meritus Medical Center 31 Univ of MD Shore Medical Ctr at Dorchester 51 Garrett County Memorial Hospital 12 Mt. -

Sustaining Partners Program
SUSTAINING PARTNERS PROGRAM Philanthropic Investment Agreement Please complete all sections of the agreement and return it with your contribution. Organization name: Contact name: Title: Mailing address: Phone: (W) (C) Email: For recognition purposes, please indicate exactly how you would like your name to appear: Check here if you would prefer to remain anonymous. Please choose your level of support. Sustaining Partnership $7,500 contribution $2,500 contribution $5,000 contribution $1,000 contribution Please designate your gift commitment: $___________ MedStar Health: Area of greatest need $___________ MedStar National Rehabilitation Hospital $___________ MedStar Franklin Square Medical Center $___________ MedStar Patient Safety Institute $___________ MedStar Georgetown University Hospital $___________ MedStar Southern Maryland Hospital Center $___________ MedStar Good Samaritan Hospital $___________ MedStar St. Mary’s Hospital $___________ MedStar Harbor Hospital $___________ MedStar Union Memorial Hospital $___________ MedStar Health Research Institute $___________ MedStar Visiting Nurse Association $___________ MedStar Institute for Innovation $___________ MedStar Washington Hospital Center $___________ MedStar Montgomery Medical Center (continued on next page) Philanthropic Investment Agreement Our organization will fulfill this corporate partnership commitment as follows: CHECK: Please make checks payable to: MedStar Health (Note the Sustaining Partners Program) CREDIT CARD: * Visa * MasterCard * American Express * Discover *You may also give securely online at MedStarHealth.org/SustainingPartners. Name on the card: Credit card #: Expiration Date: / For a contribution of $ CID#: Address of card holder, including ZIP code: INVOICE: Invoice instructions: Thank you for your partnership with MedStar Health. We will provide a receipt for tax purposes after an annual contribution payment has been made. Signature Date Signature – MedStar Philanthropy Date We will provide you with a copy of the signed Philanthropic Investment Agreement. -

Consent and Release Form Reviewed By: Date: Medstar Health Appreciates the Confidence You Have Shown in Choosing Us to Provide for Your Rehabilitative Needs
Patient Name: DOB: EMPI/MRN: Consent and Release Form Reviewed by: Date: MedStar Health appreciates the confidence you have shown in choosing us to provide for your rehabilitative needs. The service you have elected to participate in implies a financial responsibility on your part. This responsibility obligates you to ensure payment in full of your fees. As a courtesy, we will verify your coverage and bill your insurance carrier on your behalf. However, you are ultimately responsible for the payment of your bill. Primary Insurance: Coverage: % Remaining Out of Pocket: $ # of Visits Remaining: Due at Time of Visit: Copay: $ Co-ins % Remaining Deductible: $ ($100/visit until met) Secondary Insurance: Comments: Note: This is an online or telephonic quote of patient benefits and is not a guarantee. For any questions regarding this quote, the patient or patient's guardian are advised to contact and verify benefit coverage with his/her carrier . □ Financial Agreement/Guarantee of Payment and Assignment of Benefits You are responsible for payment of any co-payment at the time of service and for any deductible/coinsurance as determined by your contract with your insurance carrier. Many insurance companies have additional stipulations that may affect your coverage. You are responsible for any amount not covered by your insurer. If your insurance carrier denies any part of your claim, or if you and your physician elect to continue therapy past your approved period, you will be responsible for your account balance in full. For your convenience, we accept cash, checks and most major credit cards. Payment is expected by payment due date on your Monthly Patient Statement. -
Exceeding Expectations
WINTER 2018 Exceeding Expectations MedStar Harbor Women’s Care Goes Above and Beyond GETTING TO KNOW Stuart M. Levine, MD, FACP MedStar Harbor Hospital’s New President and Chief Medical Officer Constantly Stressed Out? A Behavioral Health Specialist Can Make all the Difference HEALTHY HABITS Keeping Your Brain Healthy as You Age [CONTENTS] [WHAT’S new] WINTER 2018 Specialized Congratulations to Our FEATURES Getting to Know Vascular Care Baltimore Magazine Top Doctors! 4 Stuart M. Levine, MD, FACP Now More Accessible altimore magazine recently published its Top Doctors issue for MedStar Harbor Hospital’s New 2017. The physicians honored with this title were chosen by ndividuals in need of specialized vascular services President and Chief Medical Officer their peers, who responded to survey questions, such as: What now have easy access to the care they need at B physician would you send your own family member to? Exceeding Expectations MedStar Harbor Hospital with the opening of MedStar Harbor Women’s Care I 8 a dedicated clinic for MedStar Heart & Vascular Goes Above and Beyond MedStar Harbor Hospital is proud to announce that five of our physicians Institute’s vascular surgery program. were recognized as Top Doctors in six specialty areas by the magazine. Constantly Stressed Out? They are: 12 A Behavioral Health Specialist The clinic is staffed by Avinash Ganti, MD, and Suzanne Can Make all the Difference Kool, MD, fellowship-trained vascular surgeons who Fouad Abbas, MD – Gynecologic Surgery, Gynecologic Oncology specialize in the diagnosis and treatment of arterial and Leigh Ann Curl, MD – Orthopaedic Surgery/Sports Medicine Kristen Fernandez, MD – Breast Surgery What You Should Know venous disease. -

Medstar Health Is Working Diligently to Care for the Patients and Communities We Serve Who May Need Us During This Challenging Time of the COVID‐19 Pandemic
MedStar Health is working diligently to care for the patients and communities we serve who may need us during this challenging time of the COVID‐19 pandemic. Our leaders, caregivers and non‐clinical personnel are focused on ensuring the safety and well‐being of our communities. We have workflows and procedures in place that address triage, screening, testing and treatment, and we are planning for an exponential increase in demand for our services in the event that becomes necessary. We are addressing the needs of our communities through various channels. We have launched chat bots to address COVID‐related questions individuals may have. This appears to have a positive outcome in reducing the number of unnecessary provider visits during a time of needed social‐distancing. MedStar has greatly increased our capability to provide E‐visits, with over 200 providers available to provide visits upon demand. E‐visit is a critical path for screening patients for COVID‐19 testing needs. MedStar continues to follow the CDC/regulatory screening criteria to identify which patients are appropriate for COVID‐19 testing. The URL for MedStar e‐visit is https://www.medstarhealth.org/medstar-health-evisit. As of March 31, MedStar has more than thirty different testing sites for COVID‐19 as outlined below. Our MedStar Medical Group sites and MedStar urgent care sites, as well as our Hospital EDs and some newly launched tents are all locations where testing is taking place. MedStar Health COVID-19 Testing Sites (ERs, Medical Group, Urgent Care) MedStar Hospital ER Testing Sites MedStar Franklin Square Medical Center - 9000 Franklin Square Dr. -
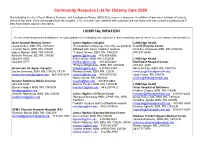
Community Resource List for Ostomy Care 2020
Community Resource List for Ostomy Care 2020 The following is a list of local Wound, Ostomy, and Continence Nurses (WOCN) to use as a resource. In addition, there are a number of ostomy clinics in the area. Once discharged from the hospital, LTC, or home care, patients with ostomies are not alone and can contact a professional if they have future ostomy care needs. HOSPITAL INPATIENT *Denotes that this particular facility/nurse accepts outpatient referrals/physician orders for treatment and your patient can be seen for ostomy related problems. Anne Arundel Medical Center Johns Hopkins Hospital LifeBridge Health Joyce Onken, BSN, RN, CWOCN (For outpatient follow-up, may only see patients Carroll Hospital Center Jennifer Davis, BSN, RN, CWON affiliated with Johns Hopkins Hospital) Christine Arrowood, BSN, RN, CWOCN Agnes Mpanja, BSN, RN, CWCN *Jessica Groom, BSN, RN, CWOCN 410-871-6839 Michelle Perkins, BS, RN, CWON [email protected] 410-955-6668 443-481-5508 Kelly Heffron, BSN, RN, CWOCN LifeBridge Health 443-481-5177 [email protected] 410-955-6647 Northwest Hospital Center *Frances Magliacane, BSN, RN, CWOCN 410-521-2200 Ascension St. Agnes Hospital [email protected] 410-955-5367 Missy McCoy, MSN, RN, CWOCN Sacha Simmons, BSN, RN, CWON, CFCN Rhonda Sewell, BSN, RN, COCN [email protected] [email protected] 667-234-3034 [email protected] 443-287-0392 Judy Coster, RN, CWCN Nancy Sujeta, RN, CWOCN [email protected] Greater Baltimore Medical Center [email protected] 410-955-6667 443-849-6992 Melissa Venker, BSN, -

At a Glance Medstar Health Facts Who We
At a Glance Who We Are MedStar Health combines the best aspects of academic medicine, Hospitals research, and innovation with a complete spectrum of clinical services to MedStar Franklin Square Medical Center advance patient care. As the largest healthcare provider in Maryland and MedStar Georgetown University Hospital the Washington, D.C., region, MedStar Health’s 10 hospitals, MedStar MedStar Good Samaritan Hospital MedStar Harbor Hospital Health Research Institute, and a comprehensive scope of health-related MedStar Montgomery Medical Center organizations are recognized regionally and nationally for excellence MedStar National Rehabilitation Hospital in medical care. MedStar Health has one of the largest graduate medical MedStar Southern Maryland Hospital Center education programs in the country, training 1,100 medical residents annually, MedStar St. Mary’s Hospital MedStar Union Memorial Hospital and is the medical education and clinical partner of Georgetown University. MedStar Washington Hospital Center MedStar Health is a $5.6 billion, not-for-profit, regional healthcare system based in Columbia, Maryland, and one of the largest employers in the region. Clinical Research and Innovation Our more than 30,000 associates and 4,700 affiliated physicians support MedStar Health Research Institute MedStar Health’s patient-first philosophy that combines care, compassion, MedStar Institute for Innovation and clinical excellence with an emphasis on customer service. Home Health Care MedStar Health Infusion MedStar Health Facts MedStar Visiting -

Participation in Medstar Select Providers Wishing to Participate with Medstar Select Are Required to Submit the Following Credentialing Information
Participation in MedStar Select Providers wishing to participate with MedStar Select are required to submit the following credentialing information: Provider application Maryland Uniform Credentialing Form or Council for Affordable Quality Healthcare (CAQH) Application Copy of unrestricted DEA registration certificate, if applicable Copy of unrestricted Controlled Dangerous Substance registration issued by the State or District in which you practice, if applicable Copy of current professional license(s) Copy of ECFMG certificate, if applicable Copy of all certification, with certification number, for Allied Healthcare Professionals, if applicable Copy of professional liability coverage certification, including limits of coverage, expiration date, and name of the provider covered under the policy; shared limits coverage is not acceptable Any other certificates held Nurse Practitioner, Nurse Midwife or Physician Assistant agreements with their collaborating physicians or their agreement with the State, whichever is applicable. W-9 or CP-575 (if submitting a W-9 please indicate the legal billing entity in line one) Organizational NPI Number (Type II) Providers must have current and unrestricted privileges at one of the MedStar Select participating hospitals: MedStar Franklin Square Medical Center, MedStar Good Samaritan Hospital, MedStar Harbor Hospital, MedStar Montgomery Medical Center, MedStar St. Mary’s Hospital, MedStar Southern Maryland Hospital, MedStar Union Memorial Hospital, MedStar Georgetown University Hospital, MedStar National Rehabilitation Network, MedStar Washington Hospital Center Providers who apply to MedStar Select have the right, upon request, to review their credentialing application, correct inaccurate information and obtain the status of their application during the credentialing process. Requests can be made by calling 800-905-1722 (MD Providers) and 855-210-6203 (DC Providers). -

When Delivery Time Comes Stuart M
2017 FALL When Delivery Time Comes Ensuring Moms-to-Be Get the Care They Need Novel Treatments for Complex Conditions Patients With Advanced Liver Cancer Among Those Benefitting Keeping Athletes in the Game Athletic Trainers Play a Key Role in Preventing and Managing Injuries [CONTENTS] FALL 2017 INTRODUCING OUR NEW PRESIDENT AND CHIEF MEDICAL OFFICER FEATURES Stuart M. Levine, MD, FACP, was recently named president and Novel Treatments for chief medical officer of MedStar 4 Complex Conditions Harbor Hospital and a senior vice Patients With Advanced Liver Cancer president of MedStar Health. He succeeds Dennis W. Pullin, Among Those Benefitting FACHE, the former president, who left MedStar Harbor after When Delivery Time Comes Stuart M. Levine, eight years of strong leadership. 8 Ensuring Moms-to-Be Get the MD, FACP Care They Need “My excitement at being appointed to this new role is beyond words,” says Dr. Levine. “What a privilege Keeping Athletes in the Game and responsibility it is to lead a phenomenal 10 Athletic Trainers Play a Key Role in organization committed to being on the forefront Preventing and Managing Injuries of healthcare delivery. I am overjoyed to continue working with all of the talented and dedicated Seasonal Depression individuals who make MedStar Harbor the vibrant 14 It’s Not Just in Your Head ... place that it is today. Together, we are one big Treatment Can Help family collectively focused on providing the highest quality and safest care possible. I am grateful for this opportunity to help write the next chapter of MedStar Harbor’s history as we move full steam DEPARTMENTS ahead on our journey of continued success.” 3 WHAT’S NEW Most recently, Dr. -

Promoting Community Health Through Direct Engagement
PROMOTING COMMUNITY HEALTH THROUGH DIRECT ENGAGEMENT How a MedStar Health ‘Task Force’ Rallies Local Stakeholders to Improve Health in Baltimore CONTRIBUTOR Contributor: Ryan Moran, Director of Community Health, MedStar Health NATIONAL TRENDS, MARYLAND INNOVATION Policies that change what we pay for in healthcare — a shift from service volume to improved health outcomes — offer clear incentives for health systems to more effectively manage the overall health of the populations they serve. In many cases, this provides an opportunity for hospitals and clinics to address the root causes of poor health — such as housing insecurity, substance abuse or lack of access to greenspace. While most health systems embrace this proactive approach, identifying the true health needs of a community and addressing those through cost-effective interventions can be daunting. Maryland’s Total Cost of Care model, launched in 2014, provides hospitals in Maryland with a global, population-based payment ABOUT MEDSTAR HEALTH to cover all hospital services provided within a contract year. Performance-based incentive payments are also provided to non- MedStar Health is a not-for-profit health system hospital healthcare and primary care providers to improve the serving people in Maryland, Virginia, and Washington, provision of care across the care continuum to support population DC. An anchor institution with over 30,000 health improvements. These significant changes push hospitals to associates, more than 5,400 affiliated physicians manage healthcare spending by providing the right care in the right across 10 hospitals and numerous ambulatory care setting with necessary supports — and have encouraged hospitals practices and urgent care facilities, MedStar is the to invest in community-based strategies to address the social largest provider of healthcare services in the region. -

Women's Health
WaterfrontA publication from MAREDST HARBOR Hospital FALL 2015 MedStarHarbor.org/Waterfront NEW MOM GETS EXTRA SPECIAL DELIVERY ON HER BIRTHDAY HEART ATTACK SYMPTOMS— WHAT WOMEN NEED TO KNOW Special Issue: Women’s Health Knowledge and Compassion Waterfront MEDSTAR Focused HARBOR HOSPITAL on Fall You 2015 1 LETTER FROM THE PRESIDENT contents A WOMAN taKES ON numerous roles throughout her lifetime, and it is essential that she stay healthy to flourish throughout each new season of life. In this issue of Waterfront, we’re focusing on the individuals who make up more than half of our patient population—women. From routine checkups with primary care providers, to labor and delivery, cardiology, emergency care, and orthopaedic surgery, MedStar Health Topics Harbor Hospital is dedicated to offering you the very best care as your health needs evolve. 3 It’s Important to Take Care We provide our female patient population with of Yourself every possible treatment option available in 6 New Baby Makes Mom’s health care today—no matter if she is delivering a baby, having a routine checkup or undergoing Birthday Special minimally invasive gynecologic surgery—and we are 8 Heart Attack Symptoms committed to constantly enhancing the quality of 10 Restoring Bodies and Spirits care we offer. 11 Free Cancer Screenings Exemplifying this commitment, our Women and 12 Building Healthier Infants’ Center, which provides a family-centered childbirth experience that includes labor, delivery, Communities—Community recovery, and postpartum services, recently was Lectures and Class Schedule honored by the March of Dimes, in partnership with the Maryland State Department of Health and 14 News from Around MedStar Health Mental Hygiene and the Maryland Patient Safety Center, for addressing the most urgent infant health problem in the U.S.—premature birth. -

Schedule of Classes & Events Fall 2012
Health Education Classes & Events Winter – Spring 2016 Healthy Families – Healthcare Alliance Childbirth and Parenting Baby Basics w/Infant CPR and Child Passenger Safety – MedStar Washington Hospital Center Parents will learn how to care for their precious newborn by our registered nurse educator. Infant CPR is always taught by instructors that are certified by the American Heart Association. Child Passenger Safety is must. Statistics show that most babies are placed in car seats that have not been properly installed. A certified trainer will review the important points every parent should know about how to keep their infant safe. Date & Time Please call for class schedules Location MedStar Washington Hospital Center - Parent Services 110 Irving St., NW, Room 5B-31 Washington, DC 20010 Registration Early registration is encouraged. Class size is limited to ensure optimum interaction with instructors. To register, call (202) 877-6161. Baby Basics at MedStar Washington This class is designed to help parents provide basic baby care. Class topics include bathing and grooming, diapering, bottle preparation, methods for consoling a crying baby, medical emergencies, methods for checking your baby’s temperature, infant passenger seat safety and infant CPR. Date & Time Fourth Sunday of the Month, 10:00 a.m. – 12 p.m. Please call to confirm class schedules Location MedStar Washington Hospital Center - Parent Services 110 Irving St., NW Washington, DC 20010 Registration Early registration is encouraged. Class size is limited to ensure optimum interaction with instructors. To register, call (202) 877-6161. Baby Care and Infant CPR Class – 1 Day – MedStar Georgetown University Hospital Learn about newborn care, growth and development, adaptations and hands on doll practice.