207695Orig1s000
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Theophylline and Selective PDE Inhibitors As Bronchodilators and Smooth Muscle Relaxants
Eur Respir J, 1995, 8, 637–642 Copyright ERS Journals Ltd 1995 DOI: 10.1183/09031936.95.08040637 European Respiratory Journal Printed in UK - all rights reserved ISSN 0903 - 1936 SERIES 'THEOPHYLLINE AND PHOSPHODIESTERASE INHIBITORS' Edited by M. Aubier and P.J. Barnes Theophylline and selective PDE inhibitors as bronchodilators and smooth muscle relaxants K.F. Rabe, H. Magnussen, G. Dent Theophylline and selective PDE inhibitors as bronchodilators and smooth muscle relaxants. Krankenhaus Grosshansdorf, Zentrum für K.F. Rabe, H. Magnussen, G. Dent. ERS Journals Ltd 1995. Pneumologie und Thoraxchirurgie, LVA ABSTRACT: In addition to its emerging immunomodulatory properties, theophy- Hamburg, Grosshansdorf, Germany. lline is a bronchodilator and also decreases mean pulmonary arterial pressure in vivo. The mechanism of action of this drug remains controversial; adenosine Correspondence: K.F. Rabe Krankenhaus Grosshansdorf antagonism, phosphodiesterase (PDE) inhibition and other actions have been advanced Wöhrendamm 80 to explain its effectiveness in asthma. Cyclic adenosine monophosphate (AMP) and D-22927 Grosshansdorf cyclic guanosine monophosphate (GMP) are involved in the regulation of smooth Germany muscle tone, and the breakdown of these nucleotides is catalysed by multiple PDE isoenzymes. The PDE isoenzymes present in human bronchus and pulmonary artery Keywords: Bronchi have been identified, and the pharmacological actions of inhibitors of these enzy- 3',5'-cyclic-nucleotide phosphodiesterase mes have been investigated. phosphodiesterase inhibitors Human bronchus and pulmonary arteries are relaxed by theophylline and by pulmonary artery selective inhibitors of PDE III, while PDE IV inhibitors also relax precontracted smooth muscle theophylline bronchus and PDE V/I inhibitors relax pulmonary artery. There appears to be some synergy between inhibitors of PDE III and PDE IV in relaxing bronchus, and Received: February 1 1995 a pronounced synergy between PDE III and PDE V inhibitors in relaxing pulmon- Accepted for publication February 1 1995 ary artery. -
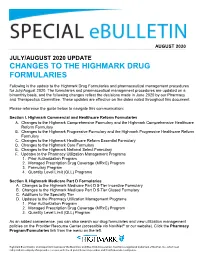
Changes to the Highmark Drug Formularies
AUGUST 2020 JULY/AUGUST 2020 UPDATE CHANGES TO THE HIGHMARK DRUG FORMULARIES Following is the update to the Highmark Drug Formularies and pharmaceutical management procedures for July/August 2020. The formularies and pharmaceutical management procedures are updated on a bimonthly basis, and the following changes reflect the decisions made in June 2020 by our Pharmacy and Therapeutics Committee. These updates are effective on the dates noted throughout this document. Please reference the guide below to navigate this communication: Section I. Highmark Commercial and Healthcare Reform Formularies A. Changes to the Highmark Comprehensive Formulary and the Highmark Comprehensive Healthcare Reform Formulary B. Changes to the Highmark Progressive Formulary and the Highmark Progressive Healthcare Reform Formulary C. Changes to the Highmark Healthcare Reform Essential Formulary D. Changes to the Highmark Core Formulary E. Changes to the Highmark National Select Formulary F. Updates to the Pharmacy Utilization Management Programs 1. Prior Authorization Program 2. Managed Prescription Drug Coverage (MRxC) Program 3. Formulary Program 4. Quantity Level Limit (QLL) Programs Section II. Highmark Medicare Part D Formularies A. Changes to the Highmark Medicare Part D 5-Tier Incentive Formulary B. Changes to the Highmark Medicare Part D 5-Tier Closed Formulary C. Additions to the Specialty Tier D. Updates to the Pharmacy Utilization Management Programs 1. Prior Authorization Program 2. Managed Prescription Drug Coverage (MRxC) Program 3. Quantity Level Limit (QLL) Program As an added convenience, you can also search our drug formularies and view utilization management policies on the Provider Resource Center (accessible via NaviNet® or our website). Click the Pharmacy Program/Formularies link from the menu on the left. -

Drug Name Plate Number Well Location % Inhibition, Screen Axitinib 1 1 20 Gefitinib (ZD1839) 1 2 70 Sorafenib Tosylate 1 3 21 Cr
Drug Name Plate Number Well Location % Inhibition, Screen Axitinib 1 1 20 Gefitinib (ZD1839) 1 2 70 Sorafenib Tosylate 1 3 21 Crizotinib (PF-02341066) 1 4 55 Docetaxel 1 5 98 Anastrozole 1 6 25 Cladribine 1 7 23 Methotrexate 1 8 -187 Letrozole 1 9 65 Entecavir Hydrate 1 10 48 Roxadustat (FG-4592) 1 11 19 Imatinib Mesylate (STI571) 1 12 0 Sunitinib Malate 1 13 34 Vismodegib (GDC-0449) 1 14 64 Paclitaxel 1 15 89 Aprepitant 1 16 94 Decitabine 1 17 -79 Bendamustine HCl 1 18 19 Temozolomide 1 19 -111 Nepafenac 1 20 24 Nintedanib (BIBF 1120) 1 21 -43 Lapatinib (GW-572016) Ditosylate 1 22 88 Temsirolimus (CCI-779, NSC 683864) 1 23 96 Belinostat (PXD101) 1 24 46 Capecitabine 1 25 19 Bicalutamide 1 26 83 Dutasteride 1 27 68 Epirubicin HCl 1 28 -59 Tamoxifen 1 29 30 Rufinamide 1 30 96 Afatinib (BIBW2992) 1 31 -54 Lenalidomide (CC-5013) 1 32 19 Vorinostat (SAHA, MK0683) 1 33 38 Rucaparib (AG-014699,PF-01367338) phosphate1 34 14 Lenvatinib (E7080) 1 35 80 Fulvestrant 1 36 76 Melatonin 1 37 15 Etoposide 1 38 -69 Vincristine sulfate 1 39 61 Posaconazole 1 40 97 Bortezomib (PS-341) 1 41 71 Panobinostat (LBH589) 1 42 41 Entinostat (MS-275) 1 43 26 Cabozantinib (XL184, BMS-907351) 1 44 79 Valproic acid sodium salt (Sodium valproate) 1 45 7 Raltitrexed 1 46 39 Bisoprolol fumarate 1 47 -23 Raloxifene HCl 1 48 97 Agomelatine 1 49 35 Prasugrel 1 50 -24 Bosutinib (SKI-606) 1 51 85 Nilotinib (AMN-107) 1 52 99 Enzastaurin (LY317615) 1 53 -12 Everolimus (RAD001) 1 54 94 Regorafenib (BAY 73-4506) 1 55 24 Thalidomide 1 56 40 Tivozanib (AV-951) 1 57 86 Fludarabine -

Pharmacy and Poisons Act 1979
Q UO N T FA R U T A F E BERMUDA PHARMACY AND POISONS ACT 1979 1979 : 26 TABLE OF CONTENTS PART I PRELIMINARY 1 Short title 2 Interpretation PART II THE PHARMACY COUNCIL 3 The Pharmacy Council 4 Membership of the Council 4A Functions of the Council 4B Protection from personal liability 4C Annual Report 5 Proceedings of the Council, etc PART III REGISTRATION OF PHARMACISTS 6 Offence to practise pharmacy if not registered 7 Registration as a pharmacist 7A Re-registration as non-practising member 7AA Period of validity of registration 8 Code of Conduct 9 Pharmacy Profession Complaints Committee 10 Investigation of complaint by Committee 10A Inquiry into complaint by Council 10B Inquiry by Council of its own initiative 11 Surrender of registration 12 Restoration of name to register 1 PHARMACY AND POISONS ACT 1979 13 Proof of registration 14 Appeals 14A Fees 14B Amendment of Seventh Schedule 15 Regulations for this part PART IV REGISTRATION OF PHARMACIES 16 Register of pharmacies 17 Registration of premises as registered pharmacies 18 Unfit premises: new applications 19 Unfit premises: registered pharmacies 20 Appeals 21 When certificates of unfitness take effect 22 Regulations for this Part PART V CONTROL OF PRESCRIPTIONS AND IMPORTATION 23 Prescriptions to be in a certain form 23A Validity of a prescription 24 Supply by registered pharmacist of equivalent medicines 25 Restrictions on the importation of medicines 26 Declaration relating to imported medicines [repealed] PART VI CONTROL OF DRUGS 27 Certain substances to be sold on prescription -

Phosphodiesterase (PDE)
Phosphodiesterase (PDE) Phosphodiesterase (PDE) is any enzyme that breaks a phosphodiester bond. Usually, people speaking of phosphodiesterase are referring to cyclic nucleotide phosphodiesterases, which have great clinical significance and are described below. However, there are many other families of phosphodiesterases, including phospholipases C and D, autotaxin, sphingomyelin phosphodiesterase, DNases, RNases, and restriction endonucleases, as well as numerous less-well-characterized small-molecule phosphodiesterases. The cyclic nucleotide phosphodiesterases comprise a group of enzymes that degrade the phosphodiester bond in the second messenger molecules cAMP and cGMP. They regulate the localization, duration, and amplitude of cyclic nucleotide signaling within subcellular domains. PDEs are therefore important regulators ofsignal transduction mediated by these second messenger molecules. www.MedChemExpress.com 1 Phosphodiesterase (PDE) Inhibitors, Activators & Modulators (+)-Medioresinol Di-O-β-D-glucopyranoside (R)-(-)-Rolipram Cat. No.: HY-N8209 ((R)-Rolipram; (-)-Rolipram) Cat. No.: HY-16900A (+)-Medioresinol Di-O-β-D-glucopyranoside is a (R)-(-)-Rolipram is the R-enantiomer of Rolipram. lignan glucoside with strong inhibitory activity Rolipram is a selective inhibitor of of 3', 5'-cyclic monophosphate (cyclic AMP) phosphodiesterases PDE4 with IC50 of 3 nM, 130 nM phosphodiesterase. and 240 nM for PDE4A, PDE4B, and PDE4D, respectively. Purity: >98% Purity: 99.91% Clinical Data: No Development Reported Clinical Data: No Development Reported Size: 1 mg, 5 mg Size: 10 mM × 1 mL, 10 mg, 50 mg (R)-DNMDP (S)-(+)-Rolipram Cat. No.: HY-122751 ((+)-Rolipram; (S)-Rolipram) Cat. No.: HY-B0392 (R)-DNMDP is a potent and selective cancer cell (S)-(+)-Rolipram ((+)-Rolipram) is a cyclic cytotoxic agent. (R)-DNMDP, the R-form of DNMDP, AMP(cAMP)-specific phosphodiesterase (PDE) binds PDE3A directly. -

Anagrelide for Gastrointestinal Stromal Tumor
Author Manuscript Published OnlineFirst on December 7, 2018; DOI: 10.1158/1078-0432.CCR-18-0815 Author manuscripts have been peer reviewed and accepted for publication but have not yet been edited. 1 Anagrelide for gastrointestinal stromal tumor Olli-Pekka Pulkka1, Yemarshet K. Gebreyohannes2, Agnieszka Wozniak2, John-Patrick Mpindi3, Olli Tynninen4, Katherine Icay5, Alejandra Cervera5, Salla Keskitalo6, Astrid Murumägi3, Evgeny Kulesskiy3, Maria Laaksonen7, Krister Wennerberg3, Markku Varjosalo6, Pirjo Laakkonen8, Rainer Lehtonen5, Sampsa Hautaniemi5, Olli Kallioniemi3, Patrick Schöffski2, Harri Sihto1*, and Heikki Joensuu1,9* 1Laboratory of Molecular Oncology, Research Programs Unit, Translational Cancer Biology, Department of Oncology, University of Helsinki, Helsinki, Finland. 2Laboratory of Experimental Oncology, Department of Oncology, KU Leuven and Department of General Medical Oncology, University Hospitals Leuven, Leuven, Belgium. 3Institute for Molecular Medicine Finland (FIMM), University of Helsinki, Helsinki, Finland 4Department of Pathology, Haartman Institute, University of Helsinki and HUSLAB, Helsinki, Finland. 5Research Programs Unit, Genome-Scale Biology, Medicum and Department of Biochemistry and Developmental Biology, Faculty of Medicine, University of Helsinki, Helsinki, Finland. 6Institute of Biotechnology, University of Helsinki, Helsinki, Finland. 7MediSapiens Ltd., Helsinki, Finland 8Research Programs Unit, Translational Cancer Biology, University of Helsinki, Helsinki, Finland. 9Comprehensive Cancer Center, -

Rolipram, but Not Siguazodan Or Zaprinast, Inhibits the Excitatory Noncholinergic Neurotransmission in Guinea-Pig Bronchi
Eur Respir J, 1994, 7, 306–310 Copyright ERS Journals Ltd 1994 DOI: 10.1183/09031936.94.07020306 European Respiratory Journal Printed in UK - all rights reserved ISSN 0903 - 1936 Rolipram, but not siguazodan or zaprinast, inhibits the excitatory noncholinergic neurotransmission in guinea-pig bronchi Y. Qian, V. Girard, C.A.E. Martin, M. Molimard, C. Advenier Rolipram, but not siguazodan or zaprinast, inhibits the excitatory noncholinergic neuro- Faculté de Médecine Paris-Ouest Labora- transmission in guinea-pig bronchi. Y. Qian, V. Girard C.A.E. Martin, M. Molimard, toire de Pharmacologie, Paris, France. C. Advenier. ERS Journals Ltd 1994. ABSTRACT: Theophylline has been reported to inhibit excitatory noncholinergic Correspondence: C. Advenier Faculté de Médecine Paris-Ouest but not cholinergic-neurotransmission in guinea-pig bronchi. As theophylline might Laboratoire de Pharmacologie exert this effect through an inhibition of phosphodiesterases (PDE), and since many 15, Rue de l'Ecole de Médecine types of PDE have now been described, the aim of this study was to investigate the F-75270 Paris Cedex 06 effects of three specific inhibitors of PDE on the electrical field stimulation (EFS) France of the guinea-pig isolated main bronchus in vitro. The drugs used were siguazo- dan, rolipram and zaprinast, which specifically inhibit PDE types, III, IV and V, Keywords: C-fibres respectively. neuropeptides Guinea-pig bronchi were stimulated transmurally with biphasic pulses (16 Hz, 1 phosphodiesterase inhibitors ms, 320 mA for 10 s) in the presence of indomethacin 10-6 M and propranolol 10-6 Received: March 11 1993 M. Two successive contractile responses were observed: a rapid cholinergic con- Accepted after revision August 8 1993 traction, followed by a long-lasting contraction due to a local release of neuropep- tides from C-fibre endings. -

Integrated Technologies for the Characterization Of
Integrated technologies for the characterization of phosphodiesterase (PDE) inhibitors Edmond Massuda, Lisa Fleet, Benjamin Lineberry, Laurel Provencher, Abbie Esterman, Dhanrajan Tiruchinapalli, Faith Gawthrop, Christopher Spence, Rajneesh P. Uzgare, Scott Perschke, Seth Cohen, and Hao Chen. 618.01/XX63 Caliper Life Sciences, a PerkinElmer Company, 7170 Standard Drive, Hanover, Maryland, 21076 USA Abstract Phosphodiesterases (PDEs) are a class of signal transduction enzymes regulating various cellular functions and disease Results Results progressions in a number of central or peripheral nervous system-related disorders. For example, these enzymes are involved in neurological diseases including psychosis in schizophrenia, multiple sclerosis and other neurodegenerative PDE1A PDE1B PDE2A PDE3A PDE3B PDE4A1A PDE4B1 Ki and kinact determination using 3D Fit Model 110 110 110 110 110 100 110 110 100 100 100 Percent of Maximum Activity by Time 100 conditions. Thus, safe and highly selective PDE inhibitors or modulators are becoming an important class of disease 100 90 100 90 90 90 90 90 80 90 80 80 80 80 modifying therapeutic agents. We have developed an integrated platform which includes Caliper LabChip™ microfluidic 80 70 80 70 70 70 70 70 60 70 60 60 60 60 mobility-shift assays measuring fluorescent analogs of cAMP and cGMP in conjunction with a cellular assay 60 60 50 50 50 50 50 50 50 40 40 40 40 characterizing intracellular signal transduction in cells modulated by PDE inhibitors. These technologies are useful in 40 40 40 30 30 30 30 %% -

Three-Dimensional Structures of PDE4D in Complex with Roliprams and Implication on Inhibitor Selectivity
View metadata, citation and similar papers at core.ac.uk brought to you by CORE provided by Elsevier - Publisher Connector Structure, Vol. 11, 865–873, July, 2003, 2003 Elsevier Science Ltd. All rights reserved. DOI 10.1016/S0969-2126(03)00123-0 Three-Dimensional Structures of PDE4D in Complex with Roliprams and Implication on Inhibitor Selectivity Qing Huai, Huanchen Wang, Yingjie Sun, 7, and 8 prefer to hydrolyze cAMP, while PDE5, 6, and Hwa-Young Kim, Yudong Liu, and Hengming Ke* 9 are cGMP specific. PDE1, 2, 3, 10, and 11 take both Department of Biochemistry and Biophysics and cAMP and cGMP as their substrates. In the past three Lineberger Comprehensive Cancer Center decades, selective inhibitors against the different PDE The University of North Carolina, Chapel Hill families have been widely studied as cardiotonic agents, Chapel Hill, North Carolina 27599 vasodilators, smooth muscle relaxants, antidepres- sants, antithrombotic compounds, antiasthma com- pounds, and agents for improving cognitive functions Summary such as memory (Reilly and Mohler, 2001; Rotella, 2002; Giembycz, 2000; Souness et al., 2000; Huang et al., Selective inhibitors against the 11 families of cyclic 2001). For example, the PDE5 inhibitor sildenafil (Viagra; nucleotide phosphodiesterases (PDEs) are used to Figure 1) is a drug for male erectile dysfunction, and the treat various human diseases. How the inhibitors se- PDE3 inhibitor cilostamide is a drug for heart diseases. lectively bind the conserved PDE catalytic domains is Selective inhibitors of PDE4 form the largest group of unknown. The crystal structures of the PDE4D2 cata- inhibitors for any PDE family and have been studied as lytic domain in complex with (R)- or (R,S)-rolipram sug- anti-inflammatory drugs targeting asthma and chronic gest that inhibitor selectivity is determined by the obstructive pulmonary disease (COPD) and also as ther- chemical nature of amino acids and subtle conforma- apeutic agents for rheumatoid arthritis, multiple sclero- tional changes of the binding pockets. -

Phosphodiesterase Inhibitors: Could They Be Beneficial for the Treatment of COVID-19?
International Journal of Molecular Sciences Review Phosphodiesterase Inhibitors: Could They Be Beneficial for the Treatment of COVID-19? Mauro Giorgi 1,*, Silvia Cardarelli 2, Federica Ragusa 3, Michele Saliola 1, Stefano Biagioni 1, Giancarlo Poiana 1 , Fabio Naro 2 and Mara Massimi 3,* 1 Department of Biology and Biotechnology “Charles Darwin”, Sapienza University of Rome, 00185 Rome, Italy; [email protected] (M.S.); [email protected] (S.B.); [email protected] (G.P.) 2 Department of Anatomical, Histological, Forensic Medicine and Orthopedic Sciences, Sapienza University, 00185 Rome, Italy; [email protected] (S.C.); [email protected] (F.N.) 3 Department of Life, Health and Environmental Sciences, University of L’Aquila, 67100 L’Aquila, Italy; [email protected] * Correspondence: [email protected] (M.G.); [email protected] (M.M.) Received: 10 July 2020; Accepted: 24 July 2020; Published: 27 July 2020 Abstract: In March 2020, the World Health Organization declared the severe acute respiratory syndrome corona virus 2 (SARS-CoV2) infection to be a pandemic disease. SARS-CoV2 was first identified in China and, despite the restrictive measures adopted, the epidemic has spread globally, becoming a pandemic in a very short time. Though there is growing knowledge of the SARS-CoV2 infection and its clinical manifestations, an effective cure to limit its acute symptoms and its severe complications has not yet been found. Given the worldwide health and economic emergency issues accompanying this pandemic, there is an absolute urgency to identify effective treatments and reduce the post infection outcomes. In this context, phosphodiesterases (PDEs), evolutionarily conserved cyclic nucleotide (cAMP/cGMP) hydrolyzing enzymes, could emerge as new potential targets. -

PFIZER INC. (Exact Name of Registrant As Specified in Its Charter)
UNITED STATES SECURITIES AND EXCHANGE COMMISSION Washington, D.C. 20549 FORM 10-K (Mark One) ☒ ANNUAL REPORT PURSUANT TO SECTION 13 OR 15(d) OF THE SECURITIES EXCHANGE ACT OF 1934 For the fiscal year ended December 31, 2019 ☐ TRANSITION REPORT PURSUANT TO SECTION 13 OR 15(d) OF THE SECURITIES EXCHANGE ACT OF 1934 For the transition period from to Commission file number 1-3619 PFIZER INC. (Exact name of registrant as specified in its charter) Delaware 13-5315170 (State or other jurisdiction of incorporation or organization) (I.R.S. Employer Identification Number) 235 East 42nd Street, New York, New York 10017 (Address of principal executive offices) (zip code) (212) 733-2323 (Registrant’s telephone number, including area code) Securities registered pursuant to Section 12(b) of the Act: Title of each class Trading Symbol(s) Name of each exchange on which registered Common Stock, $.05 par value PFE New York Stock Exchange 0.000% Notes due 2020 PFE20A New York Stock Exchange 0.250% Notes due 2022 PFE22 New York Stock Exchange 1.000% Notes due 2027 PFE27 New York Stock Exchange Securities registered pursuant to Section 12(g) of the Act: None Indicate by check mark if the registrant is a well-known seasoned issuer, as defined in Rule 405 of the Securities Act. Yes ☒ No ☐ Indicate by check mark if the registrant is not required to file reports pursuant to Section 13 or Section 15(d) of the Act. Yes ☐ No ☒ Indicate by check mark whether the registrant (1) has filed all reports required to be filed by Section 13 or 15(d) of the Securities Exchange Act of 1934 during the preceding 12 months (or for such shorter period that the registrant was required to file such reports), and (2) has been subject to such filing requirements for the past 90 days. -

Patent Application Publication ( 10 ) Pub . No . : US 2019 / 0192440 A1
US 20190192440A1 (19 ) United States (12 ) Patent Application Publication ( 10) Pub . No. : US 2019 /0192440 A1 LI (43 ) Pub . Date : Jun . 27 , 2019 ( 54 ) ORAL DRUG DOSAGE FORM COMPRISING Publication Classification DRUG IN THE FORM OF NANOPARTICLES (51 ) Int . CI. A61K 9 / 20 (2006 .01 ) ( 71 ) Applicant: Triastek , Inc. , Nanjing ( CN ) A61K 9 /00 ( 2006 . 01) A61K 31/ 192 ( 2006 .01 ) (72 ) Inventor : Xiaoling LI , Dublin , CA (US ) A61K 9 / 24 ( 2006 .01 ) ( 52 ) U . S . CI. ( 21 ) Appl. No. : 16 /289 ,499 CPC . .. .. A61K 9 /2031 (2013 . 01 ) ; A61K 9 /0065 ( 22 ) Filed : Feb . 28 , 2019 (2013 .01 ) ; A61K 9 / 209 ( 2013 .01 ) ; A61K 9 /2027 ( 2013 .01 ) ; A61K 31/ 192 ( 2013. 01 ) ; Related U . S . Application Data A61K 9 /2072 ( 2013 .01 ) (63 ) Continuation of application No. 16 /028 ,305 , filed on Jul. 5 , 2018 , now Pat . No . 10 , 258 ,575 , which is a (57 ) ABSTRACT continuation of application No . 15 / 173 ,596 , filed on The present disclosure provides a stable solid pharmaceuti Jun . 3 , 2016 . cal dosage form for oral administration . The dosage form (60 ) Provisional application No . 62 /313 ,092 , filed on Mar. includes a substrate that forms at least one compartment and 24 , 2016 , provisional application No . 62 / 296 , 087 , a drug content loaded into the compartment. The dosage filed on Feb . 17 , 2016 , provisional application No . form is so designed that the active pharmaceutical ingredient 62 / 170, 645 , filed on Jun . 3 , 2015 . of the drug content is released in a controlled manner. Patent Application Publication Jun . 27 , 2019 Sheet 1 of 20 US 2019 /0192440 A1 FIG .