Growth Hormone (Hgh, Somatropin) Therapy
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
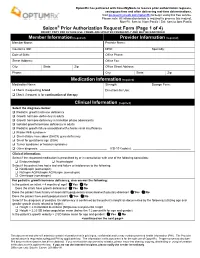
Saizen Prior Authorization Request Form (Page 1 of 4) DO NOT COPY for FUTURE USE
OptumRx has partnered with CoverMyMeds to receive prior authorization requests, saving you time and often delivering real-time determinations. Visit go.covermymeds.com/OptumRx to begin using this free service. Please note: All information below is required to process this request. Mon-Fri: 5am to 10pm Pacific / Sat: 6am to 3pm Pacific ® Saizen Prior Authorization Request Form (Page 1 of 4) DO NOT COPY FOR FUTURE USE. FORMS ARE UPDATED FREQUENTLY AND MAY BE BARCODED Member Information (required) Provider Information (required) Member Name: Provider Name: Insurance ID#: NPI#: Specialty: Date of Birth: Office Phone: Street Address: Office Fax: City: State: Zip: Office Street Address: Phone: City: State: Zip: Medication Information (required) Medication Name: Strength: Dosage Form: Check if requesting brand Directions for Use: Check if request is for continuation of therapy Clinical Information (required) Select the diagnosis below: Pediatric growth hormone deficiency Growth hormone deficiency in adults Growth hormone deficiency in transition phase adolescents Isolated growth hormone deficiency in adults Pediatric growth failure associated with chronic renal insufficiency Prader-Willi syndrome Short-stature homeobox (SHOX) gene deficiency Small for gestational age (SGA) Turner syndrome or Noonan syndrome Other diagnosis: _________________________________________ ICD-10 Code(s): ___________________________________ Clinical Information: Select if the requested medication is prescribed by or in consultation with one of the following -

September 2017 ~ Resource #330909
−This Clinical Resource gives subscribers additional insight related to the Recommendations published in− September 2017 ~ Resource #330909 Medications Stored in the Refrigerator (Information below comes from current U.S. and Canadian product labeling and is current as of date of publication) Proper medication storage is important to ensure medication shelf life until the manufacturer expiration date and to reduce waste. Many meds are recommended to be stored at controlled-room temperature. However, several meds require storage in the refrigerator or freezer to ensure stability. See our toolbox, Medication Storage: Maintaining the Cold Chain, for helpful storage tips and other resources. Though most meds requiring storage at temperatures colder than room temperature should be stored in the refrigerator, expect to see a few meds require storage in the freezer. Some examples of medications requiring frozen storage conditions include: anthrax immune globulin (Anthrasil [U.S. only]), carmustine wafer (Gliadel [U.S. only]), cholera (live) vaccine (Vaxchora), dinoprostone vaginal insert (Cervidil), dinoprostone vaginal suppository (Prostin E2 [U.S.]), varicella vaccine (Varivax [U.S.]; Varivax III [Canada] can be stored in the refrigerator or freezer), zoster vaccine (Zostavax [U.S.]; Zostavax II [Canada] can be stored in the refrigerator or freezer). Use the list below to help identify medications requiring refrigerator storage and become familiar with acceptable temperature excursions from recommended storage conditions. Abbreviations: RT = room temperature Abaloparatide (Tymlos [U.S.]) Aflibercept (Eylea) Amphotericin B (Abelcet, Fungizone) • Once open, may store at RT (68°F to 77°F • May store at RT (77°F [25°C]) for up to Anakinra (Kineret) [20°C to 25°C]) for up to 30 days. -

ANONYMOUS V MERCK SERONO Conduct of Representative
CASE AUTH/2591/3/13 ANONYMOUS v MERCK SERONO Conduct of representative An anonymous, non-contactable complainant, An anonymous, non-contactable complainant, complained about the conduct of an un-named complained about the conduct of an un-named representative from Merck Serono who had representative from Merck Serono. requested a monthly visit throughout 2013. The complainant stated that he/she felt harassed as COMPLAINT such frequent meetings were unnecessary. The complainant was informed that these visits were The complainant was concerned about a meeting required to meet an instruction to have meetings that he/she had had with a Merck Serono with seven health professionals each day. representative. The complainant alleged that the representative had requested that he/she plan a The complainant noted that before this episode, monthly visit with him/her throughout 2013. The he/she had always found the representative to be complainant stated that he/she felt harassed by this very professional and an asset to the company. The request as such frequent meetings were completely complainant considered that the representatives unnecessary. When the complainant asked why the were being forced to behave in this way by representative wanted to plan so many meetings in unrealistic expectations from their managers. advance he/she was informed that these visits were required to meet an instruction to have meetings The detailed response from Merck Serono is given with seven health professionals each day. below. The complainant noted that before this episode, he/ The Panel noted that Merck Serono’s instructions to she had always found this representative to be very its representatives referred to a number of different professional and an asset to his/her company. -

GROWTH HORMONE (Adult Therapy) Genotropin, Humatrope, Norditropin, Nutropin, Nutropin AQ, Omnitrope, Saizen, Sogroya*, Zomacton
GROWTH HORMONE (Adult therapy) Genotropin, Humatrope, Norditropin, Nutropin, Nutropin AQ, Omnitrope, Saizen, Sogroya*, Zomacton Bolded medications are the preferred products *This medication is included in this policy but is not available in the market as of yet RATIONALE FOR INCLUSION IN PA PROGRAM Background Growth hormone deficiency (GHD) in adulthood, associated with hypothalamic-pituitary dysfunction is now widely accepted as a distinct clinical syndrome, and is linked to a substantial number of significant co-morbidities, many of which can be ameliorated with growth hormone replacement therapy (1). The FDA has approved growth hormone replacement for use in adult patients with growth hormone deficiency. Approved indications are for the treatment of adults with either adult onset or childhood onset GHD. With the exception of idiopathic adult onset GHD, GHD should be confirmed as due to pituitary disease from known causes, including pituitary tumor, pituitary surgical damage, hypothalamic disease, irradiation, trauma, or reconfirmed childhood GHD. Growth hormone should only be prescribed to patients with clinical features suggestive of adult GHD and biochemically proven evidence of adult GHD (1-9). Regulatory Status FDA approved indications: Human growth hormone is indicated for treatment of adult patients with either childhood-onset or adult-onset GH deficiency (2-9). The laboratory diagnosis of GHD in adults is determined by dynamic endocrine testing. Because growth hormone has a short half-life in blood growth hormone levels frequently are undetectable in blood samples obtained at random from normal subjects. For this reason, a stimulation test is needed to confirm the diagnosis. American Association of Clinical Endocrinologists (AACE) does not recommend growth hormone stimulation testing in patients with three or more pituitary hormone deficiencies and low IGF1 (2-9). -

Specialty Guideline Management
Reference number(s) 1741-A SPECIALTY GUIDELINE MANAGEMENT GENOTROPIN (somatropin) HUMATROPE (somatropin) NORDITROPIN (somatropin) NUTROPIN AQ (somatropin) OMNITROPE (somatropin) SAIZEN (somatropin) ZOMACTON (somatropin) POLICY I. INDICATIONS The indications below including FDA-approved indications and compendial uses are considered a covered benefit provided that all the approval criteria are met and the member has no contraindications or exclusions to the prescribed therapy. A. FDA-Approved Indications 1. Pediatric patients with growth failure due to any of the following: a. Growth hormone (GH) deficiency b. Turner syndrome c. Noonan syndrome d. Small for gestational age (SGA) e. Prader-Willi syndrome f. Chronic kidney disease (CKD) g. Short stature homeobox-containing gene (SHOX) deficiency h. Idiopathic short stature (ISS)* 2. Adults with childhood-onset or adult-onset GH deficiency * ISS may not be covered by some plans B. Compendial Uses 1. Human immunodeficiency virus (HIV)-associated wasting/cachexia 2. Short bowel syndrome (SBS) 3. Growth failure associated with any of the following: a. Cerebral palsy b. Congenital adrenal hyperplasia c. Cystic fibrosis d. Russell-Silver syndrome All other indications are considered experimental/investigational and not medically necessary. II. REQUIRED DOCUMENTATION The following information is necessary to initiate the prior authorization review for both initial and continuation of therapy requests (where applicable): A. Medical records supporting the diagnosis of neonatal GH deficiency Growth Hormone With ISS 1741-A SGM P2021.docx © 2021 CVS Caremark. All rights reserved. This document contains confidential and proprietary information of CVS Caremark and cannot be reproduced, distributed or printed without written permission from CVS Caremark. This document contains prescription brand name drugs that are trademarks or registered trademarks of pharmaceutical manufacturers that are not affiliated with CVS Caremark. -

Medicines/Pharmaceuticals of Animal Origin V3.0 November 2020
Medicines/pharmaceuticals of animal origin V3.0 November 2020 Medicines/pharmaceuticals of animal origin - This guideline provides information for all clinical staff within Hospital and Health Services (HHS) on best practice for avoidance of issues related to animal products. Medicines/pharmaceuticals of animal origin - V3.0 November 2020 Published by the State of Queensland (Queensland Health), November 2020 This document is licensed under a Creative Commons Attribution 3.0 Australia licence. To view a copy of this licence, visit creativecommons.org/licenses/by/3.0/au © State of Queensland (Queensland Health) 2020 You are free to copy, communicate and adapt the work, as long as you attribute the State of Queensland (Queensland Health). For more information contact: Medication Services Queensland, Queensland Health, GPO Box 48, Brisbane QLD 4001, email [email protected] An electronic version of this document is available at https://www.health.qld.gov.au/__data/assets/pdf_file/0024/147507/qh-gdl-954.pdf Disclaimer: The content presented in this publication is distributed by the Queensland Government as an information source only. The State of Queensland makes no statements, representations or warranties about the accuracy, completeness or reliability of any information contained in this publication. The State of Queensland disclaims all responsibility and all liability (including without limitation for liability in negligence) for all expenses, losses, damages and costs you might incur as a result of the information being inaccurate -

Saizen Prescribing Information
HIGHLIGHTS OF PRESCRIBING INFORMATION ___________ WARNINGS AND PRECAUTIONS ___________ These highlights do not include all the information needed to use • Acute Critical Illness: Potential benefit of treatment continuation SAIZEN® safely and effectively. See full prescribing information should be weighed against the potential risk (5.1) for SAIZEN. • Prader-Willi syndrome in Children: Evaluate for signs of upper airway obstruction and sleep apnea before initiation of SAIZEN (somatropin) for injection, for subcutaneous use treatment. Discontinue treatment if these signs occur (5.2) Initial U.S. Approval: 1987 • Neoplasms: Monitor patients with preexisting tumors for progression or recurrence. Increased risk of a second neoplasm ______________ ______________ in childhood cancer survivors treated with somatropin—in INDICATIONS AND USAGE particular meningiomas as in patients treated with radiation to SAIZEN is a recombinant human growth hormone indicated for: the head for their first neoplasm (5.3) Pediatric: Treatment of children with growth failure due to growth • Impaired Glucose Tolerance and Diabetes Mellitus: May be hormone deficiency (GHD) (1.1) unmasked. Periodically monitor glucose levels in all patients Adult: Treatment of adults with either adult onset or childhood onset Doses of concurrent antihyperglycemic drugs in diabetics may GHD. (1.2) require adjustment (5.4) • Intracranial Hypertension: Exclude preexisting papilledema. ___________ DOSAGE AND ADMINISTRATION ___________ May develop and is usually reversible after discontinuation -

Growth Hormones Is Recommended in Those Who Meet the Following Criteria
Policy: 95015 Initial Effective Date: 06/22/1995 HCPCS J2170, J2940, J2941 and Q0515 Code(s): Annual Review Date: 06/17/2021 SUBJECT: Growth Stimulating Drugs Last Revised Date: 07/15/2021 - Genotropin(somatropin injection) - Humatrope (somatropin injection) - Increlex (mecasermin) - Norditropin® (somatropin injection) - Nutropin AQ (somatropin injection) - Omnitrope® (somatropin injection) - Saizen® (somatropin injection) - Serostim (somatropin injection) - Zomacton™ (somatropin injection) - Zorbtive (somatropin injection) - Sogroya(somapacitan injection) Prior approval is required for some or all procedure codes listed in this Corporate Drug Policy. Definition: Exogenous growth hormone (recombinant human, rhGH) is a polypeptide hormone with metabolic effects similar to endogenous human growth hormone (GH). Produced in the pituitary gland, endogenous growth hormone activates production of insulin-like growth factor-1 (IGF-1) and other peptides that: modulate lipid, carbohydrate and protein metabolism; and stimulate development of bone, cartilage, skeletal muscle and gonadal tissue, leading to longitudinal growth. Inadequate secretion or impairment of growth hormone activity during childhood and adolescence may result in short stature, growth hormone deficiency with growth failure and other medical conditions. Exogenous growth hormone products approved by the U.S. Food and Drug Administration include somatropin (Humatrope®, Nutropin®, Serostim®, Saizen®, Norditropin®, Genotropin®, Zorbtive®, Omnitrope®, ZomactonTM). These products are -
![Saizen® [Somatropin (Rdna Origin) for Injection] for Subcutaneous Or Intramuscular Injection](https://docslib.b-cdn.net/cover/3500/saizen%C2%AE-somatropin-rdna-origin-for-injection-for-subcutaneous-or-intramuscular-injection-2653500.webp)
Saizen® [Somatropin (Rdna Origin) for Injection] for Subcutaneous Or Intramuscular Injection
Saizen® [somatropin (rDNA origin) for injection] For subcutaneous or intramuscular injection DESCRIPTION Saizen® [somatropin (rDNA origin) for injection] is a human growth hormone produced by recombinant DNA technology. Saizen® has 191 amino acid residues and a molecular weight of 22,125 daltons. Its amino acid sequence and structure are identical to the dominant form of human pituitary growth hormone. Saizen® is produced by a mammalian cell line (mouse C127) that has been modified by the addition of the human growth hormone gene. Saizen®, with the correct three-dimensional configuration, is secreted directly through the cell membrane into the cell-culture medium for collection and purification. Saizen® is a highly purified preparation. Biological potency is determined by measuring the increase in body weight induced in hypophysectomized rats. Saizen® is a sterile, non-pyrogenic, white, lyophilized powder intended for subcutaneous or intramuscular injection after reconstitution with Bacteriostatic Water for Injection, USP (0.9% Benzyl Alcohol). The reconstituted solution has a pH of 6.5 to 8.5. Saizen® is available in 5 mg and 8.8 mg vials. The quantitative composition per vial is: 5 mg (approximately 15 IU) vial: Each vial contains 5.0 mg somatropin (approximately 15 IU), 34.2 mg sucrose and 1.16 mg O-phosphoric acid. The pH is adjusted with sodium hydroxide or O- phosphoric acid. 8.8 mg (approximately 26.4 IU) vial: Each vial contains 8.8 mg somatropin (approximately 26.4 IU), 60.2 mg sucrose and 2.05 mg O-phosphoric acid. The pH is adjusted with sodium hydroxide or O- phosphoric acid. -
![SAIZEN® [Somatropin (Rdna Origin) for Injection], NDA 19-764/S-020 DRAFT PACKAGE INSERT: Adult Growth Hormone Deficiency (Submitted 10.26.04)](https://docslib.b-cdn.net/cover/2241/saizen%C2%AE-somatropin-rdna-origin-for-injection-nda-19-764-s-020-draft-package-insert-adult-growth-hormone-deficiency-submitted-10-26-04-2972241.webp)
SAIZEN® [Somatropin (Rdna Origin) for Injection], NDA 19-764/S-020 DRAFT PACKAGE INSERT: Adult Growth Hormone Deficiency (Submitted 10.26.04)
SAIZEN® [somatropin (rDNA origin) for injection], NDA 19-764/S-020 DRAFT PACKAGE INSERT: Adult Growth Hormone Deficiency (Submitted 10.26.04) Saizen® [somatropin (rDNA origin) for injection] For subcutaneous or intramuscular injection DESCRIPTION Saizen® [somatropin (rDNA origin) for injection] is a human growth hormone produced by recombinant DNA technology. Saizen® has 191 amino acid residues and a molecular weight of 22,125 daltons. Its amino acid sequence and structure are identical to the dominant form of human pituitary growth hormone. Saizen® is produced by a mammalian cell line (mouse C127) that has been modified by the addition of the human growth hormone gene. Saizen®, with the correct three-dimensional configuration, is secreted directly through the cell membrane into the cell-culture medium for collection and purification. Saizen® is a highly purified preparation. Biological potency is determined by measuring the increase in body weight induced in hypophysectomized rats. Saizen® is a sterile, non-pyrogenic, white, lyophilized powder intended for subcutaneous or intramuscular injection after reconstitution with Bacteriostatic Water for Injection, USP (0.9% Benzyl Alcohol). The reconstituted solution has a pH of 6.5 to 8.5. Saizen® is available in 5 mg and 8.8 mg vials. The quantitative composition per vial is: 5 mg (approximately 15 IU) vial: Each vial contains 5.0 mg somatropin (approximately 15 IU), 34.2 mg sucrose and 1.16 mg O-phosphoric acid. The pH is adjusted with sodium hydroxide or O- phosphoric acid. 8.8 mg (approximately 26.4 IU) vial: Each vial contains 8.8 mg somatropin (approximately 26.4 IU), 60.2 mg sucrose and 2.05 mg O-phosphoric acid. -

Formulary Drug List
ABALOPARATIDE Products Affected • TYMLOS PA Criteria Criteria Details Exclusion PATIENT HAS RECEIVED A TOTAL OF 24 MONTHS Criteria CUMULATIVE TREATMENT WITH ANY PARATHYROID HORMONE THERAPY. Required Medical Information Age Restrictions Prescriber Restrictions Coverage 12 MONTHS Duration 1 PA Criteria Criteria Details Other Criteria ONE OF THE FOLLOWING: (1) HIGH RISK FOR FRACTURES DEFINED AS ONE OF THE FOLLOWING: (A) HISTORY OF OSTEOPOROTIC (I.E., FRAGILITY, LOW TRAUMA) FRACTURE(S), (B) 2 OR MORE RISK FACTORS FOR FRACTURE (E.G., HISTORY OF MULTIPLE RECENT LOW TRAUMA FRACTURES, BMD T-SCORE LESS THAN OR EQUAL TO -2.5, CORTICOSTEROID USE, OR USE OF GNRH ANALOGS), OR (C) NO PRIOR TREATMENT FOR OSTEOPOROSIS AND FRAX SCORE OF AT LEAST 20% FOR ANY MAJOR FRACTURE OR OF AT LEAST 3% FOR HIP FRACTURE. (2) UNABLE TO USE ORAL THERAPY (I.E., UPPER GASTROINTESTINAL PROBLEMS UNABLE TO TOLERATE ORAL MEDICATION, LOWER GASTROINTESTINAL PROBLEMS UNABLE TO ABSORB ORAL MEDICATIONS, TROUBLE REMEMBERING TO TAKE ORAL MEDICATIONS OR COORDINATING AN ORAL BISPHOSPHONATE WITH OTHER ORAL MEDICATIONS OR THEIR DAILY ROUTINE). (3) ADEQUATE TRIAL OF, INTOLERANCE TO, OR A CONTRAINDICATION TO ONE BISPHOSPHONATE. Indications All FDA-approved Indications. Off Label Uses 2 ABATACEPT IV Products Affected • ORENCIA (WITH MALTOSE) PA Criteria Criteria Details Exclusion Criteria Required Medical Information Age Restrictions Prescriber RHEUMATOID ARTHRITIS AND POLYARTICULAR Restrictions JUVENILE IDIOPATHIC ARTHRITIS: PRESCRIBED BY OR GIVEN IN CONSULTATION WITH A RHEUMATOLOGIST. PSORIATIC ARTHRITIS: PRESCRIBED BY OR GIVEN IN CONSULTATION WITH A DERMATOLOGIST OR RHEUMATOLOGIST. Coverage INITIAL: 6 MONTHS. RENEWAL: 12 MONTHS. Duration Other Criteria INITIAL: RHEUMATOID ARTHRITIS (RA): PREVIOUS TRIAL OF OR CONTRAINDICATION TO ANY TWO OF THE FOLLOWING PREFERRED AGENTS: HUMIRA, ENBREL, XELJANZ, RINVOQ. -

References (PDF)
References I-9012 1. Saizen prescribing information. EMD Serono, Inc. February 2020. 2. Serostim prescribing information. EMD Serono, Inc. June 2019. 3. Zorbtive prescribing information. EMD Serono, Inc. September 2019. 4. Genotropin prescribing information. Pfizer, Inc./Pharmacia and Upjohn Co. April 2019. 5. Humatrope prescribing information. Eli Lilly and Company. October 2019. 6. Norditropin FlexPro prescribing information. Novo Nordisk Inc. March 2020. 7. Omnitrope prescribing information. Sandoz Inc. June 2019. 8. Nutropin AQ NuSpin prescribing information. December 2016. 9. Zomacton prescribing information. Ferring Pharmaceuticals Inc. July 2018. 10. Richmond EJ, Rogol AD, et al. Diagnosis of Growth Hormone Deficiency in Children. UptoDate. Literature review current through June 2020. Last updated March 2020. Accessed July 2020. 11. Grimberg A, DiVall SA, Polychronakos C, et al. Pediatric Endocrine Society Guidelines for Growth Hormone and Insulin-Like Growth Factor-1 Treatment in Children and Adolescents: Growth Hormone Deficiency, Idiopathic Short Stature, and Primary Insulin-Like Growth Factor-1 Deficiency. Horm Res Paediatr. 2016;86:361–397. 12. Collett-Solberg PF, Ambler G, Backeljauw PF, et al. Growth Hormone Research Society International Perspective Guidelines for Diagnosis, Genetics, and Therapy of Short Stature in Children. Horm Res Paediatr. 2019;92:1-14. 13. Growth Hormone Research Society (GRS) Consensus Guidelines for the Diagnosis and Treatment of Growth Hormone (GH) Deficiency in Childhood and Adolescence: Summary Statement. J Clin Endocrinol Metab. 2000;85(11):3990-3993. 14. Richmond EJ, Rogol AD, et al. Diagnostic Approach to Children and Adolescents with Short Stature. UptoDate. Literature review current through June 2020. Last updated January 2020. Accessed July 2020.