Tympanic Plate Fractures in Temporal Bone Trauma: Prevalence and Associated Injuries
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

The Incudomalleolar Articulation in Down Syndrome (Trisomy 21): a Temporal Bone Study
Zurich Open Repository and Archive University of Zurich Main Library Strickhofstrasse 39 CH-8057 Zurich www.zora.uzh.ch Year: 2015 The incudomalleolar articulation in down syndrome (trisomy 21): a temporal bone study Fausch, Christian ; Röösli, Christof Abstract: HYPOTHESIS: One reason for conductive hearing loss (HL) in patients with Down syndrome (DS) is structural anomalies in the incudomalleolar joint (IMJ) that impair sound transmission. BACK- GROUND: The majority of hearing losses in patients with DS are conductive. One reason is the high incidence of inflammatory processes such as otitis media. However, in some patients, the middle earseems to be normal. The assumption of structural disorders causing a HL is supported by a previous study revealing structural abnormalities of the incudostapedial joint (ISJ) in these patients. METHODS: In a retrospective analysis, histologic sections of the IMJ of 16 patients with DS were compared with 24 age- and sex-matched subjects with normal middle ear ossicles. The length of 8 parameters of the IMJ were measured at 3 positions and compared between the 2 groups. RESULTS: Age (p = 0.318) and sex distri- bution (p = 1) for the DS group and the matched controls were comparable. The IMJs (p < 0.001) and the cartilage of patients with DS are significantly wider in most measurements compared with controls. However, the joint space is not significantly different in the 2 groups. CONCLUSION: Conductive HL might be caused by a significantly wider IMJ in patients with DS supporting the findings of aprevious study reporting similar findings for the ISJ. The etiology of these findings is unclear. -

Redalyc.Deviant Facial Nerve Course in the Middle Ear Cavity
Brazilian Journal of Otorhinolaryngology ISSN: 1808-8694 [email protected] Associação Brasileira de Otorrinolaringologia e Cirurgia Cérvico- Facial Brasil Cho, Jungkyu; Choi, Nayeon; Hwa Hong, Sung; Moon, Il Joon Deviant facial nerve course in the middle ear cavity Brazilian Journal of Otorhinolaryngology, vol. 81, núm. 6, 2015, pp. 681-683 Associação Brasileira de Otorrinolaringologia e Cirurgia Cérvico-Facial São Paulo, Brasil Available in: http://www.redalyc.org/articulo.oa?id=392442695018 How to cite Complete issue Scientific Information System More information about this article Network of Scientific Journals from Latin America, the Caribbean, Spain and Portugal Journal's homepage in redalyc.org Non-profit academic project, developed under the open access initiative Document downloaded from http://bjorl.elsevier.es day 25/11/2015. This copy is for personal use. Any transmission of this document by any media or format is strictly prohibited. Braz J Otorhinolaryngol. 2015;81(6):681---683 Brazilian Journal of OTORHINOLARYNGOLOGY www.bjorl.org CASE REPORT ଝ Deviant facial nerve course in the middle ear cavity Trajeto anômalo do nervo facial na cavidade da orelha média ∗ Jungkyu Cho, Nayeon Choi, Sung Hwa Hong, Il Joon Moon Department of Otorhinolaryngology-Head and Neck Surgery, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Republic of Korea Received 27 December 2014; accepted 17 March 2015 Available online 7 September 2015 Introduction (Fig. 1A). Other physical exams showed no facial nerve palsy or auricular anomaly (Fig. 1B). Pure-tone average Anomalous facial nerve (FN) course can be found in a sig- (0.5, 1, 2, and 3 kHz) showed air-bone gap of 58 dB nificant number of cases with aural anomalies. -

Morfofunctional Structure of the Skull
N.L. Svintsytska V.H. Hryn Morfofunctional structure of the skull Study guide Poltava 2016 Ministry of Public Health of Ukraine Public Institution «Central Methodological Office for Higher Medical Education of MPH of Ukraine» Higher State Educational Establishment of Ukraine «Ukranian Medical Stomatological Academy» N.L. Svintsytska, V.H. Hryn Morfofunctional structure of the skull Study guide Poltava 2016 2 LBC 28.706 UDC 611.714/716 S 24 «Recommended by the Ministry of Health of Ukraine as textbook for English- speaking students of higher educational institutions of the MPH of Ukraine» (minutes of the meeting of the Commission for the organization of training and methodical literature for the persons enrolled in higher medical (pharmaceutical) educational establishments of postgraduate education MPH of Ukraine, from 02.06.2016 №2). Letter of the MPH of Ukraine of 11.07.2016 № 08.01-30/17321 Composed by: N.L. Svintsytska, Associate Professor at the Department of Human Anatomy of Higher State Educational Establishment of Ukraine «Ukrainian Medical Stomatological Academy», PhD in Medicine, Associate Professor V.H. Hryn, Associate Professor at the Department of Human Anatomy of Higher State Educational Establishment of Ukraine «Ukrainian Medical Stomatological Academy», PhD in Medicine, Associate Professor This textbook is intended for undergraduate, postgraduate students and continuing education of health care professionals in a variety of clinical disciplines (medicine, pediatrics, dentistry) as it includes the basic concepts of human anatomy of the skull in adults and newborns. Rewiewed by: O.M. Slobodian, Head of the Department of Anatomy, Topographic Anatomy and Operative Surgery of Higher State Educational Establishment of Ukraine «Bukovinian State Medical University», Doctor of Medical Sciences, Professor M.V. -
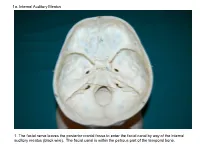
1A. Internal Auditory Meatus
1a. Internal Auditory Meatus 1. The facial nerve leaves the posterior cranial fossa to enter the facial canal by way of the internal auditory meatus (black wire). The facial canal is within the petrous part of the temporal bone. 1b. Internal Auditory Meatus The facial nerve leaves the posterior cranial fossa to enter the facial canal by way of the internal auditory meatus (black wire). 2. Hiatus of the Canal and Groove for the Greater Superficial Petrosal Nerve The greater superficial petrosal nerve leaves the facial canal to enter the middle cranial fossa by way of the hiatus of the canal for the greater superficial petrosal nerve (black wire). 3. Pterygoid Canal at Anterior Lip of the Lacerate Foramen The greater superficial petrosal nerve is joined by the deep petrosal nerve to form the nerve of the pterygoid canal (black and red wire). This nerve leaves the middle cranial fossa to enter the pterygopalatine fossa by way of the pterygoid canal. The posterior opening of the pterygoid canal is at the anterior lip of the lacerate foramen. The greater superficial nerve and the deep petrosal nerve travel within the cavernous sinus. 4. Pterygopalatine Fossa Seen Through the Pterygomaxillary Fissure The anterior opening of the pterygoid canal is into the pterygopalatine fossa (black wire). The pterygopalatine fossa is located medial to the pterygomaxillary fissure and contains the pterygopalatine ganglion. 5. External Auditory Meatus The chorda tympani nerve leaves the facial canal and crosses the middle ear (black wire). It then leaves the middle ear to arrive in the infratemporal fossa by way of the petrotympanic fissure. -

Doctoral Dissertation Template
UNIVERSITY OF OKLAHOMA GRADUATE COLLEGE MECHANICAL PROPERTIES OF HUMAN INCUDOSTAPEDIAL JOINT AND TYMPANIC MEMBRANE IN NORMAL AND BLAST-DAMAGED EARS A DISSERTATION SUBMITTED TO THE GRADUATE FACULTY in partial fulfillment of the requirements for the Degree of DOCTOR OF PHILOSOPHY By SHANGYUAN JIANG Norman, Oklahoma 2018 MECHANICAL PROPERTIES OF HUMAN INCUDOSTAPEDIAL JOINT AND TYMPANIC MEMBRANE IN NORMAL AND BLAST-DAMAGED EARS A DISSERTATION APPROVED FOR THE STEPHENSON SCHOOL OF BIOMEDICAL ENGINEERING BY ______________________________ Dr. Rong Z. Gan, Chair ______________________________ Dr. Vassilios I. Sikavitsas ______________________________ Dr. Matthias U. Nollert ______________________________ Dr. Edgar A. O’Rear ______________________________ Dr. Harold L. Stalford © Copyright by SHANGYUAN JIANG 2018 All Rights Reserved. I dedicate my dissertation work to my family. Acknowledgements I would like to express my sincere appreciation to my advisor, Dr. Rong Z. Gan for the enormous amount time, energy, resource, and patience she had devoted in my training process. I joined the Ph.D. program at the University of Oklahoma right after I got my bachelor degree and with great language difficulties. Dr. Gan has been teaching me how to think, read, learn and write as a researcher regardless of my weak background since the first day I arrived in the US. Her respect, enthusiasm, and persistence to work has deeply impressed me and changed my attitude towards my work and life. The past five years in the biomedical engineering laboratory is one of the most precious experiences in my life. I would like to express my appreciation to my committee members, Dr. Vassilios I. Sikavitsas, Dr. Matthias U. Nollert, Dr. Edgar A. -

Treatment of a Traumatic Incudomalleolar Joint Subluxation with Hydroxyapatite Bone Cement Dennis Bojrab II 1, Jennifer F Ha2,3,4,5*, David a Zopf 1
Annals of International Case Report Case Report Open Access | Research Treatment of A Traumatic Incudomalleolar Joint Subluxation with Hydroxyapatite Bone Cement Dennis Bojrab II 1, Jennifer F Ha2,3,4,5*, David A Zopf 1 1Department of Paediatrics Otolaryngology Head & Neck Surgery, University of Michigan Health System, C.S. Mott Children’s Hospital, 1540 East Hospital Drive, Ann Arbor, Michigan 48109, United States of America 2Department of Paediatrics Otolaryngology Head & Neck Surgery, Perth Children’s Hospital, Roberts Road, Nedlands 6009, Western Australia 3Murdoch ENT, Wexford Medical Centre, St John of God Hospital (Murdoch), Suite 17-18, Level 1, 3 Barry Marshall Parade, Murdoch 6150, West- ern Australia 4School of Surgery, University of Western Australia, Stirling Highway, Crawley 6009, Western Australia 5 St John of God Hospital (Murdoch), Wexford Medical Centre, Suite 17-18, Level 1, 3 Barry Marshall Parade, Murdoch 6150, Western Australia Abstract Trauma-related hearing loss can be conductive, sensorineural, or mixed in nature. Alteration of any of the conductive mechanisms can result in a conductive hearing loss. Depending on the location and type of ossicular injury there several reconstructive options have been described. Hydroxyapetite cement has been reported on several occasions for incudostapedial dislocation, however, rare- ly/never for incudomalleolar dislocation. Here we report a patient with traumatic Incudomalleolar Joint (IMJ) separation which was successfully repaired using bone cement. Case Description A 15-year-old male patient was referred to our Paediatric Otolaryngology department by his paediatrician with a lifelong history of left sided hearing loss. He was involved in two motor vehicle accidents when he was younger. -

Dissection and Exposure of the Whole Course of Deep Nerves in Human Head Specimens After Decalcification
Hindawi Publishing Corporation International Journal of Otolaryngology Volume 2012, Article ID 418650, 7 pages doi:10.1155/2012/418650 Research Article Dissection and Exposure of the Whole Course of Deep Nerves in Human Head Specimens after Decalcification Longping Liu, Robin Arnold, and Marcus Robinson Discipline of Anatomy and Histology, University of Sydney, Anderson Stuart Building F13, Sydney, NSW 2006, Australia Correspondence should be addressed to Marcus Robinson, [email protected] Received 29 July 2011; Revised 10 November 2011; Accepted 12 December 2011 AcademicEditor:R.L.Doty Copyright © 2012 Longping Liu et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited. The whole course of the chorda tympani nerve, nerve of pterygoid canal, and facial nerves and their relationships with surrounding structures are complex. After reviewing the literature, it was found that details of the whole course of these deep nerves are rarely reported and specimens displaying these nerves are rarely seen in the dissecting room, anatomical museum, or atlases. Dissections were performed on 16 decalcified human head specimens, exposing the chorda tympani and the nerve connection between the geniculate and pterygopalatine ganglia. Measurements of nerve lengths, branching distances, and ganglia size were taken. The chorda tympani is a very fine nerve (0.44 mm in diameter within the tympanic cavity) and approximately 54 mm in length. The mean length of the facial nerve from opening of internal acoustic meatus to stylomastoid foramen was 52.5 mm. -

Os Temporale (Halántékcsont)
CRANIOFACIAL AND MAXILLOFACIAL ASPECTS OF THE SKULL PhD., Dr. Dávid Lendvai / Dr. Gábor Baksa Semmelweis University Anatomy, Histology and Embryogy Institute Budapest 2018 MAIN PARTS OF THE SKULL •Constitute by 22 bones: •neurocranium (8) – UNPAIRED: frontal, occipital, sphenoid, ethmoid bones PAIRED: temporal, parietal bones •viscerocranium (14) -UNPAIRED: mandibule, vomer. PAIRED: nasal, maxilla, zygomatic, lacrimal, palatine, inferior nasal concha Their role – formation of cavities, protect viscera, voice formation, initial portions of the gastrointerstinal and respiratory systems, insertion of muscles (mascication, head movements) Cavities: - Cranial cavity, - Nasal cavity, - Paranasal sinuses - Oral cavity, - Orbit, - (Tympanic cavity, Inner ear) Cranium cerebrale 1. calvaria 2. Skull base: •Basis cranii int. •Basis cranii ext. Protub. occip. ext. → linea nuchae sup. → beginning of the linea temp. → zygomatic arch → infratemp. crest → ala major → zygomatic process → supraorbital margin → nasofrontalis suture External skull base Braus Internal skull base Braus Why do we need the neuroanatomy? Picture: Peter Claesz – Vanitas (still-life, 1630.) www.hydrocephalus.inf o ? www.totalhealth.co.u k Aesculap - B Braun Todoro w Physiologically volume and pressure are balanced within the skull A minimally disturbed balance can be already compensated Over the normal range of this compensation ability minimal changes in the volume lead to a disproportionally high elevation of intracranial pressure (ICP) (for further see in physiology the Monroe -

Imaging of Temporal Bone Trauma
Imaging of Temporal Bone Trauma Tabassum A. Kennedy, MD*, Gregory D. Avey, MD, Lindell R. Gentry, MD KEYWORDS Temporal bone fracture Trauma Ossicular injury Hearing loss Facial nerve Cerebrospinal fluid leak Pneumolabyrinth Perilymphatic fistula KEY POINTS Multidetector temporal bone computed tomography examinations should be performed in patients with a clinical or radiographic suspicion of temporal bone fracture. Categorization of temporal bone fractures should include a descriptor for fracture direction, the presence or absence of labyrinthine involvement, and the segment of temporal bone involved. It is important to identify associated complications related to temporal bone trauma that will guide management. Complications include injury to the tympanic membrane, ossicular chain, vestibulo- cochlear apparatus, facial nerve, tegmen, carotid canal, and venous system. INTRODUCTION evaluation with a noncontrast CT examination of the head. Careful scrutiny of the temporal bone The temporal bone is at risk for injury in the setting on head CT is necessary to detect primary and of high-impact craniofacial trauma occurring in 3% secondary signs of temporal bone injury. External to 22% of patients with trauma with skull fractures 1–3 auditory canal opacification, otomastoid opacifi- (Table 1). Motor vehicle collisions, assaults, cation, air within the temporomandibular joint, and falls are the most common mechanisms of 4–6 ectopic intracranial air adjacent to the temporal injury. Most patients with temporal bone trauma bone, and pneumolabyrinth in the setting of sustain unilateral injury, occurring in 80% to 90% 5,7,8 trauma should raise the suspicion of an associated of cases. Multidetector computed tomography temporal bone fracture (Fig. 1). Patients with (CT) has revolutionized the ability to evaluate the temporal bone trauma often sustain concomitant intricate anatomy of the temporal bone, enabling intracranial injury, which often necessitates more clinicians to detect fractures and complications emergent management. -

Necrosis of the Long Process of the Incus Following Stapes Surgery: New Anatomical Observations
The Laryngoscope VC 2009 The American Laryngological, Rhinological and Otological Society, Inc. Necrosis of the Long Process of the Incus Following Stapes Surgery: New Anatomical Observations Imre Gerlinger, MD, PhD; Miklo´sTo´th, MD, PhD; La´szlo´ Lujber, MD, PhD; Istva´n Szanyi, MD; Pe´ter Mo´ricz, MD; Krisztina Somogyva´ri, MD; Adrienn Ne´meth, MD; Ga´bor Ra´th, MD; Jo´zsef Pytel, MD, PhD; Wolfgang Mann, MD, PhD, FACS Objectives/Hypothesis: The most frequent incudes revealed 1-4 nutritive foramina on the long complication (generally recognized during revision processes of 48% (24) of the left-sided incudes and procedures) following seemingly successful stapedoto- 56% (28) of the right-sided incudes. The positions of mies and stapedectomies is necrosis of the long pro- these foramina differed, however, from those previ- cess of the incus. This is currently ascribed to a mal- ously described in the literature. They were mostly crimped stapes prosthesis or to a compromised blood located not on the medial side of the incus body or on supply of the incus. The two-point fixation can cause the short process or on the cranial third of the long a mucosal injury with a resulting toxic reaction, and processes, but antero-medially, mostly on the middle also osteoclastic activity. An important aspect in the or cranial third. In 48% of all the incudes examined, engineering of ideal stapes prostheses is that they an obvious foramen was not observed either in the should be fixed circularly to the long process of the body or in the long process of the incus. -

Ossiculoplasty for Malleus Bar with Incudostapedial Disconnection and Fused Incudomalleolar Joint
Hindawi Case Reports in Otolaryngology Volume 2020, Article ID 8828969, 4 pages https://doi.org/10.1155/2020/8828969 Case Report Ossiculoplasty for Malleus Bar with Incudostapedial Disconnection and Fused Incudomalleolar Joint Yuji Kanazawa , Hitomi Matsuura, Natsumi Aiso, and Masako Nakai Department of Otolaryngology, Shiga Medical Center for Children, 5-7-30 Moriyama, Moriyama City 524-0022, Japan Correspondence should be addressed to Yuji Kanazawa; [email protected] Received 3 April 2020; Revised 22 June 2020; Accepted 4 July 2020; Published 23 July 2020 Academic Editor: Nicola´s Pe´rez Ferna´ndez Copyright © 2020 Yuji Kanazawa et al. .is is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited. Malleus bar is an abnormal bony connection between the malleus handle and the posterior wall of the tympanic cavity. We report a patient with a malleus bar and another malformation of the ossicles. An 11-year-old boy presented with hearing impairment since early childhood. Computed tomography (CT) revealed a malleus bar with an incudostapedial disconnection in the right ear. At tympanoplasty, the malleus bar was first identified and removed. A fused malleus-incus, not visible on the preoperative CT, was found intraoperatively. .erefore, the fused malleus-incus was removed; then, the ossicular chain was reconstructed, resulting in an improved postoperative hearing level. On preoperative CT, the disconnected incudostapedial joint had been identified, whereas the fused malleus-incus had not. Given the variations in the malleus bar anomaly of the middle ear, the surgical procedure for ossiculoplasty should be adapted intraoperatively based on any findings not visible on the preoperative CT. -

Inferior View of Skull
human anatomy 2016 lecture sixth Dr meethak ali ahmed neurosurgeon Inferior View Of Skull the anterior part of this aspect of skull is seen to be formed by the hard palate.The palatal process of the maxilla and horizontal plate of the palatine bones can be identified . in the midline anteriorly is the incisive fossa & foramen . posterolaterlly are greater & lesser palatine foramena. Above the posterior edge of the hard palate are the choanae(posterior nasal apertures ) . these are separated from each other by the posterior margin of the vomer & bounded laterally by the medial pterygoid plate of sphenoid bone . the inferior end of the medial pterygoid plate is prolonged as a curved spike of bone , the pterygoid hamulus. the superior end widens to form the scaphoid fossa . posterolateral to the lateral pterygoid plate the greater wing of the sphenoid is pieced by the large foramen ovale & small foramen spinosum . posterolateral to the foramen spinosum is spine of the sphenoid . Above the medial border of the scaphoid fossa , the sphenoid bone is pierced by pterygoid canal . Behind the spine of the sphenoid , in the interval between the greater wing of the sphenoid and the petrous part of the temporal bone , there is agroove for the cartilaginous part of the auditory tube. The opening of the bony part of the tube can be identified. The mandibular fossa of the temporal bone & the articular tubercle form the upper articular surfaces for the temporomandibular joint . separating the mandibular fossa from the tympanic plate posteriorly is the squamotympanic fissure, through the medial end of which (petrotympanic fissure ) the chorda tympani exits from the tympanic cavity .The styloid process of the temporal bone projects downward & forward from its inferior aspect.