Ventricular Repolarization During Cardiovascular Autonomic Function Testing
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Prediction of Premature Termination Codon Suppressing Compounds for Treatment of Duchenne Muscular Dystrophy Using Machine Learning
Prediction of Premature Termination Codon Suppressing Compounds for Treatment of Duchenne Muscular Dystrophy using Machine Learning Kate Wang et al. Supplemental Table S1. Drugs selected by Pharmacophore-based, ML-based and DL- based search in the FDA-approved drugs database Pharmacophore WEKA TF 1-Palmitoyl-2-oleoyl-sn-glycero-3- 5-O-phosphono-alpha-D- (phospho-rac-(1-glycerol)) ribofuranosyl diphosphate Acarbose Amikacin Acetylcarnitine Acetarsol Arbutamine Acetylcholine Adenosine Aldehydo-N-Acetyl-D- Benserazide Acyclovir Glucosamine Bisoprolol Adefovir dipivoxil Alendronic acid Brivudine Alfentanil Alginic acid Cefamandole Alitretinoin alpha-Arbutin Cefdinir Azithromycin Amikacin Cefixime Balsalazide Amiloride Cefonicid Bethanechol Arbutin Ceforanide Bicalutamide Ascorbic acid calcium salt Cefotetan Calcium glubionate Auranofin Ceftibuten Cangrelor Azacitidine Ceftolozane Capecitabine Benserazide Cerivastatin Carbamoylcholine Besifloxacin Chlortetracycline Carisoprodol beta-L-fructofuranose Cilastatin Chlorobutanol Bictegravir Citicoline Cidofovir Bismuth subgallate Cladribine Clodronic acid Bleomycin Clarithromycin Colistimethate Bortezomib Clindamycin Cyclandelate Bromotheophylline Clofarabine Dexpanthenol Calcium threonate Cromoglicic acid Edoxudine Capecitabine Demeclocycline Elbasvir Capreomycin Diaminopropanol tetraacetic acid Erdosteine Carbidopa Diazolidinylurea Ethchlorvynol Carbocisteine Dibekacin Ethinamate Carboplatin Dinoprostone Famotidine Cefotetan Dipyridamole Fidaxomicin Chlormerodrin Doripenem Flavin adenine dinucleotide -

Supplementary Information D41586-018-05049-5
COMMENT Supplementary information to: When will clinical trials finally reflect diversity? To accompany a Comment published in Nature 557, 157–159 (2018) https://www.nature.com/articles/d41586-018-05049-5 by Todd C. Knepper & Howard L. McLeod SUPPLEMENTARY INFORMATION | NATURE | 1 Supplementary Tables Supplementary Table 1. List of drugs included in analysis Year Trade Name Non-Proprietary name Area Chemical Type Approved Gabitril tiagabine 1997 CNS 1 - New molecular entity (NME) Mirapex pramipexol 1997 CNS 1 - New molecular entity (NME) Requip ropinorole 1997 CNS 1 - New molecular entity (NME) Seroquel quetiapine 1997 CNS 1 - New molecular entity (NME) Zomig zolmitriptan 1997 CNS 1 - New molecular entity (NME) Apokyn apomorphine 2004 CNS 1 - New molecular entity (NME) Cymbalta duloxetine 2004 CNS 1 - New molecular entity (NME) Lunesta eszopiclone 2004 CNS 1 - New molecular entity (NME) Lyrica pregabalin 2004 CNS 1 - New molecular entity (NME) Prialt ziconotide 2004 CNS 1 - New molecular entity (NME) Tysabri natalizumab 2004 CNS BLA Fanapt ilioperidone 2009 CNS 1 - New molecular entity (NME) Saphris asenapine 2009 CNS 1 - New molecular entity (NME) Savella milnacipran 2009 CNS 1 - New molecular entity (NME) Amyvid florbetapir F 18 2012 CNS 1 - New molecular entity (NME) Aubagio teriflunomide 2012 CNS 1 - New molecular entity (NME) Fycompa perampanel 2012 CNS 1 - New molecular entity (NME) Belsomra suvarxant 2014 CNS 1 - New molecular entity (NME) Hetlioz tasimelteon 2014 CNS 1 - New molecular entity (NME) Movantik naloxegol 2014 CNS 1 -

Drugs Affectin the Autonomic Nervous System
Fundamentals of Medical Pharmacology Paterson Public Schools Written by Néstor Collazo, Ph.D. Jonathan Hodges, M.D. Tatiana Mikhaelovsky, M.D. for Health and Related Professions (H.A.R.P.) Academy March 2007 Course Description This fourth year course is designed to give students in the Health and Related Professions (H.A.R.P.) Academy a general and coherent explanation of the science of pharmacology in terms of its basic concepts and principles. Students will learn the properties and interactions between chemical agents (drugs) and living organisms for the rational and safe use of drugs in the control, prevention, and therapy of human disease. The emphasis will be on the fundamental concepts as they apply to the actions of most prototype drugs. In order to exemplify important underlying principles, many of the agents in current use will be singled out for fuller discussion. The course will include the following topics: ¾ The History of Pharmacology ¾ Terminology Used in Pharmacology ¾ Drug Action on Living Organisms ¾ Principles of Pharmacokinetics ¾ Dose-Response Relationships ¾ Time-Response Relationships ¾ Human Variability: Factors that will modify effects of drugs on individuals ¾ Effects of Drugs Attributable to Varying Modes of Administration ¾ Drug Toxicity ¾ Pharmacologic Aspects of Drug Abuse and Drug Dependence Pre-requisites Students must have completed successfully the following courses: Biology, Chemistry, Anatomy and Physiology, Algebra I and II Credits: 5 credits Basic Principles of Drug Action Introduction to Pharmacology a. Basic Mechanisms of Drug Actions b. Dose-response relationships c. Drug absorption d. Biotransformation of Drugs e. Pharmacokinetics f. Factors Affecting Drug Distribution g. Drug Allergy and Pharmacogenetics h. -

Pharmaceuticals As Environmental Contaminants
PharmaceuticalsPharmaceuticals asas EnvironmentalEnvironmental Contaminants:Contaminants: anan OverviewOverview ofof thethe ScienceScience Christian G. Daughton, Ph.D. Chief, Environmental Chemistry Branch Environmental Sciences Division National Exposure Research Laboratory Office of Research and Development Environmental Protection Agency Las Vegas, Nevada 89119 [email protected] Office of Research and Development National Exposure Research Laboratory, Environmental Sciences Division, Las Vegas, Nevada Why and how do drugs contaminate the environment? What might it all mean? How do we prevent it? Office of Research and Development National Exposure Research Laboratory, Environmental Sciences Division, Las Vegas, Nevada This talk presents only a cursory overview of some of the many science issues surrounding the topic of pharmaceuticals as environmental contaminants Office of Research and Development National Exposure Research Laboratory, Environmental Sciences Division, Las Vegas, Nevada A Clarification We sometimes loosely (but incorrectly) refer to drugs, medicines, medications, or pharmaceuticals as being the substances that contaminant the environment. The actual environmental contaminants, however, are the active pharmaceutical ingredients – APIs. These terms are all often used interchangeably Office of Research and Development National Exposure Research Laboratory, Environmental Sciences Division, Las Vegas, Nevada Office of Research and Development Available: http://www.epa.gov/nerlesd1/chemistry/pharma/image/drawing.pdfNational -

Cardiovascular System Drug Poster
Cardiovascular Drugs Created by the Njardarson Group (The University of Arizona): Edon Vitaku, Elizabeth A. Ilardi, Daniel J. Mack, Monica A. Fallon, Erik B. Gerlach, Miyant’e Y. Newton, Angela N. Yazzie, Jón T. Njarðarson Ethanol Glyceryl Trinitrate Anestisine Quinidine Procaine Adrenaline Adenosine Phenylepherine Heparin Vasoxyl Sotradecol Xylocaine Pronestyl Betamethasone Catapres Cedilanide Dopamine Inversine Metaraminol Acetyldigitoxin Hydrocortisone ( Ethanol ) ( Nitroglycerin ) ( Benzocaine ) ( Quinidine ) ( Procaine ) ( Epinephrine ) ( Adenosine ) ( Phenylephrine ) ( Heparin ) ( Methoxamine ) ( Sodium Tetradecyl Sulfate ) ( Lidocaine ) ( Procainamide ) ( Betamethasone ) ( Clonidine ) ( Deslanoside ) ( Dopamine ) ( Mecamylamine ) ( Metaraminol ) ( Acetyldigitoxin ) ( Hydrocortisone ) VASOPROTECTIVE CARDIAC THERAPY VASOPROTECTIVE CARDIAC THERAPY VASOPROTECTIVE CARDIAC THERAPY CARDIAC THERAPY CARDIAC THERAPY VASOPROTECTIVE CARDIAC THERAPY VASOPROTECTIVE CARDIAC THERAPY CARDIAC THERAPY VASOPROTECTIVE ANTIHYPERTENSIVE CARDIAC THERAPY CARDIAC THERAPY ANTIHYPERTENSIVE CARDIAC THERAPY CARDIAC THERAPY VASOPROTECTIVE Approved 1700s Approved 1879 Approved 1890s Approved 1900s Approved 1903 Approved 1920s Approved 1929 Approved 1930s Approved 1935 Approved 1940s Approved 1946 Approved 1949 Approved 1950 Approved 1950s Approved 1950s Approved 1950s Approved 1950s Approved 1950s Approved 1951 Approved 1952 Approved 1952 Regitine Phenoxybenzamine Serpasol Rescinnamine Diuril Harmonyl Naturetin Hydrochlorothiazide Hydrocortamate Fastin Ismel -

CPT / HCPCS Code Drug Description Approximate Cost Share
The information listed here is for our most prevalent plan. The amount you pay for a covered drug will depend on your plan’s coverage. Please refer to your Medical Plan GTB for more information. To find out the cost of your drugs, please contact HMSA Customer Service at 1-800-776-4672. If you receive services from a nonparticipating provider, you are responsible for a copayment plus any difference between the actual charge and the eligible charge. Legend $0 = no cost share $ = $100 and under $$ = over $100 to $250 $$$ = over $250 to $500 $$$$ = over $500 to $1000 $$$$$ = over $1000 1 = Please call HMSA Customer Service 1-800-776-4672 for cost share information. 2 = The cost share for this drug is dependent upon the diagnosis. Please call HMSA Customer Service at 1-800-772-4672 for more information. 3 = Cost share information for these drugs is dependent upon the dose prescribed. Please call HMSA Customer Service at 1- 800-772-4672 for more information. CPT / HCPCS approximate Code Drug Description cost share J0129 Abatacept Injection $$$$ J0130 Abciximab Injection 3 J0131 Acetaminophen Injection $ J0132 Acetylcysteine Injection $ J0133 Acyclovir Injection $ J0135 Adalimumab Injection $$$$ J0153 Adenosine Inj 1Mg $ J0171 Adrenalin Epinephrine Inject $ J0178 Aflibercept Injection $$$ J0180 Agalsidase Beta Injection 3 J0200 Alatrofloxacin Mesylate 3 J0205 Alglucerase Injection 3 J0207 Amifostine 3 J0210 Methyldopate Hcl Injection 3 J0215 Alefacept 3 J0220 Alglucosidase Alfa Injection 3 J0221 Lumizyme Injection 3 J0256 Alpha 1 Proteinase Inhibitor -

LD5655.V856 1994.D671.Pdf (7.787Mb)
Circulatory, Hormonal, and Metabolic Effects of Arbutamine Compared to Exercise in Persons With Known or Suspected Coronary Artery Disease by Karen Toft Dorn Dissertation submitted to the faculty of the Virginia Polytechnic Institute and State University in partial fulfillment of the requirements for the degree of DOCTOR OF PHILOSOPHY in Educational Research and Evaluation APPROVED: bia Pibadoode- Ne i It bf / hy C CVA G. Herbert, Chair immie C. Fortune F, C. Gwazdguskas Marion F. Ehrich J/ Edwin Wilder October, 1994 Blacksburg, VA ¢ 5655 / 656 944 Db 1 & Circulatory, Hormonal, and Metabolic Effects of Arbutamine Compared to Exercise in Persons With Known or Suspected Coronary Artery Disease by Karen LaVonne Toft Dorn Committee Chairman: William G. Herbert Exercise Science (ABSTRACT) The purpose of this study was to test the hypothesis that arbutamine, a specific B,-adrenergic agonist, will not cause different circulatory and physiologic effects than the less specific endogenous catecholamines released in response to an exercise stress test in persons with known or suspected coronary artery disease. Nine male subjects, mean age 66 years, completed symptom-limited arbutamine (ESA) and exercise (ETT) stress tests in a randomized cross-over study. The ESA delivery device controlled infusion rate to induce a graded heart rate increase of 8 bt'min’. Heart rate, systolic blood pressure, diastolic blood pressure, rate pressure product, ST segment shift, and specimens for epinephrine, norepinephrine, dopamine, cortisol, insulin, glucagon, glucose, free fatty acids, glycerol, and lactate were collected at baseline, immediate post-stress, and 10, 30, and 60 minutes post-stress. The research hypothesis was rejected. Repeated measures analysis of variance for each measure demonstrated a significant (p «< .05) time’treatment interaction in heart rate, systolic blood pressure, rate pressure product, insulin, glucagon, glycerol, free fatty acid, and lactate responses and a significant time effect for cortisol response. -

Federal Register / Vol. 60, No. 80 / Wednesday, April 26, 1995 / Notices DIX to the HTSUS—Continued
20558 Federal Register / Vol. 60, No. 80 / Wednesday, April 26, 1995 / Notices DEPARMENT OF THE TREASURY Services, U.S. Customs Service, 1301 TABLE 1.ÐPHARMACEUTICAL APPEN- Constitution Avenue NW, Washington, DIX TO THE HTSUSÐContinued Customs Service D.C. 20229 at (202) 927±1060. CAS No. Pharmaceutical [T.D. 95±33] Dated: April 14, 1995. 52±78±8 ..................... NORETHANDROLONE. A. W. Tennant, 52±86±8 ..................... HALOPERIDOL. Pharmaceutical Tables 1 and 3 of the Director, Office of Laboratories and Scientific 52±88±0 ..................... ATROPINE METHONITRATE. HTSUS 52±90±4 ..................... CYSTEINE. Services. 53±03±2 ..................... PREDNISONE. 53±06±5 ..................... CORTISONE. AGENCY: Customs Service, Department TABLE 1.ÐPHARMACEUTICAL 53±10±1 ..................... HYDROXYDIONE SODIUM SUCCI- of the Treasury. NATE. APPENDIX TO THE HTSUS 53±16±7 ..................... ESTRONE. ACTION: Listing of the products found in 53±18±9 ..................... BIETASERPINE. Table 1 and Table 3 of the CAS No. Pharmaceutical 53±19±0 ..................... MITOTANE. 53±31±6 ..................... MEDIBAZINE. Pharmaceutical Appendix to the N/A ............................. ACTAGARDIN. 53±33±8 ..................... PARAMETHASONE. Harmonized Tariff Schedule of the N/A ............................. ARDACIN. 53±34±9 ..................... FLUPREDNISOLONE. N/A ............................. BICIROMAB. 53±39±4 ..................... OXANDROLONE. United States of America in Chemical N/A ............................. CELUCLORAL. 53±43±0 -
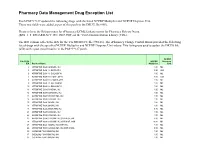
Pharmacy Data Management Drug Exception List
Pharmacy Data Management Drug Exception List Patch PSS*1*127 updated the following drugs with the listed NCPDP Multiplier and NCPDP Dispense Unit. These two fields were added as part of this patch to the DRUG file (#50). Please refer to the Release notes for ePharmacy/ECME Enhancements for Pharmacy Release Notes (BPS_1_5_EPHARMACY_RN_0907.PDF) on the VistA Documentation Library (VDL). The IEN column reflects the IEN for the VA PRODUCT file (#50.68). The ePharmacy Change Control Board provided the following list of drugs with the specified NCPDP Multiplier and NCPDP Dispense Unit values. This listing was used to update the DRUG file (#50) with a post install routine in the PSS*1*127 patch. NCPDP File 50.68 NCPDP Dispense IEN Product Name Multiplier Unit 2 ATROPINE SO4 0.4MG/ML INJ 1.00 ML 3 ATROPINE SO4 1% OINT,OPH 3.50 GM 6 ATROPINE SO4 1% SOLN,OPH 1.00 ML 7 ATROPINE SO4 0.5% OINT,OPH 3.50 GM 8 ATROPINE SO4 0.5% SOLN,OPH 1.00 ML 9 ATROPINE SO4 3% SOLN,OPH 1.00 ML 10 ATROPINE SO4 2% SOLN,OPH 1.00 ML 11 ATROPINE SO4 0.1MG/ML INJ 1.00 ML 12 ATROPINE SO4 0.05MG/ML INJ 1.00 ML 13 ATROPINE SO4 0.4MG/0.5ML INJ 1.00 ML 14 ATROPINE SO4 0.5MG/ML INJ 1.00 ML 15 ATROPINE SO4 1MG/ML INJ 1.00 ML 16 ATROPINE SO4 2MG/ML INJ 1.00 ML 18 ATROPINE SO4 2MG/0.7ML INJ 0.70 ML 21 ATROPINE SO4 0.3MG/ML INJ 1.00 ML 22 ATROPINE SO4 0.8MG/ML INJ 1.00 ML 23 ATROPINE SO4 0.1MG/ML INJ,SYRINGE,5ML 5.00 ML 24 ATROPINE SO4 0.1MG/ML INJ,SYRINGE,10ML 10.00 ML 25 ATROPINE SO4 1MG/ML INJ,AMP,1ML 1.00 ML 26 ATROPINE SO4 0.2MG/0.5ML INJ,AMP,0.5ML 0.50 ML 30 CODEINE PO4 30MG/ML -

2000 Dialysis of Drugs
2000 Dialysis of Drugs PROVIDED AS AN EDUCATIONAL SERVICE BY AMGEN INC. I 2000 DIAL Dialysis of Drugs YSIS OF DRUGS Curtis A. Johnson, PharmD Member, Board of Directors Nephrology Pharmacy Associates Ann Arbor, Michigan and Professor of Pharmacy and Medicine University of Wisconsin-Madison Madison, Wisconsin William D. Simmons, RPh Senior Clinical Pharmacist Department of Pharmacy University of Wisconsin Hospital and Clinics Madison, Wisconsin SEE DISCLAIMER REGARDING USE OF THIS POCKET BOOK DISCLAIMER—These Dialysis of Drugs guidelines are offered as a general summary of information for pharmacists and other medical professionals. Inappropriate administration of drugs may involve serious medical risks to the patient which can only be identified by medical professionals. Depending on the circumstances, the risks can be serious and can include severe injury, including death. These guidelines cannot identify medical risks specific to an individual patient or recommend patient treatment. These guidelines are not to be used as a substitute for professional training. The absence of typographical errors is not guaranteed. Use of these guidelines indicates acknowledgement that neither Nephrology Pharmacy Associates, Inc. nor Amgen Inc. will be responsible for any loss or injury, including death, sustained in connection with or as a result of the use of these guidelines. Readers should consult the complete information available in the package insert for each agent indicated before prescribing medications. Guides such as this one can only draw from information available as of the date of publication. Neither Nephrology Pharmacy Associates, Inc. nor Amgen Inc. is under any obligation to update information contained herein. Future medical advances or product information may affect or change the information provided. -

Administrative Records, Texas Department of Criminal Justice
Consistent with the terms of the Court’s May 22, 2017 scheduling order, the record has been redacted for all information that plaintiff, Texas Department of Criminal Justice (Texas), has identified as confidential. In addition, Defendants have also redacted information that the drug’s supplier and broker have separately advised the agency they consider confidential and private, as well as information the agency itself generally treats as confidential. This information has been redacted pending final FDA’s review of confidentiality claims, and our filing of the record with these redactions does not necessarily reflect our agreement with all of the claims of confidentiality Defendants have received. Defendants explicitly reserve the right to make an independent determination regarding the proper scope of redactions at a later time. Should we identify any of Texas’s redactions that are over-broad or otherwise improper, we will work with Texas’s counsel to revise the redactions in the record. MISCELLANEOUS FDA 568 DOCUMENT#: VERSION#: DIOP PROCEDURE ~L ORO-DIOP- 2.00 FOOD & DRUG ADMINISTRATION .008 I OFFICE OF REGULATORY AFFAIRS PAGE 1 OF 4 TITLE: EFFECTIVE DATE: PROCESSING OF SODIUM THIOPENTAL ENTRIES 4/16/2012 Sections included in this document 1. Purpose 2. Scope 3. Responsibility 4. Background 5. References 6. Procedure 7. Definitions/Glossary 8. Records 9. Supporting Documents 10. Contact Information 11.Attachments Document History and Change History 1. Purpose Pending litigation, this procedure provides instructions on the handling of shipments of Sodium Thiopental by Districts and the responsibility of DIOP in the processing of Sodium Thiopental entries. Districts should disseminate this information to all pertinent staff handling these entries. -

PHARMACEUTICAL APPENDIX to the HARMONIZED TARIFF SCHEDULE Harmonized Tariff Schedule of the United States (2008) (Rev
Harmonized Tariff Schedule of the United States (2008) (Rev. 1) Annotated for Statistical Reporting Purposes PHARMACEUTICAL APPENDIX TO THE HARMONIZED TARIFF SCHEDULE Harmonized Tariff Schedule of the United States (2008) (Rev. 1) Annotated for Statistical Reporting Purposes PHARMACEUTICAL APPENDIX TO THE TARIFF SCHEDULE 2 Table 1. This table enumerates products described by International Non-proprietary Names (INN) which shall be entered free of duty under general note 13 to the tariff schedule. The Chemical Abstracts Service (CAS) registry numbers also set forth in this table are included to assist in the identification of the products concerned. For purposes of the tariff schedule, any references to a product enumerated in this table includes such product by whatever name known. ABACAVIR 136470-78-5 ACIDUM GADOCOLETICUM 280776-87-6 ABAFUNGIN 129639-79-8 ACIDUM LIDADRONICUM 63132-38-7 ABAMECTIN 65195-55-3 ACIDUM SALCAPROZICUM 183990-46-7 ABANOQUIL 90402-40-7 ACIDUM SALCLOBUZICUM 387825-03-8 ABAPERIDONUM 183849-43-6 ACIFRAN 72420-38-3 ABARELIX 183552-38-7 ACIPIMOX 51037-30-0 ABATACEPTUM 332348-12-6 ACITAZANOLAST 114607-46-4 ABCIXIMAB 143653-53-6 ACITEMATE 101197-99-3 ABECARNIL 111841-85-1 ACITRETIN 55079-83-9 ABETIMUSUM 167362-48-3 ACIVICIN 42228-92-2 ABIRATERONE 154229-19-3 ACLANTATE 39633-62-0 ABITESARTAN 137882-98-5 ACLARUBICIN 57576-44-0 ABLUKAST 96566-25-5 ACLATONIUM NAPADISILATE 55077-30-0 ABRINEURINUM 178535-93-8 ACODAZOLE 79152-85-5 ABUNIDAZOLE 91017-58-2 ACOLBIFENUM 182167-02-8 ACADESINE 2627-69-2 ACONIAZIDE 13410-86-1 ACAMPROSATE