Growth Hormones Is Recommended in Those Who Meet the Following Criteria
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

DRUGS REQUIRING PRIOR AUTHORIZATION in the MEDICAL BENEFIT Page 1
Effective Date: 08/01/2021 DRUGS REQUIRING PRIOR AUTHORIZATION IN THE MEDICAL BENEFIT Page 1 Therapeutic Category Drug Class Trade Name Generic Name HCPCS Procedure Code HCPCS Procedure Code Description Anti-infectives Antiretrovirals, HIV CABENUVA cabotegravir-rilpivirine C9077 Injection, cabotegravir and rilpivirine, 2mg/3mg Antithrombotic Agents von Willebrand Factor-Directed Antibody CABLIVI caplacizumab-yhdp C9047 Injection, caplacizumab-yhdp, 1 mg Cardiology Antilipemic EVKEEZA evinacumab-dgnb C9079 Injection, evinacumab-dgnb, 5 mg Cardiology Hemostatic Agent BERINERT c1 esterase J0597 Injection, C1 esterase inhibitor (human), Berinert, 10 units Cardiology Hemostatic Agent CINRYZE c1 esterase J0598 Injection, C1 esterase inhibitor (human), Cinryze, 10 units Cardiology Hemostatic Agent FIRAZYR icatibant J1744 Injection, icatibant, 1 mg Cardiology Hemostatic Agent HAEGARDA c1 esterase J0599 Injection, C1 esterase inhibitor (human), (Haegarda), 10 units Cardiology Hemostatic Agent ICATIBANT (generic) icatibant J1744 Injection, icatibant, 1 mg Cardiology Hemostatic Agent KALBITOR ecallantide J1290 Injection, ecallantide, 1 mg Cardiology Hemostatic Agent RUCONEST c1 esterase J0596 Injection, C1 esterase inhibitor (recombinant), Ruconest, 10 units Injection, lanadelumab-flyo, 1 mg (code may be used for Medicare when drug administered under Cardiology Hemostatic Agent TAKHZYRO lanadelumab-flyo J0593 direct supervision of a physician, not for use when drug is self-administered) Cardiology Pulmonary Arterial Hypertension EPOPROSTENOL (generic) -

Abstracts from the 9Th Biennial Scientific Meeting of The
International Journal of Pediatric Endocrinology 2017, 2017(Suppl 1):15 DOI 10.1186/s13633-017-0054-x MEETING ABSTRACTS Open Access Abstracts from the 9th Biennial Scientific Meeting of the Asia Pacific Paediatric Endocrine Society (APPES) and the 50th Annual Meeting of the Japanese Society for Pediatric Endocrinology (JSPE) Tokyo, Japan. 17-20 November 2016 Published: 28 Dec 2017 PS1 Heritable forms of primary bone fragility in children typically lead to Fat fate and disease - from science to global policy a clinical diagnosis of either osteogenesis imperfecta (OI) or juvenile Peter Gluckman osteoporosis (JO). OI is usually caused by dominant mutations affect- Office of Chief Science Advsor to the Prime Minister ing one of the two genes that code for two collagen type I, but a re- International Journal of Pediatric Endocrinology 2017, 2017(Suppl 1):PS1 cessive form of OI is present in 5-10% of individuals with a clinical diagnosis of OI. Most of the involved genes code for proteins that Attempts to deal with the obesity epidemic based solely on adult be- play a role in the processing of collagen type I protein (BMP1, havioural change have been rather disappointing. Indeed the evidence CREB3L1, CRTAP, LEPRE1, P4HB, PPIB, FKBP10, PLOD2, SERPINF1, that biological, developmental and contextual factors are operating SERPINH1, SEC24D, SPARC, from the earliest stages in development and indeed across generations TMEM38B), or interfere with osteoblast function (SP7, WNT1). Specific is compelling. The marked individual differences in the sensitivity to the phenotypes are caused by mutations in SERPINF1 (recessive OI type obesogenic environment need to be understood at both the individual VI), P4HB (Cole-Carpenter syndrome) and SEC24D (‘Cole-Carpenter and population level. -

SPECIALTY MEDICATIONS Available Through Accredo Health Group, Inc., Medco’S Specialty Pharmacy Call Toll-Free (800) 803-2523, 8:00 A.M
SPECIALTY MEDICATIONS available through Accredo Health Group, Inc., Medco’s specialty pharmacy Call toll-free (800) 803-2523, 8:00 a.m. to 8:00 p.m., eastern time, Monday through Friday, to confirm that your medication is covered. Effective as of July 1, 2011 Abraxane® (paclitaxel protein-bound particles) Berinert® (C 1 esterase inhibitor [human])* (PA) (QD) Actemra ™ (tocilizumab) (PA) Betaseron® (interferon beta-1b) (PA) Actimmune® (interferon gamma-1b) (PA) Botox® (botulinum toxin type A) (PA) Adagen® (pegademase bovine) Carbaglu ™ (carglumic acid) Adcirca® (tadalafil) (ST) (QD) Carimune® NF (immune globulin intravenous [human]) (PA) Advate® (antihemophilic factor [recombinant]) (CPA) Cerezyme® (imiglucerase) (CPA) (ST) Afinitor® (everolimus) (PA) (QD) Cimzia® (certolizumab pegol) (ST) Aldurazyme® (laronidase) (CPA) Copaxone® (glatiramer acetate) (PA) Alphanate® (antihemophilic factor [human]) (CPA) Copegus® (ribavirin) (ST) AlphaNine® SD (coagulation factor IX [human]) (CPA) Corifact® (factor XIII [human]) (CPA) Amevive® (alefacept) (PA) Cystadane® (betaine) Ampyra ™ (dalfampridine) (PA) CytoGam® (cytomegalovirus immune globulin Apokyn® (apomorphine hydrochloride) (PA) (QD) intravenous [human])* (CPA) Aralast® (alpha[1]-proteinase inhibitor [human]) Cytovene® IV (ganciclovir sodium)* Aranesp® (darbepoetin alfa) (PA) Dacogen® (decitabine) Arcalyst® (rilonacept) (PA) (QD) Dysport® (abobotulinumtoxinA) (PA) Arixtra® (fondaparinux sodium)* Egrifta ™ (tesamorelin) (PA) Arranon® (nelarabine) Elaprase® (idursulfase) (CPA) Arzerra® (ofatumumab) -

January 2021 Update
PUBLISHED JULY 08, 2021 OCTOBER/DECEMBER 2020; JANUARY 2021 UPDATE CHANGES TO THE HIGHMARK DRUG FORMULARIES Following is the update to the Highmark Drug Formularies and pharmaceutical management procedures for January 2021. The formularies and pharmaceutical management procedures are updated on a bimonthly basis, and the following changes reflect the decisions made in October, December, and January by our Pharmacy and Therapeutics Committee. These updates are effective on the dates noted throughout this document. Please reference the guide below to navigate this communication: Section I. Highmark Commercial and Healthcare Reform Formularies A. Changes to the Highmark Comprehensive Formulary and the Highmark Comprehensive Healthcare Reform Formulary B. Changes to the Highmark Healthcare Reform Essential Formulary C. Changes to the Highmark Core Formulary D. Changes to the Highmark National Select Formulary E. Updates to the Pharmacy Utilization Management Programs 1. Prior Authorization Program 2. Managed Prescription Drug Coverage (MRxC) Program 3. Formulary Program 4. Quantity Level Limit (QLL) Programs As an added convenience, you can also search our drug formularies and view utilization management policies on the Provider Resource Center (accessible via NaviNet® or our website). Click the Pharmacy Program/Formularies link from the menu on the left. Highmark Blue Cross Blue Shield Delaware is an independent licensee of the Blue Cross and Blue Shield Association. NaviNet is a registered trademark of NaviNet, Inc., which is an independent company that provides secure, web-based portal between providers and health insurance companies. IMPORTANT DRUG SAFETY UPDATES 03/31/2021 – Studies show increased risk of heart rhythm problems with seizure and mental health medicine lamotrigine (Lamictal) in patients with heart disease. -
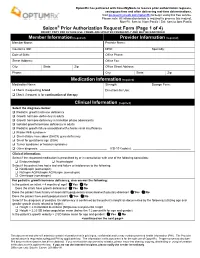
Saizen Prior Authorization Request Form (Page 1 of 4) DO NOT COPY for FUTURE USE
OptumRx has partnered with CoverMyMeds to receive prior authorization requests, saving you time and often delivering real-time determinations. Visit go.covermymeds.com/OptumRx to begin using this free service. Please note: All information below is required to process this request. Mon-Fri: 5am to 10pm Pacific / Sat: 6am to 3pm Pacific ® Saizen Prior Authorization Request Form (Page 1 of 4) DO NOT COPY FOR FUTURE USE. FORMS ARE UPDATED FREQUENTLY AND MAY BE BARCODED Member Information (required) Provider Information (required) Member Name: Provider Name: Insurance ID#: NPI#: Specialty: Date of Birth: Office Phone: Street Address: Office Fax: City: State: Zip: Office Street Address: Phone: City: State: Zip: Medication Information (required) Medication Name: Strength: Dosage Form: Check if requesting brand Directions for Use: Check if request is for continuation of therapy Clinical Information (required) Select the diagnosis below: Pediatric growth hormone deficiency Growth hormone deficiency in adults Growth hormone deficiency in transition phase adolescents Isolated growth hormone deficiency in adults Pediatric growth failure associated with chronic renal insufficiency Prader-Willi syndrome Short-stature homeobox (SHOX) gene deficiency Small for gestational age (SGA) Turner syndrome or Noonan syndrome Other diagnosis: _________________________________________ ICD-10 Code(s): ___________________________________ Clinical Information: Select if the requested medication is prescribed by or in consultation with one of the following -

Classification Decisions Taken by the Harmonized System Committee from the 47Th to 60Th Sessions (2011
CLASSIFICATION DECISIONS TAKEN BY THE HARMONIZED SYSTEM COMMITTEE FROM THE 47TH TO 60TH SESSIONS (2011 - 2018) WORLD CUSTOMS ORGANIZATION Rue du Marché 30 B-1210 Brussels Belgium November 2011 Copyright © 2011 World Customs Organization. All rights reserved. Requests and inquiries concerning translation, reproduction and adaptation rights should be addressed to [email protected]. D/2011/0448/25 The following list contains the classification decisions (other than those subject to a reservation) taken by the Harmonized System Committee ( 47th Session – March 2011) on specific products, together with their related Harmonized System code numbers and, in certain cases, the classification rationale. Advice Parties seeking to import or export merchandise covered by a decision are advised to verify the implementation of the decision by the importing or exporting country, as the case may be. HS codes Classification No Product description Classification considered rationale 1. Preparation, in the form of a powder, consisting of 92 % sugar, 6 % 2106.90 GRIs 1 and 6 black currant powder, anticaking agent, citric acid and black currant flavouring, put up for retail sale in 32-gram sachets, intended to be consumed as a beverage after mixing with hot water. 2. Vanutide cridificar (INN List 100). 3002.20 3. Certain INN products. Chapters 28, 29 (See “INN List 101” at the end of this publication.) and 30 4. Certain INN products. Chapters 13, 29 (See “INN List 102” at the end of this publication.) and 30 5. Certain INN products. Chapters 28, 29, (See “INN List 103” at the end of this publication.) 30, 35 and 39 6. Re-classification of INN products. -

Somatropin Adult Mcp004d
Subject: Recombinant Human Growth Hormone Original Effective Date: 7/5/2007 (somatropin)_ADULT Growth Hormone Deficiency ° GHD ° HIV/AIDS-associated wasting and cachexia ° Short Bowel Syndrome (SBS) Policy Number: Revision Date(s): 4/28/2010, 4/27/2011, MCP-004-D 3/14/2017 Review Dates: 4/28/2010, 4/27/2011, 3/14/2017, 7/10/2018 DISCLAIMER This Molina Clinical Policy (MCP) is intended to facilitate the Utilization Management process. It expresses Molina's determination as to whether certain services or supplies are medically necessary, experimental, investigational, or cosmetic for purposes of determining appropriateness of payment. The conclusion that a particular service or supply is medically necessary does not constitute a representation or warranty that this service or supply is covered (i.e., will be paid for by Molina) for a particular member. The member's benefit plan determines coverage. Each benefit plan defines which services are covered, which are excluded, and which are subject to dollar caps or other limits. Members and their providers will need to consult the member's benefit plan to determine if there are any exclusion(s) or other benefit limitations applicable to this service or supply. If there is a discrepancy between this policy and a member's plan of benefits, the benefits plan will govern. In addition, coverage may be mandated by applicable legal requirements of a State, the Federal government or CMS for Medicare and Medicaid members. CMS's Coverage Database can be found on the CMS website. The coverage directive(s) and criteria from an existing National Coverage Determination (NCD) or Local Coverage Determination (LCD) will supersede the contents of this MCP document and provide the directive for all Medicare members. -

62. Deutscher Kongress Für Endokrinologie
62. Deutscher Kongress für Endokrinologie dge2019.de TAGUNGS- FÜHRER 20.–22. März 2019 © Conny Blaack M.A., kunst & mediendesign, 37130 Gleichen/Bremke GÖTTINGEN Kongresspräsidentin: HAUPTTHEMEN Prof. Dr. Heide Siggelkow Knochen als hormonelles Organ Wissenschaftliche Kongresssekretärin: Vitamin D, das endokrine und Dr. Katja Gollisch metabolische System Kongressorganisation: Individualisierte Osteoporosetherapie EndoScience Endokrinologie Service GmbH Update Andrologie nach Berthold Endokrine Onkologie Mittwoch, 20.03.2019 Programmübersicht Raum Lichtenberg Raum Gauss Raum Heisenberg Raum Gebrüder Grimm Raum Göttinger Sieben 09:00 – 10:30 Vorstandssitzung 09:00 – 12:00 S. 18 Sektionstreffen YARE / MuSkITYRS 10:30 – 11:30 Pressekonferenz S. 18 S. 18 11:30 – 12:30 Eröffung der Industrieausstellung S. 19 12:30 – 13:00 Kongresseröffnung S. 19 13:00 – 13:45 Aktuelles zur Mikrobiom-Hor- mon-Achse: Prof. Dr. Bar- bara Obermayer- Pietsch, Graz, Österreich S. 19 13:45 – 14:15 Lunch 13:45 – 14:45 Akromegalieregister 14:00 – 15:00 Neugründung 14:15 – 15:15 14:00 – 16:00 S. 19 der AG Labor Satelliten Symposium 1: 14:15 – 15:45 S1: Vom Tiermodell zum UCB Pharma GmbH S. 20 Satelliten Symposium 2: Menschen – Aktuelles S. 22 Merck Serono GmbH zur Reproduktions- endokrinologie S. 22 15:45 – 16:15 Kaffeepause S. 20 16:00 – 17:30 16:15 – 17:15 16:00 – 17:30 S2: Hypophysen- Sektionstreffen MTE 1 16:15 – 17:45 15:00 – 19:15 erkrankungen Reproduktions- MTE 2 S3 Hauptthema: Endokrinologie in der Schwangerschaft biologie und -medizin Cortisol und Knochen: für die Praxis S. 24 Freunde oder Feinde? update 2019 S. 23 S. 23/24 (kostenpflichtig) separate Anmeldung S. -

September 2017 ~ Resource #330909
−This Clinical Resource gives subscribers additional insight related to the Recommendations published in− September 2017 ~ Resource #330909 Medications Stored in the Refrigerator (Information below comes from current U.S. and Canadian product labeling and is current as of date of publication) Proper medication storage is important to ensure medication shelf life until the manufacturer expiration date and to reduce waste. Many meds are recommended to be stored at controlled-room temperature. However, several meds require storage in the refrigerator or freezer to ensure stability. See our toolbox, Medication Storage: Maintaining the Cold Chain, for helpful storage tips and other resources. Though most meds requiring storage at temperatures colder than room temperature should be stored in the refrigerator, expect to see a few meds require storage in the freezer. Some examples of medications requiring frozen storage conditions include: anthrax immune globulin (Anthrasil [U.S. only]), carmustine wafer (Gliadel [U.S. only]), cholera (live) vaccine (Vaxchora), dinoprostone vaginal insert (Cervidil), dinoprostone vaginal suppository (Prostin E2 [U.S.]), varicella vaccine (Varivax [U.S.]; Varivax III [Canada] can be stored in the refrigerator or freezer), zoster vaccine (Zostavax [U.S.]; Zostavax II [Canada] can be stored in the refrigerator or freezer). Use the list below to help identify medications requiring refrigerator storage and become familiar with acceptable temperature excursions from recommended storage conditions. Abbreviations: RT = room temperature Abaloparatide (Tymlos [U.S.]) Aflibercept (Eylea) Amphotericin B (Abelcet, Fungizone) • Once open, may store at RT (68°F to 77°F • May store at RT (77°F [25°C]) for up to Anakinra (Kineret) [20°C to 25°C]) for up to 30 days. -

ANONYMOUS V MERCK SERONO Conduct of Representative
CASE AUTH/2591/3/13 ANONYMOUS v MERCK SERONO Conduct of representative An anonymous, non-contactable complainant, An anonymous, non-contactable complainant, complained about the conduct of an un-named complained about the conduct of an un-named representative from Merck Serono who had representative from Merck Serono. requested a monthly visit throughout 2013. The complainant stated that he/she felt harassed as COMPLAINT such frequent meetings were unnecessary. The complainant was informed that these visits were The complainant was concerned about a meeting required to meet an instruction to have meetings that he/she had had with a Merck Serono with seven health professionals each day. representative. The complainant alleged that the representative had requested that he/she plan a The complainant noted that before this episode, monthly visit with him/her throughout 2013. The he/she had always found the representative to be complainant stated that he/she felt harassed by this very professional and an asset to the company. The request as such frequent meetings were completely complainant considered that the representatives unnecessary. When the complainant asked why the were being forced to behave in this way by representative wanted to plan so many meetings in unrealistic expectations from their managers. advance he/she was informed that these visits were required to meet an instruction to have meetings The detailed response from Merck Serono is given with seven health professionals each day. below. The complainant noted that before this episode, he/ The Panel noted that Merck Serono’s instructions to she had always found this representative to be very its representatives referred to a number of different professional and an asset to his/her company. -

Earnings Presentation
GOOD START INTO MerckTHE KGaA , Darmstadt,YEAR Germany, Q1 2016 results Marcus Kuhnert, CFO Belén Garijo, CEO Healthcare May 19, 2016 Disclaimer Publication of Merck KGaA, Darmstadt, Germany. In the United States and Canada the group of companies affiliated with Merck KGaA, Darmstadt, Germany operates under individual business names (EMD Serono, Millipore Sigma, EMD Performance Materials). To reflect such fact and to avoid any misconceptions of the reader of the publication certain logos, terms and business descriptions of the publication have been substituted or additional descriptions have been added. This version of the publication, therefore, slightly deviates from the otherwise identical version of the publication provided outside the United States and Canada. 2 Disclaimer Cautionary Note Regarding Forward-Looking Statements and financial indicators This communication may include “forward-looking statements.” Statements that include words such as “anticipate,” “expect,” “should,” “would,” “intend,” “plan,” “project,” “seek,” “believe,” “will,” and other words of similar meaning in connection with future events or future operating or financial performance are often used to identify forward-looking statements. All statements in this communication, other than those relating to historical information or current conditions, are forward-looking statements. We intend these forward-looking statements to be covered by the safe harbor provisions for forward-looking statements in the Private Securities Litigation Reform Act of 1995. These forward-looking -

GROWTH HORMONE (Adult Therapy) Genotropin, Humatrope, Norditropin, Nutropin, Nutropin AQ, Omnitrope, Saizen, Sogroya*, Zomacton
GROWTH HORMONE (Adult therapy) Genotropin, Humatrope, Norditropin, Nutropin, Nutropin AQ, Omnitrope, Saizen, Sogroya*, Zomacton Bolded medications are the preferred products *This medication is included in this policy but is not available in the market as of yet RATIONALE FOR INCLUSION IN PA PROGRAM Background Growth hormone deficiency (GHD) in adulthood, associated with hypothalamic-pituitary dysfunction is now widely accepted as a distinct clinical syndrome, and is linked to a substantial number of significant co-morbidities, many of which can be ameliorated with growth hormone replacement therapy (1). The FDA has approved growth hormone replacement for use in adult patients with growth hormone deficiency. Approved indications are for the treatment of adults with either adult onset or childhood onset GHD. With the exception of idiopathic adult onset GHD, GHD should be confirmed as due to pituitary disease from known causes, including pituitary tumor, pituitary surgical damage, hypothalamic disease, irradiation, trauma, or reconfirmed childhood GHD. Growth hormone should only be prescribed to patients with clinical features suggestive of adult GHD and biochemically proven evidence of adult GHD (1-9). Regulatory Status FDA approved indications: Human growth hormone is indicated for treatment of adult patients with either childhood-onset or adult-onset GH deficiency (2-9). The laboratory diagnosis of GHD in adults is determined by dynamic endocrine testing. Because growth hormone has a short half-life in blood growth hormone levels frequently are undetectable in blood samples obtained at random from normal subjects. For this reason, a stimulation test is needed to confirm the diagnosis. American Association of Clinical Endocrinologists (AACE) does not recommend growth hormone stimulation testing in patients with three or more pituitary hormone deficiencies and low IGF1 (2-9).