T2 Ankle Arthrodesis Nail
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Federal Register/Vol. 83, No. 150/Friday, August 3, 2018/Notices
Federal Register / Vol. 83, No. 150 / Friday, August 3, 2018 / Notices 38161 Community Community map repository address Canadian County, Oklahoma and Incorporated Areas Project: 12–06–1030S Preliminary Date: February 8, 2018 City of El Reno ......................................................................................... Municipal Building, 101 North Choctaw Avenue, El Reno, OK 73036. Aransas County, Texas and Incorporated Areas Project: 15–06–0811S Preliminary Date: March 16, 2018 City of Aransas Pass ................................................................................ City Hall, 600 West Cleveland Boulevard, Aransas Pass, TX 78336. San Patricio County, Texas and Incorporated Areas Project: 15–06–0811S Preliminary Date: March 16, 2018 City of Aransas Pass ................................................................................ City Hall, 600 West Cleveland Boulevard, Aransas Pass, TX 78336. [FR Doc. 2018–16666 Filed 8–2–18; 8:45 am] 97.048, Disaster Housing Assistance to Brown Fund; 97.032, Crisis Counseling; BILLING CODE 9110–12–P Individuals and Households In Presidentially 97.033, Disaster Legal Services; 97.034, Declared Disaster Areas; 97.049, Disaster Unemployment Assistance (DUA); Presidentially Declared Disaster Assistance— 97.046, Fire Management Assistance Grant; DEPARTMENT OF HOMELAND Disaster Housing Operations for Individuals 97.048, Disaster Housing Assistance to and Households; 97.050, Presidentially Individuals and Households In Presidentially SECURITY Declared Disaster Assistance to Individuals -
Mechanical Keyswitch B3F
Mechanical Keyswitch B3F Miniature, Space-Saving Keyswitch Provides Long Service Life and Easy Mounting ■ Extended mechanical/electrical service life: 10 x 106 operations for 12 x 12 mm type and 1 x 106 operations for the 6 x 6 mm type ■ Ideal for applications such as audio, office and communications equipment, measuring instruments, TVs, VCRs, etc. ■ Taped radial type, vertical type, high force type, and gold-plated contact type are available as series versions ■ Flux-tight base structure allows automatic soldering of the keyswitches onto a PC board Ordering Information Flat Projected ■ B3F-1■■■, B3F-3■■■ 6 x 6 mm type Part Number Switch Without ground terminal With ground terminal Type Plunger height x pitch Operating Force Bags Sticks* Bags Sticks* Standard Flat 4.3 x 6.5 mm General-purpose: 100 g B3F-1000 B3F-1000S B3F-1100 B3F-1100S 150 g B3F-1002 B3F-1002S B3F-1102 B3F-1102S High-force: 260 g B3F-1005 B3F-1005S B3F-1105 B3F-1105S 5.0 x 6.5 mm General-purpose: 100 g B3F-1020 B3F-1020S B3F-1120 B3F-1120S 150 g B3F-1022 B3F-1022S B3F-1122 B3F-1122S High-force: 260 g B3F-1025 B3F-1025S B3F-1125 B3F-1125S 5.0 x 7.5 mm General-purpose: 100 g — — B3F-1110 — Projected 7.3 x 6.5 mm General-purpose: 100 g B3F-1050 B3F-1050S B3F-1150 B3F-1150S 150 g B3F-1052 B3F-1052S B3F-1152 B3F-1152S High-force: 260 g B3F-1055 B3F-1055S B3F-1155 B3F-1155S Vertical Flat 3.15 mm General-purpose: 100 g — — B3F-3100 — 150 g — — B3F-3102 — High-force: 260 g — — B3F-3105 — 3.85 mm General-purpose: 100 g — — B3F-3120 — 150 g — — B3F-3122 — High-force: 260 g — — B3F-3125 — Projected 6.15 mm General-purpose: 100 g — — B3F-3150 — 150 g — — B3F-3152 — High-force: 260 g — — B3F-3155 — * Number of switches per stick: Without ground terminal ... -
Herefore, Incentives Typically Offered and Used for Development Would Be Replaced with the EB-5 Investment
Revised – 9/18/17 CITY OF YPSILANTI REGULAR COUNCIL MEETING CITY COUNCIL CHAMBERS – ONE SOUTH HURON ST. YPSILANTI, MI 48197 TUESDAY, SEPTEMBER 19, 2017 7:00 p.m. I. CALL TO ORDER – II. ROLL CALL – Council Member Bashert P A Council Member Robb P A Mayor Pro-Tem Brown P A Council Member Vogt P A Council Member Murdock P A Mayor Edmonds P A Council Member Richardson P A III. INVOCATION – IV. PLEDGE OF ALLEGIANCE – “I pledge allegiance to the flag, of the United States of America, and to the Republic for which it stands, one nation, under God, indivisible, with liberty and justice for all.” V. AGENDA APPROVAL – VI. INTRODUCTIONS – VII. AUDIENCE PARTICIPATION – VIII. REMARKS BY THE MAYOR – IX. PUBLIC HEARING – International Village - Water Street A. Resolution No. 2017-208, approving purchase agreement. B. Open public hearing C. Resolution No. 2017-209, close public hearing X. PRESENTATIONS – Discussion of Easement Agreement with Michigan Advocacy Program on 15 N. Washington. XI. ORDINANCES – FIRST READING – Ordinance No. 1294 An ordinance to rezone 75 Catherine from Core Neighborhood to Production, Manufacturing & Distribution. A. Resolution No. 2017-210, determination B. Open public hearing C. Resolution No. 2017-211, close public hearing 1 XII. CONSENT AGENDA – Resolution No. 2017-212 1. Resolution No. 2017–213, approving minutes of August 22 and September 5, 2017. 2. Resolution No. 2017-214, approving the issuance of a blanket permit for window signs of any size for the month of October for businesses that participate with the Eastern Michigan University’s “Follow the Green & White Road” homecoming spirit project. -
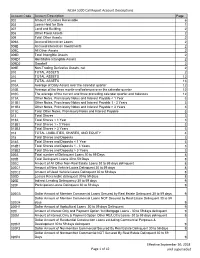
NCUA 5300 Call Report Account Descriptions Page 1 of 42 Effective
NCUA 5300 Call Report Account Descriptions Account Code Account Description Page 002 Amount of Leases Receivable 6 003 Loans Held for Sale 1 007 Land and Building 2 008 Other Fixed Assets 2 009 Total Other Assets 2 009A Accrued Interest on Loans 2 009B Accrued Interest on Investments 2 009C All Other Assets 2 009D Total Intangible Assets 2 009D1 Identifiable Intangible Assets 2 009D2 Goodwill 2 009E Non-Trading Derivative Assets, net 2 010 TOTAL ASSETS 2 010 TOTAL ASSETS 12 010 TOTAL ASSETS 13 010A Average of Daily Assets over the calendar quarter 12 010B Average of the three month-end balances over the calendar quarter 12 010C The average of the current and three preceding calendar quarter-end balances 12 011A Other Notes, Promissory Notes and Interest Payable < 1 Year 3 011B1 Other Notes, Promissory Notes and Interest Payable 1 - 3 Years 3 011B2 Other Notes, Promissory Notes and Interest Payable > 3 Years 3 011C Total Other Notes, Promissory Notes and Interest Payable 3 013 Total Shares 3 013A Total Shares < 1 Year 3 013B1 Total Shares 1 - 3 Years 3 013B2 Total Shares > 3 Years 3 014 TOTAL LIABILITIES, SHARES, AND EQUITY 4 018 Total Shares and Deposits 3 018A Total Shares and Deposits < 1 Year 3 018B1 Total Shares and Deposits 1 - 3 Years 3 018B2 Total Shares and Deposits > 3 Years 3 020A Total number of Delinquent Loans 30 to 59 Days 8 020B Total Delinquent Loans 30 to 59 Days 8 020C Amount of All Other Non-Real Estate Loans 30 to 59 days delinquent 8 020C1 Amount of New Vehicle Loans Delinquent 30 to 59 days 8 020C2 Amount of Used -
T2 R1.5 Femoral Nailing System
T2 R1.5 Femoral Nailing System Operative Technique Femoral Nailing System Contributing Surgeons Prof. Dr. med. Volker Bühren Chief of Surgical Services Medical Director of Murnau Trauma Center Murnau Germany Joseph D. DiCicco III, D. O. Director Orthopaedic Trauma Service Good Samaritan Hospital Dayton, Ohio Associate Clinical Professor of Orthopeadic Surgery Ohio University and Wright State University USA Thomas G. DiPasquale, D. O. Medical Director, Orthopedic Trauma Services Director, Orthopedic Trauma Fellowship and This publication sets forth detailed Orthopedic Residency Programs recommended procedures for using York Hospital Stryker Osteosynthesis devices and York instruments. USA It offers guidance that you should heed, but, as with any such technical guide, each surgeon must consider the particular needs of each patient and make appropriate adjustments when and as required. A workshop training is required prior to first surgery. All non-sterile devices must be cleaned and sterilized before use. Follow the instructions provided in our reprocessing guide (L24002000). Multi-component instruments must be disassembled for cleaning. Please refer to the corresponding assembly/ disassembly instructions. See package insert (L22000007) for a complete list of potential adverse effects, contraindications, warnings and precautions. The surgeon must discuss all relevant risks, including the finite lifetime of the device, with the patient, when necessary. Warning: Fixation Screws: Stryker Ostreosynthesis bone screws are not approved or intended for screw attachment or fixation to the posterior elements (pedicles) of the cervical, thoracic or lumbar spine. 2 Contents Page 1. Introduction 4 Implant Features 4 Instrument Features 6 References 6 2. Indications, Precautions and Contraindications 7 Indications 7 Precautions 7 Relative Contraindications 7 3. -

Electric Actuators Vsi-1000 Series
ELECTRIC ACTUATORS TM VSI-1000 SERIES DESCRIPTION VSI-1000 Series Electric Actuators are used on Kele KBV Series butterfly valves to provide two-position (with or without battery backup) or proportional control in a NEMA 4X housing. The VSI-1000 Series comes standard on 8" and larger non-spring return assemblies and on 5" and larger two- position spring return assemblies. They can be ordered on smaller valve assemblies as an option. Standard fea- tures include 2 SPDT fully adjustable auxiliary switches KBV-2-6-E2SO (two-position only), manual override crank, and an inter- assembly includes nal heater to prevent condensation in outdoor installa- VSI-BB1020 actuator tions. SPECIFICATIONS FEATURES Power 120 VAC standard •Lightweight, compact design Models 1005 to 1020 12/24 VDC optional • Two-position or modulating control Models 1005 to 1040 24 VAC optional • Two-position battery-backed models Torque range 347-17,359 in-lb • NEMA 4X watertight, corrosion-resistant housing Motor 120 VAC, 1 phase, 60 Hz; • Integral position indicator enclosed, non-ventilated, high • Space heater standard starting torque, reversible induc- • Two 1/2" conduit connections tion, Class E insulation • Detachable manual override crank Thermal overload Auto reset, embedded • Terminal strip wiring Travel limit switches Cam operated, adjustable SPDT • Worm gear drive, no electro-mechanical brake for open/close stop required • Mounting orientation in any direction Position indicator High-visibility graduated dial • 4-20 mA or 500Ω optional feedback signal Conduit connections -

Urban Society and Communal Independence in Twelfth-Century Southern Italy
Urban society and communal independence in Twelfth-Century Southern Italy Paul Oldfield Submitted in accordance with the requirements for the degree of PhD. The University of Leeds The School of History September 2006 The candidate confirms that the work submitted is his own and that appropriate credit has been given where reference has been made to the work of others. This copy has been supplied on the understanding that it is copyright material and that no quotation from the thesis may be published without proper acknowledgement. Acknowledgements I would like to express my thanks for the help of so many different people, without which there would simply have been no thesis. The funding of the AHRC (formerly AHRB) and the support of the School of History at the University of Leeds made this research possible in the first place. I am grateful too for the general support, and advice on reading and sources, provided by Dr. A. J. Metcalfe, Dr. P. Skinner, Professor E. Van Houts, and Donald Matthew. Thanks also to Professor J-M. Martin, of the Ecole Francoise de Rome, for his continual eagerness to offer guidance and to discuss the subject. A particularly large thanks to Mr. I. S. Moxon, of the School of History at the University of Leeds, for innumerable afternoons spent pouring over troublesome Latin, for reading drafts, and for just chatting! Last but not least, I am hugely indebted to the support, understanding and endless efforts of my supervisor Professor G. A. Loud. His knowledge and energy for the subject has been infectious, and his generosity in offering me numerous personal translations of key narrative and documentary sources (many of which are used within) allowed this research to take shape and will never be forgotten. -

Norman Identity and Historiography in the 11Th-12Th Centuries
Butler Journal of Undergraduate Research Volume 5 2019 The Comedia Normannorum: Norman Identity and Historiography in the 11th-12th Centuries Patrick Stroud Wabash College Follow this and additional works at: https://digitalcommons.butler.edu/bjur Recommended Citation Stroud, Patrick (2019) "The Comedia Normannorum: Norman Identity and Historiography in the 11th-12th Centuries," Butler Journal of Undergraduate Research: Vol. 5 , Article 10. Retrieved from: https://digitalcommons.butler.edu/bjur/vol5/iss1/10 This Article is brought to you for free and open access by the Undergraduate Scholarship at Digital Commons @ Butler University. It has been accepted for inclusion in Butler Journal of Undergraduate Research by an authorized editor of Digital Commons @ Butler University. For more information, please contact [email protected]. BUTLER JOURNAL OF UNDERGRADUATE RESEARCH, VOLUME 5 THE COMEDIA NORMANNORUM: NORMAN IDENTITY AND HISTORIOGRAPHY IN THE 11TH-12TH CENTURIES PATRICK STROUD, WABASH COLLEGE MENTOR: STEPHEN MORILLO Introduction—How Symbols and Ethnography Tie to Historical Myth Since the 1970s, historians have tried many different methodologies for exploring texts. Because multiple paradigms tempt the historian’s gaze, medieval texts can often befuddle readers in their hagiographies and chronologies. At the same time, these texts also give the historian a unique opportunity in the form of cultural insight. In his 1995 work Making History: The Normans and their Historians in Eleventh-Century Italy, Kenneth Baxter Wolf discusses a text’s role in medieval historiography. A professor of History at Pomona College, Wolf divides historical commentary on medieval primary sources into two ends of a spectrum. While one end worries itself on the accuracy and classical “truth” of a source, the other end, postmodern historiography, uses historical records “to tell us how the people who wrote them conceived of the events occurring in the world around them.”1 The historian treats a medieval text as a launching pad for cultural analysis. -

Form OR-20-S, Instructions for Oregon S Corporation Tax Return
Oregon S Corporation Tax Form OR-20-S Instructions 2019 Table of contents Important reminders ............................................ 2 Form instructions What’s new .................................................................... 2 Heading and checkboxes .................................................... 7 Questions ............................................................................... 8 Form changes and looking ahead .............. 3 Line instructions ..................................... 3 Estimated tax payments Additions ............................................................................... 9 Filing information Subtractions ........................................................................ 10 Who must file with Oregon? .............................................. 4 Net loss deduction ............................................................. 10 Excise or income tax? ........................................................... 5 Tax ........................................................................................ 11 Shareholder information ..................................................... 5 Credits .................................................................................. 11 Composite returns ............................................................... 5 LIFO benefit recapture addition ...................................... 11 Withholding requirement ................................................... 5 Net tax ................................................................................. -

Instructions for Form 1125-E (Rev. October 2016)
Userid: CPM Schema: Leadpct: 100% Pt. size: 10 Draft Ok to Print instrx AH XSL/XML Fileid: … s/I1125E/201610/A/XML/Cycle04/source (Init. & Date) _______ Page 1 of 2 13:39 - 29-Sep-2016 The type and rule above prints on all proofs including departmental reproduction proofs. MUST be removed before printing. Department of the Treasury Instructions Internal Revenue Service for Form 1125-E (Rev. October 2016) Compensation of Officers Section references are to the Internal Revenue Code Disallowance of Deduction for Employee unless otherwise noted. Compensation in Excess of $1 Million Future Developments Publicly held corporations cannot deduct compensation to a “covered employee” to the extent that the compensation For the latest information about developments related to exceeds $1 million. Generally, a covered employee is: Form 1125-E and its instructions, such as legislation The principal executive officer of the corporation (or an enacted after they were published, go to www.irs.gov/ individual acting in that capacity) as of the end of the tax form1125e. year, or An employee whose total compensation must be General Instructions reported to shareholders under the Securities Exchange Act of 1934 because the employee is among the three Purpose of Form highest compensated officers for that tax year (other than Certain entities with total receipts of $500,000 or more use the principal executive officer). Form 1125-E to provide a detailed report of the deduction for compensation of officers. For this purpose, compensation does not include the following. Who Must File Income from certain employee trusts, annuity plans, or Form 1125-E must be completed and attached to Form pensions, and 1120, 1120-C, 1120-F, 1120-RIC, 1120-REIT, or 1120S, if Any benefit paid to an employee that is excluded from the entity has total receipts (defined below) of $500,000 or the employee's income. -
Connecticut Pass-Through Entity
2020 Connecticut FORM Pass-Through CT-1065/ CT-1120SI Entity Tax Instructions This booklet contains Dear Taxpayer, information and 2020 has been a challenging year to say the least. Rest assured, however, instructions about the that the tax professionals at the Connecticut Department of Revenue following forms: Services (DRS) stand ready to provide our customers with world-class service. All of us at DRS have been busy reinventing how the agency • Form CT-1065/ delivers assistance to our citizens. The COVID-19 pandemic has forced CT-1120SI public servants to reflect on how we can improve the delivery of services in a changing environment. I think you will find the DRS approach is • Form CT-1065/ more efficient and convenient. CT-1120SI EXT The instructions in this booklet and our forms that are available on • Form CT-1065/ our website at portal.ct.gov/DRS contain everything you will need to complete your 2020 Connecticut pass‑through entity tax filing. Please CT-1120SI ES remember that electronic filing is the easiest and most efficient way to • Schedule CT K-1 file. In fact, if you are expecting a refund, electronic filing is the sure way to receive that refund as quickly as possible. All of your electronic • Schedule CT-AB filing options are contained in these instructions. • Schedule CT-CE Your feedback is critically important, especially during these challenging times. I encourage you to let us know how we are doing. We welcome • Schedule CT-NR your ideas and suggestions. You may send an email or call to personally speak to a Taxpayer Services representative. -

Reimbursement to American Red Cross for Hurricanes Charley, Frances, Ivan, and Jeanne
United States Government Accountability Office GAO Report to Congressional Committees May 2006 DISASTER RELIEF Reimbursement to American Red Cross for Hurricanes Charley, Frances, Ivan, and Jeanne a GAO-06-518 May 2006 DISASTER RELIEF Accountability Integrity Reliability Highlights Reimbursement to American Red Cross Highlights of GAO-06-518, a report to for Hurricanes Charley, Frances, Ivan, congressional committees and Jeanne Why GAO Did This Study What GAO Found In accordance with Public Law 108- The signed agreement between FEMA and the Red Cross properly 324, GAO is required to audit the established criteria for the Red Cross to be reimbursed for allowable reimbursement of up to $70 million expenses for disaster relief, recovery, and emergency services related to of appropriated funds to the hurricanes Charley, Frances, Ivan, and Jeanne. The Red Cross incurred American Red Cross (Red Cross) $88.6 million of allowable expenses. for disaster relief associated with 2004 hurricanes Charley, Frances, Ivan, and Jeanne. The audit was Consistent with the law, the agreement explicitly provided that the Red performed to determine if (1) the Cross would not seek reimbursement for any expenses reimbursed by other Federal Emergency Management federal funding sources. GAO identified $0.3 million of FEMA paid costs that Agency (FEMA) established the Red Cross properly deducted from its reimbursement requests, so as not criteria and defined allowable to duplicate funding by other federal sources. The Red Cross also reduced its expenditures to ensure that requested reimbursements by $60.2 million to reflect private donations for reimbursement claims paid to the disaster relief for the four hurricanes, for a net reimbursement of Red Cross met the purposes of the 28.1 million.