Laser-Assisted Uvulopalatoplasty for Snoring: Medium- to Long-Term Subjective and Objective Analysis
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

(FNE) and Nasal Endoscopy in Ireland During COVID-19 Pandemic Rev 1
Royal College of Surgeons in Ireland Coláiste Ríoga na Máinleá in Éirinn Interim Clinical Guidance on Flexible Nasendoscopy (FNE) and Nasal Endoscopy in Ireland during COVID-19 pandemic Rev 1 INTERIM CLINICAL GUIDANCE ON FLEXIBLE NASENDOSCOPY (FNE) AND NASAL ENDOSCOPY IN IRELAND DURING COVID-19 PANDEMIC Rev 1 INTERIM CLINICAL GUIDANCE ON FLEXIBLE NASENDOSCOPY (FNE) AND NASAL ENDOSCOPY IN IRELAND DURING COVID-19 PANDEMIC Table of Contents 1. Overview ............................................................................................................................................................................. 2 2. Purpose ............................................................................................................................................................................... 2 3. Authorship ......................................................................................................................................................................... 2 4. Target Audience .............................................................................................................................................................. 2 5. Introduction ....................................................................................................................................................................... 2 6. Risk of infection associated with FNE .................................................................................................................. 2 7. Aerosol Generating Procedures -

Surgical Treatment of Snoring and Obstructive Sleep Apnea Syndrome
Medical Policy Surgical Treatment of Snoring and Obstructive Sleep Apnea Syndrome Table of Contents Policy: Commercial Coding Information Information Pertaining to All Policies Policy: Medicare Description References Authorization Information Policy History Policy Number: 130 BCBSA Reference Number: 7.01.101 Related Policies None Policy Commercial Members: Managed Care (HMO and POS), PPO, and Indemnity Medicare HMO BlueSM and Medicare PPO BlueSM Members Uvulopalatopharyngoplasty (UPPP) may be MEDICALLY NECESSARY for the treatment of clinically significant obstructive sleep apnea syndrome (OSAS) in appropriately selected adult patients who have failed an adequate trial of continuous positive airway pressure (CPAP) or failed an adequate trial of an oral appliance (OA). Clinically significant OSA is defined as those patients who have: Apnea/hypopnea Index (AHI) or Respiratory Disturbance Index (RDI) 15 or more events per hour, or AHI or RDI 5 or more events and 14 or less events per hour with documented symptoms of excessive daytime sleepiness, impaired cognition, mood disorders or insomnia, or documented hypertension, ischemic heart disease, or history of stroke. Hyoid suspension, surgical modification of the tongue, and/or maxillofacial surgery, including mandibular- maxillary advancement (MMA), may be MEDICALLY NECESSARY in appropriately selected adult patients with clinically significant OSA and objective documentation of hypopharyngeal obstruction who have failed an adequate trial of continuous positive airway pressure (CPAP) or failed an adequate trial of an oral appliance (OA). Clinically significant OSA is defined as those patients who have: AHI or RDI 15 or more events per hour, or AHI or RDI 5 or more events and 14 or less events per hour with documented symptoms of excessive daytime sleepiness, impaired cognition, mood disorders or insomnia, or documented hypertension, ischemic heart disease, or history of stroke. -

Home Care After Sleep Surgery-Uvulopalatopharyngoplasty (UP3) And/Or Tonsillectomy
Home Care after Sleep Surgery-Uvulopalatopharyngoplasty (UP3) and/or Tonsillectomy The above surgeries are all performed on patients to help relieve or lessen the symptoms of sleep apnea. All address the palate, or the upper part of your throat. General Information You may lack energy for several days, and may also be restless at night. This will improve over the next 10 to 14 days. It is quite common to feel progressively worse during the first five to six days after surgery. You may also become constipated during this time for three reasons: you will not be eating a regular diet, you will be taking pain medications, and you may be less active. Wound Care All of the above surgeries are performed within the mouth on the upper throat. No external incisions are made, all are internal. Depending on the surgery, you may feel and/or see some suture on your palate (upper throat). This is normal and will dissolve over the next two weeks. No specific wound care is necessary for these procedures. Diet It is important for you to drink plenty of fluids after surgery. Drink every hour while awake. A soft diet is recommended for the first 14 days (anything that you may eat without teeth constitutes as a soft diet). Avoid hot liquids/solids. It is alright if you don’t feel like eating much, as long as you drink lots of fluids. Signs that you need to drink more are when the urine is darker in color (urine should be pale yellow). A high fever that persists may also be a sign that you are not taking in enough fluids. -
The Importance of Orofacial Myofunctional Therapy Before and After CO2 Laser Frenectomy in Achieving Optimal Orofacial Function
LASERfocus The Importance of Orofacial Myofunctional Therapy Before and After CO2 Laser Frenectomy in Achieving Optimal Orofacial Function by Karen M. Wuertz, DDS, ABCDSM, DABLS, FOM, and Brooke Pettus, RDH, BSDH, COMS Frenectomy Methods ing, speaking, and breathing patterns may be Frenotomies performed with a scalpel or scissors can be accompanied by caused by incorrect oral posture and oral re- significant bleeding, obscuring the surgical field making it difficult to ensure strictions. Therefore, in the authors’ opinion, if the restriction has been completely removed. Because of the increased risk the removal of oral restrictions is necessary to of early primary closure of the site, postoperative active wound care is es- attain optimal orofacial function, and must be sential to reduce the risk of potential scarring. To properly restore and main- combined with regular pre- and post-frenecto- tain optimum function, active wound care should be implemented as soon my orofacial myofunctional therapy (OMT).1,4 as possible. However, if sutures are placed, the active wound care may be OMT helps re-educate the tongue and orofa- delayed so as not to cause early tearing of tissue. Due to the contact nature of cial muscles during movement and at rest to conventional procedure, there is a certain potential for infection; in addition, create new neuromuscular patterns for proper higher levels of postoperative pain and discomfort have been reported.1,2 Elec- oral function, including chewing, swallowing, trocautery and a hot glass tip of dental diodes may leave a fairly substantial speaking, and breathing.5,6 Camacho et al.7 zone of thermal tissue change3 and may result in delayed healing. -

Tonsillotomy (Partial) and Complete Tonsillectomy
OPEN ACCESS ATLAS OF OTOLARYNGOLOGY, HEAD & NECK OPERATIVE SURGERY TONSILLOTOMY (PARTIAL) & COMPLETE TONSILLECTOMY - SURGICAL TECHNIQUE Klaus Stelter and Goetz Lehnerdt Acute tonsillitis is treated with steroids e.g. first and easiest-to-reach station of the dexamethasone, NSAIDs e.g. ibuprofen and mucosa associated lymphoid tissue system beta-lactam antibiotics e.g. penicillin or cef- (MALT) 2-4. As the main phase of the im- uroxime. Only 10 days of antibiotic therapy mune acquisition continues until the age of has proven to be effective to prevent rheu- 6yrs, the palatine tonsils are physiological- matic fever and glomerulonephritis. ly hyperplastic at this time 5, 6. This is followed by involution, which is reflected Tonsillectomy is only done for recurrent by regression of tonsil size until age 12yrs acute bacterial tonsillitis, or for noninfec- 7. tious reasons such as suspected neoplasia. The lymphoid tissue is separated by a cap- Partial tonsillectomy (tonsillotomy) is the sule from the surrounding muscle (superior 1st line treatment for snoring due to tonsillar pharyngeal constrictor) 8. The blood supply hyperplasia. It is low-risk, and postopera- originates from four different vessels, the tive pain and risk of haemorrhage are much lingual artery, the ascending pharyngeal less than with tonsillectomy. It is immate- artery and the ascending and descending rial whether the tonsillotomy is done with palatine arteries. These vessels radiate laser, radiofrequency, shaver, coblation, bi- mainly to the upper and lower tonsillar polar scissors or monopolar electrocautery, poles, as well as to the centre of the tonsil as long as the crypts remain open and some from laterally 9. -

Read Full Article
PEDIATRIC/CRANIOFACIAL Pharyngeal Flap Outcomes in Nonsyndromic Children with Repaired Cleft Palate and Velopharyngeal Insufficiency Stephen R. Sullivan, M.D., Background: Velopharyngeal insufficiency occurs in 5 to 20 percent of children M.P.H. following repair of a cleft palate. The pharyngeal flap is the traditional secondary Eileen M. Marrinan, M.S., procedure for correcting velopharyngeal insufficiency; however, because of M.P.H. perceived complications, alternative techniques have become popular. The John B. Mulliken, M.D. authors’ purpose was to assess a single surgeon’s long-term experience with a Boston, Mass.; and Syracuse, N.Y. tailored superiorly based pharyngeal flap to correct velopharyngeal insufficiency in nonsyndromic patients with a repaired cleft palate. Methods: The authors reviewed the records of all children who underwent a pharyngeal flap performed by the senior author (J.B.M.) between 1981 and 2008. The authors evaluated age of repair, perceptual speech outcome, need for a secondary operation, and complications. Success was defined as normal or borderline sufficient velopharyngeal function. Failure was defined as borderline insufficiency or severe velopharyngeal insufficiency with recommendation for another procedure. Results: The authors identified 104 nonsyndromic patients who required a pharyngeal flap following cleft palate repair. The mean age at pharyngeal flap surgery was 8.6 Ϯ 4.9 years. Postoperative speech results were available for 79 patients. Operative success with normal or borderline sufficient velopharyngeal function was achieved in 77 patients (97 percent). Obstructive sleep apnea was documented in two patients. Conclusion: The tailored superiorly based pharyngeal flap is highly successful in correcting velopharyngeal insufficiency, with a low risk of complication, in non- syndromic patients with repaired cleft palate. -
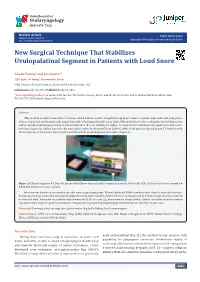
New Surgical Technique That Stabilizes Uvulopalatinal Segment in Patients with Loud Snore
Global Journal of Otolaryngology ISSN 2474-7556 Review Article Glob J Otolaryngol Volume 8 Issue 5 - July 2017 Copyright © All rights are reserved by Jon Garito DOI: 10.19080/GJO.2017.08.555748 New Surgical Technique That Stabilizes Uvulopalatinal Segment in Patients with Loud Snore Novak Vukoje1 and Jon Garito2* 1ENT office “dr Vukoje”, Petrovaradin, Serbia 2PhD, Inventer the dual Frequency device and the RF electrodes, USA Submission: July 01, 2017; Published: July 13, 2017 *Corresponding author: Jon Garito, PhD, Inventer the dual Frequency device and the RF electrodes, 1111 Crandon, BLVD, FL 33149, USA, Tel: ; Email: Abstract This method is author’s innovative technique which follows number of applied surgical procedures on palate and uvula with only goal to advance functional results and avoid complications like velofaringeal insufficiency. Task of this method is to solve uvulopalato lateral obstruction and to expand oropharyngeal airway. It was introduced in the year 2000 by Dr. Vukoje. It requires strict indications for application and correct selection of patients. Author has done this surgical procedure in the period from 2000 to 2004, on 36 patients (19 males and 17 females) with the average age of 45.3 years. Patient selection followed thorough diagnostic procedure (Figure 1). Figure 1: Ellman Surgitron 4.0 Dual RF, patented by Ellman International Company, Oceanside, New York, USA. (US Patent reference number # 5.954.686-Inventor dr Jon C. Garito). Interventions have been executed using radio wave surgical apparatus “Ellman Sugitron 4.0MHz combined with classical surgical technique. Follow-up, done two years after the surgery, imply that noisy sleep ceased to exist in 72.2% of cases (26) and in 19.4% of cases (7) it was reduced to tolerable level. -

Surgical Treatments for Obstructive Sleep Apnea (OSA) Policy Number: PG0056 ADVANTAGE | ELITE | HMO Last Review: 06/01/2021
Surgical Treatments for Obstructive Sleep Apnea (OSA) Policy Number: PG0056 ADVANTAGE | ELITE | HMO Last Review: 06/01/2021 INDIVIDUAL MARKETPLACE | PROMEDICA MEDICARE PLAN | PPO GUIDELINES This policy does not certify benefits or authorization of benefits, which is designated by each individual policyholder terms, conditions, exclusions and limitations contract. It does not constitute a contract or guarantee regarding coverage or reimbursement/payment. Self-Insured group specific policy will supersede this general policy when group supplementary plan document or individual plan decision directs otherwise. Paramount applies coding edits to all medical claims through coding logic software to evaluate the accuracy and adherence to accepted national standards. This medical policy is solely for guiding medical necessity and explaining correct procedure reporting used to assist in making coverage decisions and administering benefits. SCOPE X Professional _ Facility DESCRIPTION Sleep apnea is a disorder where breathing nearly or completely stops for periods of time during sleep. In obstructive sleep apnea (OSA), the brain sends the message to breathe, but there is a blockage to air flowing into the chest. It is a condition in which repetitive episodes of upper airway obstruction occur during sleep. The obstruction may be localized to one or two areas, or may encompass the entire upper airway passages to include the nasal cavity (nose), oropharynx (palate, tonsils, tonsillar pillars) and hypopharynx (tongue base). The hallmark symptom of OSA is excessive daytime sleepiness, and the typical clinical sign of OSA is snoring, which can abruptly cease and be followed by gasping associated with a brief arousal from sleep. The snoring resumes when the patient falls back to sleep, and the cycle of snoring/apnea/arousal may be repeated as frequently as every minute throughout the night. -

How to Care for Your Child After Tonsillectomy Surgery
How to Care for Your Child After Tonsillectomy Surgery 1 IMPORTANT PHONE NUMBERS Children’s Mercy Hospital Kansas ENT Clinic: (913) 696-8620 Children’s Mercy Adele Hall Campus ENT Clinic: (816) 234-3040 Contact a nurse after hours and on weekends: (816) 234-3188 Emergency: 911 Your Surgeon: _____________________________________ Primary Care Physician: _____________________________ © The Children’s Mercy Hospital, 2017 2 TONSILLECTOMY and/or ADENOIDECTOMY (T&A) SURGERY • This is a very common and safe operation. It is the second most common surgery performed on children. • It is normal to see white patches on the back of your child’s throat. Do not remove them. • Your child will have scabs in the back of his/her throat. The scabs will fall off on their own about seven days after surgery. 3 PAIN • Your child may have a sore throat, neck and/or ear pain for 2-3 weeks after surgery. The pain may be the worst for 3-4 days after surgery. One to two weeks after surgery, pain may worsen because the scabs are falling off. • It is important to control your child’s pain after surgery. This helps your child drink and eat. • Your child may have bad ear pain after surgery. Ear pain is actually pain coming from the throat. This is normal. It may last for up to three weeks after surgery. Pain medication, chewing gum or eating chewy foods (like gummy bears) should help. • Give your child pain medicine at set times for 2-4 days after surgery even if he/she doesn’t seem to have a lot of pain. -

Stanford University
STANFORD UNIVERSITY CURRICULUM VITAE Updated September 2019 NAME Stanley Yung-Chuan Liu, MD, DDS POSITION Assistant Professor of Otolaryngology Stanford University School of Medicine Co-Director, Sleep Surgery Fellowship EDUCATION Date Attended Institution Degree, Title Major 9/25/96 - 6/11/00 Stanford University B.S. Biology 8/28/02 - 6/17/07 University of California – San D.D.S. Dentistry Francisco (UCSF), School of Dentistry 9/12/07 - 6/10/11 University of California – San M.D. Medicine Francisco (UCSF), School of Medicine ACADEMIC APPOINTMENTS 6/2013 – 6/2014 Clinical Instructor Department of Otolaryngology, Stanford University School of Medicine Stanford, CA, USA 9/2014 – Present Assistant Professor (Medical Center Line) Department of Otolaryngology, Stanford University School of Medicine Stanford, CA, USA 9/2015 – Present Preceptor Department of Ophthalmology, Stanford University School of Medicine Stanford, CA, USA HOSPITAL APPOINTMENTS/AFFILIATIONS 6/2013 – Present Stanford Hospital and Clinics, Stanford, CA, USA 9/2015 – Present San Francisco Veterans Affairs Hospital, Palo Alto, CA, USA CERTIFICATION 4/2018 – Present Diplomate, American Board of Oral & Maxillofacial Surgery 4/2018 – Present Candidate, American College of Surgeons LICENSURE 2010 – Present California Dental License #59319 2012 – Present California Medical License # A122495 HONORS AND AWARDS 2004 Howard Hughes Medical Institute – NIH Research Scholarship (Cloister Program) 2009 Advanced Training Clinical Research Fellowship, UCSF School of Medicine, 2010 Lightowler -

Post Operative Instructions Tonsillectomy
8230 Walnut Hill Lane 6300 West Parker Road Building 3, Suite 420 Building 2, Suite 221 Dallas, Texas 75231 Plano, Texas 75093 (214) 265-0800 (972) 378-3708 POST OPERATIVE INSTRUCTIONS TONSILLECTOMY WHAT TO EXPECT AFTER SURGERY After tonsils are removed, there is a raw surface on the sides of the throat where the tonsils used to be. Because this takes 7-10 days for the mucous membrane to heal, this is usually painful for the first 7 days after surgery and gradually improves each day thereafter. The tonsil area becomes coated with white/yellow thickened mucous which acts as a protective covering while the area heals. This “eschar” begins to fall off after about 7 days. This often increases the throat pain and can cause pain to be felt in the ears. The ear pain normally subsides in a few days, but pain can still be felt when yawning or sneezing even after 2 weeks after the procedure. The tonsil area completely heals in 2 to 3 weeks in most instances. The uvula, the finger-like tissue that hangs down from the soft palate in the back of the throat, will usually become swollen on the first day or two after surgery. This is normal and is due to the cauterization of the tonsil blood vessels that forces the uvula to swell up until the glands develop an alternative drainage pattern. This can cause patients to have a sensation of something in their throat and feel that their throat is “blocked”. This does not happen and can be improved by drinking cold liquids. -

Treatments for Ankyloglossia and Ankyloglossia with Concomitant Lip-Tie Comparative Effectiveness Review Number 149
Comparative Effectiveness Review Number 149 Treatments for Ankyloglossia and Ankyloglossia With Concomitant Lip-Tie Comparative Effectiveness Review Number 149 Treatments for Ankyloglossia and Ankyloglossia With Concomitant Lip-Tie Prepared for: Agency for Healthcare Research and Quality U.S. Department of Health and Human Services 540 Gaither Road Rockville, MD 20850 www.ahrq.gov Contract No. 290-2012-00009-I Prepared by: Vanderbilt Evidence-based Practice Center Nashville, TN Investigators: David O. Francis, M.D., M.S. Sivakumar Chinnadurai, M.D., M.P.H. Anna Morad, M.D. Richard A. Epstein, Ph.D., M.P.H. Sahar Kohanim, M.D. Shanthi Krishnaswami, M.B.B.S., M.P.H. Nila A. Sathe, M.A., M.L.I.S. Melissa L. McPheeters, Ph.D., M.P.H. AHRQ Publication No. 15-EHC011-EF May 2015 This report is based on research conducted by the Vanderbilt Evidence-based Practice Center (EPC) under contract to the Agency for Healthcare Research and Quality (AHRQ), Rockville, MD (Contract No. 290-2012-00009-I). The findings and conclusions in this document are those of the authors, who are responsible for its contents; the findings and conclusions do not necessarily represent the views of AHRQ. Therefore, no statement in this report should be construed as an official position of AHRQ or of the U.S. Department of Health and Human Services. The information in this report is intended to help health care decisionmakers—patients and clinicians, health system leaders, and policymakers, among others—make well-informed decisions and thereby improve the quality of health care services. This report is not intended to be a substitute for the application of clinical judgment.