Bq = Becquerel Gy = Gray (Sv = Sievert)
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Nuclear Threat
MANAGEMENT OF RADIOLOGIC CASUALTIES Nuclear Threat . Formerly .Soviet Union .Nuclear fallout . Now .NBC threat against civilians .Accidental exposure of workers and public Images: CIA, FBI Accidental Exposure in Brazil . Cesium-137 source found by scavengers in 1987 . Source broken open, contents shared . 112,800 surveyed for contamination . 120 externally contaminated only . 129 internally & externally contaminated . 20 required hospital treatment . 14 developed bone marrow depression . 8 treated with Granulocyte Macrophage Colony-Stimulating Factors (GM-CSF) . 4 died acute phase, hemorrhage, infection . 1 died in 1994 from liver failure Images: CIA Medical Staff Exposure Medical staff received doses: . Maximum 500 millirem (5 millisieverts) .Natural background radiation dose ~ 200 millirems annually . Average 20 millirem (0.2 millisieverts) .Equivalent to one chest X-ray Juarez, Mexico Incident . 400 curies of cobalt-60 in stainless steel therapy device sold for scrap . Ended up in recycled steel rebar . Wrong turn into Los Alamos lab . I0 people significantly exposed . 1 construction worker died .bone cancer . 109 houses demolished in Mexico Images: CIA US Experience 1944-1999 . 243 radiation accidents leading to “serious” classification . 790 people received significant exposure resulting in 30 fatalities .Incidents included: . 137 industrial . 80 medical . 11 criticality Image: DOE The Basics of Radiation Radiation is energy that comes from a source and travels through matter or space Radioactivity is the spontaneous emission of radiation: . Either directly from unstable atomic nuclei, or . As a consequence of a nuclear reaction, or . Machine – produced (X-ray) Image: NOAA Contamination . Defined as internal or external deposition of radioactive particles . Irradiation continues until source removed by washing, flushing or radioactive decay . -

Unerring in Her Scientific Enquiry and Not Afraid of Hard Work, Marie Curie Set a Shining Example for Generations of Scientists
Historical profile Elements of inspiration Unerring in her scientific enquiry and not afraid of hard work, Marie Curie set a shining example for generations of scientists. Bill Griffiths explores the life of a chemical heroine SCIENCE SOURCE / SCIENCE PHOTO LIBRARY LIBRARY PHOTO SCIENCE / SOURCE SCIENCE 42 | Chemistry World | January 2011 www.chemistryworld.org On 10 December 1911, Marie Curie only elements then known to or ammonia, having a water- In short was awarded the Nobel prize exhibit radioactivity. Her samples insoluble carbonate akin to BaCO3 in chemistry for ‘services to the were placed on a condenser plate It is 100 years since and a chloride slightly less soluble advancement of chemistry by the charged to 100 Volts and attached Marie Curie became the than BaCl2 which acted as a carrier discovery of the elements radium to one of Pierre’s electrometers, and first person ever to win for it. This they named radium, and polonium’. She was the first thereby she measured quantitatively two Nobel prizes publishing their results on Boxing female recipient of any Nobel prize their radioactivity. She found the Marie and her husband day 1898;2 French spectroscopist and the first person ever to be minerals pitchblende (UO2) and Pierre pioneered the Eugène-Anatole Demarçay found awarded two (she, Pierre Curie and chalcolite (Cu(UO2)2(PO4)2.12H2O) study of radiactivity a new atomic spectral line from Henri Becquerel had shared the to be more radioactive than pure and discovered two new the element, helping to confirm 1903 physics prize for their work on uranium, so reasoned that they must elements, radium and its status. -

Absorbed Dose in Radioactive Media Outline Introduction Radiation Equilibrium Charged-Particle Equilibrium Limiting Cases
Outline • General dose calculation considerations, Absorbed Dose in Radioactive absorbed fraction Media • Radioactive disintegration processes and associated dose deposition – Alpha disintegration Chapter 5 – Beta disintegration – Electron-capture transitions F.A. Attix, Introduction to Radiological – Internal conversion Physics and Radiation Dosimetry • Summary Introduction Radiation equilibrium • We are interested in calculating the absorbed dose in a. The atomic composition radioactive media, applicable to cases of of the medium is – Dose within a radioactive organ homogeneous – Dose in one organ due to radioactive source in another b. The density of the organ medium is • If conditions of CPE or RE are satisfied, dose homogeneous c. The radioactive source calculation is straightforward is uniformly distributed • Intermediate situation is more difficult but can be d. No external electric or handled at least in approximations magnetic fields are present Charged-particle equilibrium Limiting cases • Emitted radiation typically includes both • Each charged particle of a given type and photons (longer range) and charged energy leaving the volume is replaced by an particles (shorter range) identical particle of the same energy entering • Assume the conditions for RE are satisfied the volume • Consider two • Existence of RE is sufficient condition for CPE limited cases based • Even if RE does not exist CPE may still exist on the size of the (for a very large or a very small volume) radioactive object 1 Limiting cases: small object Limiting -

3.Joule's Experiments
The Force of Gravity Creates Energy: The “Work” of James Prescott Joule http://www.bookrags.com/biography/james-prescott-joule-wsd/ James Prescott Joule (1818-1889) was the son of a successful British brewer. He tinkered with the tools of his father’s trade (particularly thermometers), and despite never earning an undergraduate degree, he was able to answer two rather simple questions: 1. Why is the temperature of the water at the bottom of a waterfall higher than the temperature at the top? 2. Why does an electrical current flowing through a conductor raise the temperature of water? In order to adequately investigate these questions on our own, we need to first define “temperature” and “energy.” Second, we should determine how the measurement of temperature can relate to “heat” (as energy). Third, we need to find relationships that might exist between temperature and “mechanical” energy and also between temperature and “electrical” energy. Definitions: Before continuing, please write down what you know about temperature and energy below. If you require more space, use the back. Temperature: Energy: We have used the concept of gravity to show how acceleration of freely falling objects is related mathematically to distance, time, and speed. We have also used the relationship between net force applied through a distance to define “work” in the Harvard Step Test. Now, through the work of Joule, we can equate the concepts of “work” and “energy”: Energy is the capacity of a physical system to do work. Potential energy is “stored” energy, kinetic energy is “moving” energy. One type of potential energy is that induced by the gravitational force between two objects held at a distance (there are other types of potential energy, including electrical, magnetic, chemical, nuclear, etc). -
Modern Physics Unit 15: Nuclear Structure and Decay Lecture 15.1: Nuclear Characteristics
Modern Physics Unit 15: Nuclear Structure and Decay Lecture 15.1: Nuclear Characteristics Ron Reifenberger Professor of Physics Purdue University 1 Nucleons - the basic building blocks of the nucleus Also written as: 7 3 Li ~10-15 m Examples: A X=Chemical Element Z X Z = number of protons = atomic number 12 A = atomic mass number = Z+N 6 C N= A-Z = number of neutrons 35 17 Cl 2 What is the size of a nucleus? Three possibilities • Range of nuclear force? • Mass radius? • Charge radius? It turns out that for nuclear matter Nuclear force radius ≈ mass radius ≈ charge radius defines nuclear force range defines nuclear surface 3 Nuclear Charge Density The size of the lighter nuclei can be approximated by modeling the nuclear charge density ρ (C/m3): t ≈ 4.4a; a=0.54 fm 90% 10% Usually infer the best values for ρo, R and a for a given nucleus from scattering experiments 4 Nuclear mass density Scattering experiments indicate the nucleus is roughly spherical with a radius given by 1 3 −15 R = RRooA ; =1.07 × 10meters= 1.07 fm = 1.07 fermis A=atomic mass number What is the nuclear mass density of the most common isotope of iron? 56 26 Fe⇒= A56; Z = 26, N = 30 m Am⋅⋅3 Am 33A ⋅ m m ρ = nuc p= p= pp = o 1 33 VR4 3 3 3 44ππA R nuc π R 4(π RAo ) o o 3 3×× 1.66 10−27 kg = 3.2× 1017kg / m 3 4×× 3.14 (1.07 × 10−15m ) 3 The mass density is constant, independent of A! 5 Nuclear mass density for 27Al, 97Mo, 238U (from scattering experiments) (kg/m3) ρo heavy mass nucleus light mass nucleus middle mass nucleus 6 Typical Densities Material Density Helium 0.18 kg/m3 Air (dry) 1.2 kg/m3 Styrofoam ~100 kg/m3 Water 1000 kg/m3 Iron 7870 kg/m3 Lead 11,340 kg/m3 17 3 Nuclear Matter ~10 kg/m 7 Isotopes - same chemical element but different mass (J.J. -
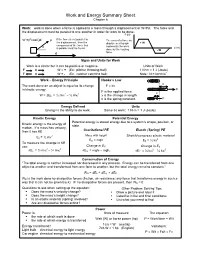
Work and Energy Summary Sheet Chapter 6
Work and Energy Summary Sheet Chapter 6 Work: work is done when a force is applied to a mass through a displacement or W=Fd. The force and the displacement must be parallel to one another in order for work to be done. F (N) W =(Fcosθ)d F If the force is not parallel to The area of a force vs. the displacement, then the displacement graph + W component of the force that represents the work θ d (m) is parallel must be found. done by the varying - W d force. Signs and Units for Work Work is a scalar but it can be positive or negative. Units of Work F d W = + (Ex: pitcher throwing ball) 1 N•m = 1 J (Joule) F d W = - (Ex. catcher catching ball) Note: N = kg m/s2 • Work – Energy Principle Hooke’s Law x The work done on an object is equal to its change F = kx in kinetic energy. F F is the applied force. 2 2 x W = ΔEk = ½ mvf – ½ mvi x is the change in length. k is the spring constant. F Energy Defined Units Energy is the ability to do work. Same as work: 1 N•m = 1 J (Joule) Kinetic Energy Potential Energy Potential energy is stored energy due to a system’s shape, position, or Kinetic energy is the energy of state. motion. If a mass has velocity, Gravitational PE Elastic (Spring) PE then it has KE 2 Mass with height Stretch/compress elastic material Ek = ½ mv 2 EG = mgh EE = ½ kx To measure the change in KE Change in E use: G Change in ES 2 2 2 2 ΔEk = ½ mvf – ½ mvi ΔEG = mghf – mghi ΔEE = ½ kxf – ½ kxi Conservation of Energy “The total energy is neither increased nor decreased in any process. -

Estimation of the Collective Effective Dose to the Population from Medical X-Ray Examinations in Finland
Estimation of the collective effective dose to the population from medical x-ray examinations in Finland Petra Tenkanen-Rautakoskia, Hannu Järvinena, Ritva Blya aRadiation and Nuclear Safety Authority (STUK), PL 14, 00880 Helsinki, Finland Abstract. The collective effective dose to the population from all x-ray examinations in Finland in 2005 was estimated. The numbers of x-ray examinations were collected by a questionnaire to the health care units (response rate 100 %). The effective doses in plain radiography were calculated using a Monte Carlo based program (PCXMC), as average values for selected health care units. For computed tomography (CT), weighted dose length product (DLPw) in a standard phantom was measured for routine CT protocols of four body regions, for 80 % of CT scanners including all types. The effective doses were calculated from DPLw values using published conversion factors. For contrast-enhanced radiology and interventional radiology, the effective dose was estimated mainly by using published DAP values and conversion factors for given body regions. About 733 examinations per 1000 inhabitants (excluding dental) were made in 2005, slightly less than in 2000. The proportions of plain radiography, computed tomography, contrast-enhanced radiography and interventional procedures were about 92, 7, 1 and 1 %, respectively. From 2000, the frequencies (number of examinations per 1000 inhabitants) of plain radiography and contrast-enhanced radiography have decreased about 8 and 33 %, respectively, while the frequencies of CT and interventional radiology have increased about 28 and 38 %, respectively. The population dose from all x-ray examinations is about 0,43 mSv per person (in 1997 0,5 mSv). -

Nuclear Radiation 1. an Atom Contains Electrons, Protons and Neutrons
Nuclear Radiation 1. An atom contains electrons, protons and neutrons. Which of these particles a) are outside the nucleus b) are uncharged c) have a negative charge d) are nucleons e) are much lighter than the others? 2. Complete the table below. Name Symbol Charge What is it? Alpha particle β -1 Gamma ray An electromagnetic wave 3. How is an ionised material different from a material that is not ionised? National 5 Physics: Waves & Radiation 1 Absorption of Radiation 1. The figure below shows a Geiger tube used to detect radiation from a radioactive source. thick lead plate 0 4 2 5 start counter stop ON OFF reset Geiger tube radioactive source The following measurements were made using the apparatus above. Counts in 300 seconds Readings Average 1 No source present 102 94 110 2 Source present at fixed distance from tube a) No lead plate present 3466 3420 3410 b) Thick lead plate present 105 109 89 c) Aluminium sheet in place of the 1834 1787 1818 thick lead sheet a) Complete the table by calculating the average readings. b) Why are the readings on each line not the same? c) What can you say from the table about the effect on the radiation of: i. The lead plate? ii. The aluminium plate? d) Why is it possible to say from the readings that: i. gamma radiation is emitted by the source? ii. alpha and beta radiation might be emitted by the source? e) What further tests could you make using this arrangement to find out whether or not the source emits alpha radiation? National 5 Physics: Waves & Radiation 2 2. -

Uranium Fact Sheet
Fact Sheet Adopted: December 2018 Health Physics Society Specialists in Radiation Safety 1 Uranium What is uranium? Uranium is a naturally occurring metallic element that has been present in the Earth’s crust since formation of the planet. Like many other minerals, uranium was deposited on land by volcanic action, dissolved by rainfall, and in some places, carried into underground formations. In some cases, geochemical conditions resulted in its concentration into “ore bodies.” Uranium is a common element in Earth’s crust (soil, rock) and in seawater and groundwater. Uranium has 92 protons in its nucleus. The isotope2 238U has 146 neutrons, for a total atomic weight of approximately 238, making it the highest atomic weight of any naturally occurring element. It is not the most dense of elements, but its density is almost twice that of lead. Uranium is radioactive and in nature has three primary isotopes with different numbers of neutrons. Natural uranium, 238U, constitutes over 99% of the total mass or weight, with 0.72% 235U, and a very small amount of 234U. An unstable nucleus that emits some form of radiation is defined as radioactive. The emitted radiation is called radioactivity, which in this case is ionizing radiation—meaning it can interact with other atoms to create charged atoms known as ions. Uranium emits alpha particles, which are ejected from the nucleus of the unstable uranium atom. When an atom emits radiation such as alpha or beta particles or photons such as x rays or gamma rays, the material is said to be undergoing radioactive decay (also called radioactive transformation). -

THE COLLECTIVE EFFECTIVE DOSE RESULTING from RADIATION EMITTED DURING the FIRST WEEKS of the FUKUSHIMA DAIICHI NUCLEAR ACCIDENT Matthew Mckinzie, Ph.D
THE COLLECTIVE EFFECTIVE DOSE RESULTING FROM RADIATION EMITTED DURING THE FIRST WEEKS OF THE FUKUSHIMA DAIICHI NUCLEAR ACCIDENT Matthew McKinzie, Ph.D. and Thomas B. Cochran, Ph.D., Natural Resources Defense Council April 10, 2011 The Magnitude 9.0 earthquake off Japan’s Pacific Coast, which was the initiating event for accidents at four of the six reactors at the Fukushima Daiichi nuclear power plant, occurred at 14:46 local time on March 11th. At 15:41 a tsunami hit the plant and a station blackout ensued. A reconstruction of the accident progression by Areva1 posited that the final option for cooling the reactors – the reactor core isolation pumps – failed just hours later in Unit 1 (at 16:36), failed in the early morning of March 13th in Unit 3 (at 02:44), and failed early in the afternoon of March 14th in Unit 2 (at 13:25). Radiological releases spiked beginning on March 15th and in the Areva analysis are attributed to the venting of the reactor pressure vessels, explosion in Unit 2, and – significantly – explosion and fire in Unit 4. Fuel had been discharged from the Unit 4 reactor core to the adjacent spent fuel pool on November 30, 2010, raising the possibility of a core melt “on fresh air.” The Japanese Ministry of Education, Culture, Sports, Science and Technology (MEXT) has posted hourly dose rates by prefecture2 on its website. We do not currently know the geographic coordinates of these radiation monitoring sites. The English language versions of the hourly dose rate measurements by prefecture begin in table form at 17:00 on March 16th, and hourly dose rates are provided as charts3 beginning at 00:00 on March 14th. -
Guide for the Use of the International System of Units (SI)
Guide for the Use of the International System of Units (SI) m kg s cd SI mol K A NIST Special Publication 811 2008 Edition Ambler Thompson and Barry N. Taylor NIST Special Publication 811 2008 Edition Guide for the Use of the International System of Units (SI) Ambler Thompson Technology Services and Barry N. Taylor Physics Laboratory National Institute of Standards and Technology Gaithersburg, MD 20899 (Supersedes NIST Special Publication 811, 1995 Edition, April 1995) March 2008 U.S. Department of Commerce Carlos M. Gutierrez, Secretary National Institute of Standards and Technology James M. Turner, Acting Director National Institute of Standards and Technology Special Publication 811, 2008 Edition (Supersedes NIST Special Publication 811, April 1995 Edition) Natl. Inst. Stand. Technol. Spec. Publ. 811, 2008 Ed., 85 pages (March 2008; 2nd printing November 2008) CODEN: NSPUE3 Note on 2nd printing: This 2nd printing dated November 2008 of NIST SP811 corrects a number of minor typographical errors present in the 1st printing dated March 2008. Guide for the Use of the International System of Units (SI) Preface The International System of Units, universally abbreviated SI (from the French Le Système International d’Unités), is the modern metric system of measurement. Long the dominant measurement system used in science, the SI is becoming the dominant measurement system used in international commerce. The Omnibus Trade and Competitiveness Act of August 1988 [Public Law (PL) 100-418] changed the name of the National Bureau of Standards (NBS) to the National Institute of Standards and Technology (NIST) and gave to NIST the added task of helping U.S. -

Copyright by Arthur Bryan Crawford 2004
Copyright by Arthur Bryan Crawford 2004 The Dissertation Committee for Arthur Bryan Crawford Certifies that this is the approved version of the following dissertation: Evaluation of the Impact of Non -Uniform Neutron Radiation Fields on the Do se Received by Glove Box Radiation Workers Committee: Steven Biegalski, Supervisor Sheldon Landsberger John Howell Ofodike Ezekoye Sukesh Aghara Evaluation of the Impact of Non -Uniform Neutron Radiation Fields on the Dose Received by Glove Box Radiation Workers by Arthur Bryan Crawford, B.S., M.S. Dissertation Presented to the Faculty of the Graduate School of The University of Texas at Austin in Partial Fulfillment of the Requirements for the Degree of Doctor of Philosophy The University of Texas at Austin December, 2004 Dedication I was born to goodly parents Harvey E. Crawford and Johnnie Lee Young Crawford Acknowledgements I would like to express my gratitude to Dr. Sheldon Landsberger for his vision in starting a distance learning program at the University of Texas at Austin and for his support and encouragement on this quest. I would like to thank my advisor, Dr. Steven Biegalski, for his support and encouragement even though the topic area was new to him. I would like to thank the members of my dissertation committee for finding the time to review this dissertation. To the staff of the Nuclear Engineering Teaching Laboratory I say thank you for your kindness and support during those brief times that I was on cam pus. A special thanks to my past and present group leaders, David Seidel, Eric McNamara, and Bill Eisele and my Division Leader, Lee McAtee, at Los Alamos National Laboratory, for their support in being allowed to use time and material resources at the Lab oratory and for financial support in the form of tuition reimbursement and travel expenses.