VNSNY CHOICE Total Prior Authorization Requirements Effective: 01/01/2021
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

DRUGS REQUIRING PRIOR AUTHORIZATION in the MEDICAL BENEFIT Page 1
Effective Date: 08/01/2021 DRUGS REQUIRING PRIOR AUTHORIZATION IN THE MEDICAL BENEFIT Page 1 Therapeutic Category Drug Class Trade Name Generic Name HCPCS Procedure Code HCPCS Procedure Code Description Anti-infectives Antiretrovirals, HIV CABENUVA cabotegravir-rilpivirine C9077 Injection, cabotegravir and rilpivirine, 2mg/3mg Antithrombotic Agents von Willebrand Factor-Directed Antibody CABLIVI caplacizumab-yhdp C9047 Injection, caplacizumab-yhdp, 1 mg Cardiology Antilipemic EVKEEZA evinacumab-dgnb C9079 Injection, evinacumab-dgnb, 5 mg Cardiology Hemostatic Agent BERINERT c1 esterase J0597 Injection, C1 esterase inhibitor (human), Berinert, 10 units Cardiology Hemostatic Agent CINRYZE c1 esterase J0598 Injection, C1 esterase inhibitor (human), Cinryze, 10 units Cardiology Hemostatic Agent FIRAZYR icatibant J1744 Injection, icatibant, 1 mg Cardiology Hemostatic Agent HAEGARDA c1 esterase J0599 Injection, C1 esterase inhibitor (human), (Haegarda), 10 units Cardiology Hemostatic Agent ICATIBANT (generic) icatibant J1744 Injection, icatibant, 1 mg Cardiology Hemostatic Agent KALBITOR ecallantide J1290 Injection, ecallantide, 1 mg Cardiology Hemostatic Agent RUCONEST c1 esterase J0596 Injection, C1 esterase inhibitor (recombinant), Ruconest, 10 units Injection, lanadelumab-flyo, 1 mg (code may be used for Medicare when drug administered under Cardiology Hemostatic Agent TAKHZYRO lanadelumab-flyo J0593 direct supervision of a physician, not for use when drug is self-administered) Cardiology Pulmonary Arterial Hypertension EPOPROSTENOL (generic) -

SPECIALTY MEDICATIONS Available Through Accredo Health Group, Inc., Medco’S Specialty Pharmacy Call Toll-Free (800) 803-2523, 8:00 A.M
SPECIALTY MEDICATIONS available through Accredo Health Group, Inc., Medco’s specialty pharmacy Call toll-free (800) 803-2523, 8:00 a.m. to 8:00 p.m., eastern time, Monday through Friday, to confirm that your medication is covered. Effective as of July 1, 2011 Abraxane® (paclitaxel protein-bound particles) Berinert® (C 1 esterase inhibitor [human])* (PA) (QD) Actemra ™ (tocilizumab) (PA) Betaseron® (interferon beta-1b) (PA) Actimmune® (interferon gamma-1b) (PA) Botox® (botulinum toxin type A) (PA) Adagen® (pegademase bovine) Carbaglu ™ (carglumic acid) Adcirca® (tadalafil) (ST) (QD) Carimune® NF (immune globulin intravenous [human]) (PA) Advate® (antihemophilic factor [recombinant]) (CPA) Cerezyme® (imiglucerase) (CPA) (ST) Afinitor® (everolimus) (PA) (QD) Cimzia® (certolizumab pegol) (ST) Aldurazyme® (laronidase) (CPA) Copaxone® (glatiramer acetate) (PA) Alphanate® (antihemophilic factor [human]) (CPA) Copegus® (ribavirin) (ST) AlphaNine® SD (coagulation factor IX [human]) (CPA) Corifact® (factor XIII [human]) (CPA) Amevive® (alefacept) (PA) Cystadane® (betaine) Ampyra ™ (dalfampridine) (PA) CytoGam® (cytomegalovirus immune globulin Apokyn® (apomorphine hydrochloride) (PA) (QD) intravenous [human])* (CPA) Aralast® (alpha[1]-proteinase inhibitor [human]) Cytovene® IV (ganciclovir sodium)* Aranesp® (darbepoetin alfa) (PA) Dacogen® (decitabine) Arcalyst® (rilonacept) (PA) (QD) Dysport® (abobotulinumtoxinA) (PA) Arixtra® (fondaparinux sodium)* Egrifta ™ (tesamorelin) (PA) Arranon® (nelarabine) Elaprase® (idursulfase) (CPA) Arzerra® (ofatumumab) -

Somatropin Adult Mcp004d
Subject: Recombinant Human Growth Hormone Original Effective Date: 7/5/2007 (somatropin)_ADULT Growth Hormone Deficiency ° GHD ° HIV/AIDS-associated wasting and cachexia ° Short Bowel Syndrome (SBS) Policy Number: Revision Date(s): 4/28/2010, 4/27/2011, MCP-004-D 3/14/2017 Review Dates: 4/28/2010, 4/27/2011, 3/14/2017, 7/10/2018 DISCLAIMER This Molina Clinical Policy (MCP) is intended to facilitate the Utilization Management process. It expresses Molina's determination as to whether certain services or supplies are medically necessary, experimental, investigational, or cosmetic for purposes of determining appropriateness of payment. The conclusion that a particular service or supply is medically necessary does not constitute a representation or warranty that this service or supply is covered (i.e., will be paid for by Molina) for a particular member. The member's benefit plan determines coverage. Each benefit plan defines which services are covered, which are excluded, and which are subject to dollar caps or other limits. Members and their providers will need to consult the member's benefit plan to determine if there are any exclusion(s) or other benefit limitations applicable to this service or supply. If there is a discrepancy between this policy and a member's plan of benefits, the benefits plan will govern. In addition, coverage may be mandated by applicable legal requirements of a State, the Federal government or CMS for Medicare and Medicaid members. CMS's Coverage Database can be found on the CMS website. The coverage directive(s) and criteria from an existing National Coverage Determination (NCD) or Local Coverage Determination (LCD) will supersede the contents of this MCP document and provide the directive for all Medicare members. -

Earnings Presentation
GOOD START INTO MerckTHE KGaA , Darmstadt,YEAR Germany, Q1 2016 results Marcus Kuhnert, CFO Belén Garijo, CEO Healthcare May 19, 2016 Disclaimer Publication of Merck KGaA, Darmstadt, Germany. In the United States and Canada the group of companies affiliated with Merck KGaA, Darmstadt, Germany operates under individual business names (EMD Serono, Millipore Sigma, EMD Performance Materials). To reflect such fact and to avoid any misconceptions of the reader of the publication certain logos, terms and business descriptions of the publication have been substituted or additional descriptions have been added. This version of the publication, therefore, slightly deviates from the otherwise identical version of the publication provided outside the United States and Canada. 2 Disclaimer Cautionary Note Regarding Forward-Looking Statements and financial indicators This communication may include “forward-looking statements.” Statements that include words such as “anticipate,” “expect,” “should,” “would,” “intend,” “plan,” “project,” “seek,” “believe,” “will,” and other words of similar meaning in connection with future events or future operating or financial performance are often used to identify forward-looking statements. All statements in this communication, other than those relating to historical information or current conditions, are forward-looking statements. We intend these forward-looking statements to be covered by the safe harbor provisions for forward-looking statements in the Private Securities Litigation Reform Act of 1995. These forward-looking -

Exactus Drug List by Disease State
Name changes, innovation continues Name changes, patient care continues Anemia ALIMTA ELOXATIN KISQALI SYLATRON ARANESP ALKERAN ELSPAR KYPROLIS SYNRIBO EPOGEN ARRANON EMPLICITI LETROZOLE TAFINLAR PROCRIT ARZERRA ERBITUX LEUCOVORIN CALCIUM TARCEVA RETACRIT AVASTIN ERIVEDGE LEUSTATIN TARGRETIN AZACITIDINE ERWINAZE LUPANETA PACK TASIGNA Anticoagulants BCG VACCINE (TICE STRAIN) ETHYOL MEKINIST TAXOTERE ARIXTRA BENDEKA ETOPOPHOS MESNA TEMODAR ENOXAPARIN SODIUM BESPONSA ETOPOSIDE MITOMYCIN TEMOZOLOMIDE FONDAPARINUX SODIUM BEXXAR FARYDAK MITOXANTRONE HCL THALOMID FRAGMIN BICNU FASLODEX MOZOBIL THIOTEPA LOVENOX BLEOMYCIN SULFATE FEMARA MUSTARGEN TOPOTECAN HCL CAMPATH FLUDARA MYLOTARG TORISEL Anti-Emetic CAMPTOSAR FOLOTYN NINLARO TREANDA AKYNZEO CAPECITABINE FUSILEV NIPENT TRELSTAR GRANISETRON HCL CARBOPLATIN GAZYVA NOVANTRONE TRETINOIN SANCUSO CERUBIDINE GEMCITABINE HCL ODOMZO TRISENOX SUSTOL CISPLATIN GEMZAR OFORTA TYKERB ONDANSETRON HCL CLADRIBINE GLEEVEC ONCASPAR VALSTAR CLOLAR HALAVEN ONTAK VANDETANIB Asthma COSMEGEN HERCEPTIN ONUREG VANTAS CINQAIR COTELLIC HYCAMTIN OPDIVO VECTIBIX DUPIXENT CYCLOPHOSPHAMIDE IDAMYCIN PFS OXALIPLATIN VELCADE XOLAIR CYTARABINE IDARUBICIN HCL PACLITAXEL VENOFER DACARBAZINE IFEX PERJETA VIDAZA Cancer/Chemotherapy DACOGEN IFOSFAMIDE PIQRAY VINCRISTINE SULFATE ABRAXANE DARZALEX IMATINIB MESYLATE POMALYST VINORELBINE TARTRATE ADCETRIS DAUNOXOME IRINOTECAN HCL PROLEUKIN VOTRIENT ADRIAMYCIN DECITABINE ISTODAX REVLIMID XELODA ADRUCIL DOCETAXEL IXEMPRA RITUXAN YERVOY AFINITOR DOXIL JEVTANA RYDAPT YONDELIS AFINITOR DISPERZ -

Growth Hormones Is Recommended in Those Who Meet the Following Criteria
Policy: 95015 Initial Effective Date: 06/22/1995 HCPCS J2170, J2940, J2941 and Q0515 Code(s): Annual Review Date: 06/17/2021 SUBJECT: Growth Stimulating Drugs Last Revised Date: 07/15/2021 - Genotropin(somatropin injection) - Humatrope (somatropin injection) - Increlex (mecasermin) - Norditropin® (somatropin injection) - Nutropin AQ (somatropin injection) - Omnitrope® (somatropin injection) - Saizen® (somatropin injection) - Serostim (somatropin injection) - Zomacton™ (somatropin injection) - Zorbtive (somatropin injection) - Sogroya(somapacitan injection) Prior approval is required for some or all procedure codes listed in this Corporate Drug Policy. Definition: Exogenous growth hormone (recombinant human, rhGH) is a polypeptide hormone with metabolic effects similar to endogenous human growth hormone (GH). Produced in the pituitary gland, endogenous growth hormone activates production of insulin-like growth factor-1 (IGF-1) and other peptides that: modulate lipid, carbohydrate and protein metabolism; and stimulate development of bone, cartilage, skeletal muscle and gonadal tissue, leading to longitudinal growth. Inadequate secretion or impairment of growth hormone activity during childhood and adolescence may result in short stature, growth hormone deficiency with growth failure and other medical conditions. Exogenous growth hormone products approved by the U.S. Food and Drug Administration include somatropin (Humatrope®, Nutropin®, Serostim®, Saizen®, Norditropin®, Genotropin®, Zorbtive®, Omnitrope®, ZomactonTM). These products are -

Growth Hormone
Texas Prior Authorization Program Clinical Edit Criteria Drug/Drug Class Growth Hormone Clinical Edit Information Included in this Document Excluding Serostim® / Zorbtive® • Drugs requiring prior authorization: the list of drugs requiring prior authorization for this clinical edit • Prior authorization criteria logic: a description of how the prior authorization request will be evaluated against the clinical edit criteria rules • Logic diagram: a visual depiction of the clinical edit criteria logic • Supporting tables: a collection of information associated with the steps within the criteria (diagnosis codes, procedure codes, and therapy codes); provided when applicable Serostim • Drugs requiring prior authorization: the list of drugs requiring prior authorization for this clinical edit • Prior authorization criteria logic: a description of how the prior authorization request will be evaluated against the clinical edit criteria rules • Logic diagram: a visual depiction of the clinical edit criteria logic • Supporting tables: a collection of information associated with the steps within the criteria (diagnosis codes, procedure codes, and therapy codes); provided when applicable Note: Click the hyperlink to navigate directly to that section. October 21, 2014 Copyright © 2011-2014 Health Information Designs, LLC 1 Texas Prior Authorization Program Clinical Edits Growth Hormones Zorbtive • Drugs requiring prior authorization: the list of drugs requiring prior authorization for this clinical edit • Prior authorization criteria logic: a description of how the prior authorization request will be evaluated against the clinical edit criteria rules • Logic diagram: a visual depiction of the clinical edit criteria logic • Supporting tables: a collection of information associated with the steps within the criteria (diagnosis codes, procedure codes, and therapy codes); provided when applicable Note: Click the hyperlink to navigate directly to that section. -
Pre-Certification Requirements for Procedures, Programs & Drugs
Procedures, programs and drugs that require precertification Participating provider precertification list Starting August 1, 2020 Applies to the following plans (also see General information section #1-#4, #9-#10): Aetna® plans, except Traditional Choice® plans All health benefits and insurance plans offered and/or underwritten by Innovation Health plans, Inc., and Innovation Health Insurance Company, except indemnity plans, Foreign Service Benefit Plan, MHBP and Rural Carrier Benefit Plan All health benefits and health insurance plans offered, underwritten and/or administered by the following: Banner Health and Aetna Health Insurance Company and/or Banner Health and Aetna Health Plan Inc. (Banner|Aetna), Texas Health +Aetna Health Insurance Company and/or Texas Health+Aetna Health Plan Inc. (Texas Health Aetna), Allina Health and Aetna Health Insurance Company (Allina Health| Aetna), Sutter Health and Aetna Administrative Services LLC (Sutter Health | Aetna) aetna.com 23.03.882.1 I (8/20) Proprietary For additional information, read all general precertification information Providers may submit most precertification requests electronically through the secure provider website or using your Electronic Medical Record (EMR) system portal (See #1 in the General Information section for more information on precertification). Services that require precertification: 1. Inpatient confinements (except hospice) 18. Nonparticipating freestanding ambulatory For example, surgical and nonsurgical stays, surgical facility services, when referred stays in a skilled nursing facility or rehabilitation by a participating provider facility, and maternity and newborn stays that 19. Orthognathic surgery procedures, bone grafts, osteotomies and surgical exceed the standard length of stay (LOS) (See #5 management of the temporomandibular in the General Information section). joint 2. -

Health Net Pharmaceutical Services (HNPS) at (800) 977-8226
PHARMACEUTICAL PRIOR AUTHORIZATION REQUIREMENTS Practitioners may Fax completed Prior Authorization Form to Health Net Pharmaceutical Services (HNPS) at (800) 977-8226. The following medications/classes require Prior Authorization. CONNECTICUT PLANS THIS LIST IS NOT APPLICABLE TO MEDICARE PART D PLANS DRUGS THAT REQUIRE PRIOR AUTHORIZATION FOR VARIOUS PRESCRIPTION RIDERS GENERIC NAME / DRUG CLASS BRAND NAME EXAMPLES Angiotensin II Receptor Blockers (ARBs), & ATACAND, ATACAND HCT, AVAPRO, AVALIDE, AZOR, BENICAR, BENICAR HCT, Renin Inhibitors COZAAR, DIOVAN, DIOVAN HCT, EXFORGE, HYZAAR, MICARDIS, MICARDIS HCT, TEKTURNA, TEKTURNA HCT, TEVETEN, TEVETEN HCT 2, 6 2, 6 Antidepressants CYMBALTA, EFFEXOR XR, LEXAPRO, PRISTIQ [Effective April 1, 2009] Compounded Prescriptions N/A 1 Fertility Agents BRAVELLE, CETROTIDE, GANIRELIX, HCG, FOLLISTIM AQ, FERTINEX, GONAL-F, LUPRON, LUVERIS, MENOPUR, NOVAREL, OVIDREL, PREGNYL, PROCHIEVE, PROFASI, REPRONEX, etc. 1, 5 Growth Hormone (somatropin) HUMATROPE, NUTROPIN, NUTROPIN AQ, 1, 5 (somatropin) ACCRETROPIN, GENOTROPIN, NORDITROPIN, OMNITROPE, SAIZEN, SEROSTIM, TEV-TROPIN 1, 5, 6 (IGF) INCRELEX, IPLEX 1, 5 Drug Utilization Review (DUR) exceptions See: Drug Utilization Review (DUR) & Quantity Limits (QL) Low-Sedating Antihistamines ALLEGRA, ALLEGRA-D, CLARINEX, CLARINEX-D, XYZAL 2, 6 desloratadine, fexofenadine Nicotine Addiction CHANTIX, IVERSINE, NICOTROL, ZYBAN 1 bupropion, nicotine, mecamylamine, varenicline Nutritional Supplements MSUD, PHENYL-FREE, XP-ANALOG, XPHEN, NEOCATE, etc. 1 Onychomycosis Agents -
![Growth Hormone [Somatropin]](https://docslib.b-cdn.net/cover/1560/growth-hormone-somatropin-3741560.webp)
Growth Hormone [Somatropin]
Cigna National Formulary Coverage Policy Prior Authorization Growth Disorders - Growth hormone [somatropin] Table of Contents Product Identifer(s) National Formulary Medical Necessity ................ 1 12988 Conditions Not Covered....................................... 8 Background ........................................................ 10 References ........................................................ 14 Revision History ................................................. 16 INSTRUCTIONS FOR USE The following Coverage Policy applies to health benefit plans administered by Cigna Companies. Certain Cigna Companies and/or lines of business only provide utilization review services to clients and do not make coverage determinations. References to standard benefit plan language and coverage determinations do not apply to those clients. Coverage Policies are intended to provide guidance in interpreting certain standard benefit plans administered by Cigna Companies. Please note, the terms of a customer’s particular benefit plan document [Group Service Agreement, Evidence of Coverage, Certificate of Coverage, Summary Plan Description (SPD) or similar plan document] may differ significantly from the standard benefit plans upon which these Coverage Policies are based. For example, a customer’s benefit plan document may contain a specific exclusion related to a topic addressed in a Coverage Policy. In the event of a conflict, a customer’s benefit plan document always supersedes the information in the Coverage Policies. In the absence of a controlling federal or state coverage mandate, benefits are ultimately determined by the terms of the applicable benefit plan document. Coverage determinations in each specific instance require consideration of 1) the terms of the applicable benefit plan document in effect on the date of service; 2) any applicable laws/regulations; 3) any relevant collateral source materials including Coverage Policies and; 4) the specific facts of the particular situation. -
MSM PDL Document 010109
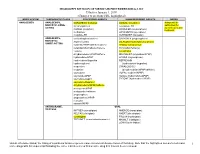
MISSISSIPPI DIVISION OF MEDICAID PREFERRED DRUG LIST Effective January 1, 2009 (Changes to previous PDL highlighted) BODY SYSTEM THERAPEUTIC CLASS PREFERRED AGENTS NON-PREFERRED AGENTS NOTES ANALGESICS ANALGESICS, DURAGESIC (fentanyl) AVINZA (morphine) Avinza will be NARCOTIC-LONG- fentanyl patches oxycodone ER authorized for ACTING patients on stable KADIAN (morphine) OPANA ER (oxymorphone) treatment. methadone OXYCONTIN (oxycodone) morphine ER ULTRAM ER (tramadol) ANALGESICS, acetaminophen/codeine DARVON-N (propoxyphene) NARCOTIC- aspirin/codeine DILAUDID liquid (hydromorphone) SHORT-ACTING butalbital/APAP/caffeine/codeine fentanyl transmucosal butalbital/ASA/caffeine/codeine FENTORA (fentanyl) codeine levorphanol dihydrocodeine/ APAP/caffeine MAGNACET (oxycodone/APAP) hydrocodone/APAP OPANA (oxymorphone) hydrocodone/ibuprofen REPREXAIN hydromorphone (hydrocodone/ibuprofen) meperidine SYNALGOS-DC morphine (dihydrocodeine/APAP/caffeine) oxycodone VOPAC (codeine/APAP) oxycodone/APAP XODOL (hydrocodone/APAP) ZYDONE (hydrocodone/APAP) oxycodone/aspirin oxycodone/ibuprofen dihydrocodeine/APAP/caffeine pentazocine/APAP pentazocine/naloxone propoxyphene propoxyphene/APAP tramadol tramadol/APAP ANTIMIGRAINE, ORAL TRIPTANS IMITREX (sumatriptan) AMERGE (naratriptan) RELPAX (eletriptan) AXERT (almotriptan) sumatriptan FROVA (frovatriptan) TREXIMET (sumatriptan/naproxen) MAXALT (rizatriptan) ZOMIG (zolmitriptan) Unless otherwise stated, the listing of a particular brand or generic name includes all dosage forms of that drug. Note that the highlighted -

Formulary Drug List
Effective Date May 2021 Foreword The following topics may apply: This document represents the efforts of the MedImpact Healthcare Systems Pharmacy and Therapeutics (P&T) and Formulary 1. Generic Substitution Committees to provide physicians and pharmacists with a method to When available, FDA approved generic drugs are to be used in evaluate the safety, efficacy and cost-effectiveness of commercially all situations, regardless of the brand name indicated. The available drug products. A structured approach to the drug selection generic names are italicized in the formulary listing wherever an process is essential in ensuring continuing patient access to rational FDA approved generic drug product is available. Greater drug therapies. economy is realized through the use of generic equivalents. This policy is not meant to preclude or supplant any state This is accomplished through the auspices of the MedImpact P&T statutes that may exist. All drugs that are or become available and Formulary Committees. These committees meet quarterly and generically are subject to review by MedImpact’s Pharmacy more often as warranted to ensure clinical relevancy of the Formulary. and Therapeutics Committee. MedImpact approves such multi- To accommodate changes to this document, updates are made source drugs for addition to the MAC list based on the following accessible as necessary. criteria: ● A multi-source drug product manufactured by at least one (1) Access to the most current version of the PEEHIP Commercial nationally marketed company. Formulary can be obtained by visiting www.rsa-al.gov. ● At least one (1) of the generic manufacturer’s products must have an “A” rating or the generic product has been The MedImpact P&T and Formulary Committees use the following determined to be unassociated with efficacy, safety or criteria in the evaluation of drug selection for the Formulary: bioequivalency concerns by the MedImpact P&T Committee.