NEW 2018 Specialty Drugs
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Quarterly Review
Tropical Gastroenterology 2008.29;4:187–193 Quarterly Have hematopoietic growth factors made an Review impact on the management of liver disease? Pankaj Tyagi and Kaushal Madan ABSTRACT Department of Gastroenterology, It is clear that the major indication for the use of hematopoietic growth factors in hepatology GB Pant Hospital & Department of is to counteract the adverse effects of interferons (neutropenia and thrombocytopenia) and Medical Hepatology, ribavirin (hemolytic anaemia) during the treatment of hepatitis C infection. This is important Institute of Liver and Biliary Sciences, because the probability of SVR depends on proper adherence to therapy (at least 80% of the New Delhi requisite dose maintained for at least 80% of the requisite duration) and proper adherence can only be achieved if the side effects are reduced to a minimum. Even though the studies Correspondence: Dr. Kaushal Madan have demonstrated beyond doubt that the use of hematopoietic growth factors does indeed Email: [email protected] reduce the incidence and severity of these adverse effects and helps the patients to complete the course of therapy, the data on improvement of SVR is still limited. There is only one study of darbepoetin and filgrastim showing the beneficial effect on SVR. Even among the hematological side effects, possibly the only significant effect which limits the use of optimal HCV therapy is the hemolytic anaemia induced by ribavirin. The other two main side effects, i.e. neutropenia and thrombocytopenia are not clinically problematic. The use of such growth factors would be particularly effective if patients who have advanced liver disease or cirrhosis are able to receive adequate anti-viral therapy as has been demonstrated in the study of eltrombopag among HCV cirrhotics. -

STIM1 Controls Calcineurin/Akt/Mtor/NFATC2‑Mediated Osteoclastogenesis Induced by RANKL/M‑CSF
736 EXPERIMENTAL AND THERAPEUTIC MEDICINE 20: 736-747, 2020 STIM1 controls calcineurin/Akt/mTOR/NFATC2‑mediated osteoclastogenesis induced by RANKL/M‑CSF YANJIAO HUANG1, QIANG LI2, ZUNYONG FENG3 and LANRONG ZHENG1 Departments of 1Pathological Anatomy, 2Anatomy and 3Forensic Medicine, Wannan Medical College, Wuhu, Anhui 241002, P.R. China Received October 15, 2018; Accepted June 20, 2019 DOI: 10.3892/etm.2020.8774 Abstract. Store-operated Ca2+ entry (SOCE) is the stable (p.E136X, p.R429C) or constitutively activated (p.R304W) calcium channel influx in most cells. It consists of the SOCE, failed to respond to RANKL/M-CSF-mediated induc- cytoplasmic ion channel ORAI and endoplasmic reticulum tion of normal osteoclastogenesis. In addition, activation of the receptor stromal interaction molecule 1 (STIM1). Abolition calcineurin/Akt/mTOR/NFATC2 signalling cascade induced of SOCE function due to ORAI1 and STIM1 gene defects by RANKL/M-CSF was abnormal in the BMDMs with may cause non-perspiration, ectoderm dysplasia and STIM1 mutants compared with that in BMDMs from healthy skeletal malformations with severe combined immunodefi- subjects. In addition, overexpression of wild-type STIM1 ciency (CID). Calcineurin/mammalian target of rapamycin restored SOCE in p.R429C- and p.E136X-mutant BMDMs, but (mTOR)/nuclear factor of activated T cells 2 (NFATC2) is not in p.R304W-mutant BMDMs. Of note, calcineurin, cyclo- an important signalling cascade for osteoclast development. sporin A, mTOR inhibitor rapamycin and NFATC2‑specific Calcineurin is activated by Ca2+ via SOCE during osteoclas- small interfering RNA restored the function of SOCE in togenesis, which is induced by receptor activator of NF-κB p.R304W-mutant BMDMs. -

Managing Adverse Effects and Complications in Completing Treatment for Hepatitis C Virus Infection
HCV Treatment Complications Volume 20 Issue 4 October/November 2012 Perspective Managing Adverse Effects and Complications in Completing Treatment for Hepatitis C Virus Infection The addition of direct-acting antivirals (DAAs) to hepatitis C virus (HCV) Psychiatric Complications treatment regimens has made treatment more effective and patient Depression is the most common psy- management more complex. Shepherding patients through a full course of chiatric complication encountered in HCV therapy requires motivation and involvement on the part of the patient HCV patients, with mild to moderate and the physician. Indeed, physician inexperience and lack of confidence in depression found in as much as 80% of guiding patients through the challenges of treatment appears to be a primary patients. Bipolar disorder and schizo- reason for early discontinuation of therapy. Among the many complications phrenia are also not infrequently en- of HCV treatment that must be managed efficiently and effectively are countered. depression and other psychiatric disorders; hematologic abnormalities There is little evidence to support including DAA- and ribavirin-associated anemia and peginterferon alfa- a benefit of preemptive antidepres- associated neutropenia and thrombocytopenia; rash and drug eruptions, sant therapy in all patients undergo- including telaprevir-associated rash; and weight loss. Practical considerations ing HCV treatment, though a recent in management of these common complications are offered. This article randomized trial of HCV patients -

Denosumab and Anti-Angiogenetic Drug-Related Osteonecrosis of the Jaw: an Uncommon but Potentially Severe Disease
ANTICANCER RESEARCH 33: 1793-1798 (2013) Denosumab and Anti-angiogenetic Drug-related Osteonecrosis of the Jaw: An Uncommon but Potentially Severe Disease STEFANO SIVOLELLA1, FRANCO LUMACHI2, EDOARDO STELLINI1 and LORENZO FAVERO1 Departments of 1Neurosciences, Section of Dentistry and 2Surgery, Oncology and Gastroenterology, University of Padua, School of Medicine, Padova, Italy Abstract. Osteonecrosis of the jaw (ONJ) is a rare but bone exposure in the oral cavity (1). Experimental radio-ONJ serious lesion of the jaw characterized by exposed necrotic was first reported in the 1960s and better-described by Zach bone and is related to several drugs usually used for treating et al. (2, 3). Currently, ONJ may represent a serious problem patients with advanced malignancies. Common therapies in patients irradiated for head and neck carcinomas, but may inducing ONJ are nitrogen-containing bisphosphonates (BPs), also be an uncommon complication of cancer chemotherapy the human monoclonal antibody to the receptor activator of (4, 5). Other causes of ONJ are local malignancy, periodontal nuclear factor-kappa B ligand denosumab and some anti- disease, trauma, and long-term glucocorticoid or angiogenic drugs, alone or in combination with BPs. The real bisphosphonate (BP) therapy (6). ONJ is a potentially incidence of ONJ is unknown. Several cases of ONJ in patients debilitating disease, which occurs in approximately 5% of with cancer who underwent denosumab therapy have been patients with myeloma or bone metastases from breast cancer reported and it seems that the overall incidence of denosumab- (BC) or prostate cancer receiving high-dose intravenous BPs related ONJ is similar to that for BP-related in this (7). -
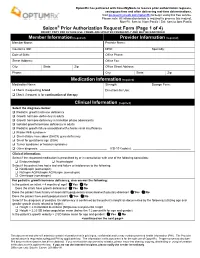
Saizen Prior Authorization Request Form (Page 1 of 4) DO NOT COPY for FUTURE USE
OptumRx has partnered with CoverMyMeds to receive prior authorization requests, saving you time and often delivering real-time determinations. Visit go.covermymeds.com/OptumRx to begin using this free service. Please note: All information below is required to process this request. Mon-Fri: 5am to 10pm Pacific / Sat: 6am to 3pm Pacific ® Saizen Prior Authorization Request Form (Page 1 of 4) DO NOT COPY FOR FUTURE USE. FORMS ARE UPDATED FREQUENTLY AND MAY BE BARCODED Member Information (required) Provider Information (required) Member Name: Provider Name: Insurance ID#: NPI#: Specialty: Date of Birth: Office Phone: Street Address: Office Fax: City: State: Zip: Office Street Address: Phone: City: State: Zip: Medication Information (required) Medication Name: Strength: Dosage Form: Check if requesting brand Directions for Use: Check if request is for continuation of therapy Clinical Information (required) Select the diagnosis below: Pediatric growth hormone deficiency Growth hormone deficiency in adults Growth hormone deficiency in transition phase adolescents Isolated growth hormone deficiency in adults Pediatric growth failure associated with chronic renal insufficiency Prader-Willi syndrome Short-stature homeobox (SHOX) gene deficiency Small for gestational age (SGA) Turner syndrome or Noonan syndrome Other diagnosis: _________________________________________ ICD-10 Code(s): ___________________________________ Clinical Information: Select if the requested medication is prescribed by or in consultation with one of the following -

Managing Osteoporosis and Joint Damage in Patients with Rheumatoid Arthritis: an Overview
Journal of Clinical Medicine Review Managing Osteoporosis and Joint Damage in Patients with Rheumatoid Arthritis: An Overview Yoshiya Tanaka The First Department of Internal Medicine, School of Medicine, University of Occupational and Environmental Health, 1-1, Iseigaoka, Kitakyushu 807-8555, Japan; [email protected]; Tel.: +81-93-603-1611; Fax: +81-93-691-7580 Abstract: In rheumatoid arthritis, a representative systemic autoimmune disease, immune abnor- mality and accompanying persistent synovitis cause bone and cartilage destruction and systemic osteoporosis. Biologics targeting tumor necrosis factor, which plays a central role in the inflammatory process, and Janus kinase inhibitors have been introduced in the treatment of rheumatoid arthritis, making clinical remission a realistic treatment goal. These drugs can prevent structural damage to bone and cartilage. In addition, osteoporosis, caused by factors such as menopause, aging, immobility, and glucocorticoid use, can be treated with bisphosphonates and the anti-receptor activator of the nuclear factor-κB ligand antibody. An imbalance in the immune system in rheumatoid arthritis induces an imbalance in bone metabolism. However, osteoporosis and bone and cartilage destruction occur through totally different mechanisms. Understanding the mechanisms underlying osteo- porosis and joint destruction in rheumatoid arthritis leads to improved care and the development of new treatments. Keywords: rheumatoid arthritis; osteoporosis; joint destruction; DMARD; biologics Citation: Tanaka, Y. Managing Osteoporosis and Joint Damage in Patients with Rheumatoid Arthritis: An Overview. J. Clin. Med. 2021, 10, 1. Introduction 1241. https://doi.org/10.3390/ Rheumatoid arthritis is a systemic autoimmune disease characterized by inflammatory jcm10061241 polyarthritis. It occurs commonly in women in their 30s to 60s, and often causes organ disorders. -

Overview of Antiviral Medications Used in Ophthalmology
ANTIVIRALS Overview of antiviral medications Jeremy Hoffman Clinical Research used in ophthalmology Fellow: International Centre for Eye Health, As eye health professionals, London School of Hygiene & Tropical we are fortunate to have Medicine, UK. a number of antiviral medications available in our armoury to treat a range of ophthalmic viral infections. This article provides an overview of what antiviral agents are available for these conditions, detailing their regimen SANDIP DAS SANYAM (SAGARMATHA CHOUDHARY EYE HOSPITAL, NEPAL) SANDIP DAS SANYAM(SAGARMATHA and evidence that Aciclovir – either as topical eye ointment or systemic tablets – is still the first-line antiviral in the treatment of many viral eye diseases around the supports their use. world, including here in Nepal. phthalmic viral infections, particularly herpes associated with toxicity, including superficial punctate simplex keratitis, have been at the forefront of keratopathy, chemical conjunctivitis, punctal occlusion Othe development of antiviral medications. and occasional serious hypersensitivity reactions. Idoxuridine was also unable to penetrate the corneal The discovery of the first targeted antiviral agent, epithelium to treat stromal or endothelial keratitis. in common with penicillin (the first antibiotic), owes much to serendipity. In 1959, William Prusoff With the advent of aciclovir in 1982, most herpetic developed idoxuridine (IDU) as a potential systemic ophthalmic infections became treatable, including anti-cancer agent. Idoxuridine those caused by herpes -

The Pennsylvania State University
The Pennsylvania State University The Graduate School Department of Chemistry SYNTHESIS OF NOVEL ANTIVIRAL AGENTS AND FLUORESCENT MOLECULAR PROBES A Dissertation in Chemistry by Runzhi Wu 2010 Runzhi Wu Submitted in Partial Fulfillment of the Requirements for the Degree of Doctor of Philosophy August 2010 The dissertation of Runzhi Wu was reviewed and approved* by the following: Blake R. Peterson Regents Distinguished Professor of Medicinal Chemistry University of Kansas Dissertation Advisor Special Member of Committee Raymond L. Funk Professor of Chemistry Chair of Committee Phillip C. Bevilacqua Professor of Chemistry Gong Chen Assistant Professor of Chemistry Avery August Distinguished Professor of Immunology Barbara J. Garrison Shapiro Professor of Chemistry Head of the Department of Chemistry *Signatures are on file in the Graduate School iii ABSTRACT RNA viruses cause a wide variety of diseases including SARS, influenza, hepatitis C and polio. Therapeutics for RNA virus infections are often limited because of the rapid development of antiviral drug resistance. RNA viruses are known to exhibit high error rates during replication and thus exist as quasispecies. To maintain the maximum adaptability, these viruses exist on the edge of “error catastrophe”, and small increases in the mutation frequency can cause a drastic decrease in viral infectivity. By taking advantage of the high mutation rate of RNA virus replication, a relatively new antiviral approach termed “lethal mutagenesis” can be used to increase the error rate of RNA viral replication to intolerable levels, resulting in the loss of viral viability. Chapter one of this dissertation reviews current antiviral therapeutics and lethal mutagenesis as an antiviral strategy. -

Paracrine and Endocrine Actions of Bone—The Functions of Secretory
Bone Research www.nature.com/boneres REVIEW ARTICLE OPEN Paracrine and endocrine actions of bone—the functions of secretory proteins from osteoblasts, osteocytes, and osteoclasts Yujiao Han1, Xiuling You1, Wenhui Xing1, Zhong Zhang1 and Weiguo Zou 1 The skeleton is a dynamic organ that is constantly remodeled. Proteins secreted from bone cells, namely osteoblasts, osteocytes, and osteoclasts exert regulation on osteoblastogenesis, osteclastogenesis, and angiogenesis in a paracrine manner. Osteoblasts secrete a range of different molecules including RANKL/OPG, M-CSF, SEMA3A, WNT5A, and WNT16 that regulate osteoclastogenesis. Osteoblasts also produce VEGFA that stimulates osteoblastogenesis and angiogenesis. Osteocytes produce sclerostin (SOST) that inhibits osteoblast differentiation and promotes osteoclast differentiation. Osteoclasts secrete factors including BMP6, CTHRC1, EFNB2, S1P, WNT10B, SEMA4D, and CT-1 that act on osteoblasts and osteocytes, and thereby influenceaA osteogenesis. Osteoclast precursors produce the angiogenic factor PDGF-BB to promote the formation of Type H vessels, which then stimulate osteoblastogenesis. Besides, the evidences over the past decades show that at least three hormones or “osteokines” from bone cells have endocrine functions. FGF23 is produced by osteoblasts and osteocytes and can regulate phosphate metabolism. Osteocalcin (OCN) secreted by osteoblasts regulates systemic glucose and energy metabolism, reproduction, and cognition. Lipocalin-2 (LCN2) is secreted by osteoblasts and can influence energy metabolism by suppressing appetite in the brain. We review the recent progresses in the paracrine and endocrine functions of the secretory proteins of osteoblasts, osteocytes, and osteoclasts, revealing connections of the skeleton with other tissues and providing added insights into the pathogenesis of degenerative diseases affecting multiple organs and the drug discovery process. -

Investor Presentation
Participants Company overview Pharmaceuticals Oncology Financial review Conclusion Appendix References Q1 2021 Results Investor presentation 1 Investor Relations │ Q1 2021 Results Participants Company overview Pharmaceuticals Oncology Financial review Conclusion Appendix References Disclaimer This presentation contains forward-looking statements within the meaning of the United States Private Securities Litigation Reform Act of 1995, that can generally be identified by words such as “potential,” “expected,” “will,” “planned,” “pipeline,” “outlook,” or similar expressions, or by express or implied discussions regarding potential new products, potential new indications for existing products, potential product launches, or regarding potential future revenues from any such products; or regarding the impact of the COVID-19 pandemic on certain therapeutic areas including dermatology, ophthalmology, our breast cancer portfolio, some newly launched brands and the Sandoz retail and anti-infectives business, and on drug development operations; or regarding potential future, pending or announced transactions; regarding potential future sales or earnings of the Group or any of its divisions; or by discussions of strategy, plans, expectations or intentions; or regarding the Group’s liquidity or cash flow positions and its ability to meet its ongoing financial obligations and operational needs; or regarding our collaboration with Molecular Partners to develop, manufacture and commercialize potential medicines for the prevention and treatment of COVID- 19 and our joining of the industry-wide efforts to meet global demand for COVID-19 vaccines and therapeutics by leveraging our manufacturing capacity and capabilities to support the production of the Pfizer-BioNTech vaccine and to manufacture the mRNA and bulk drug product for the vaccine candidate CVnCoV from CureVac. -

Trifluridine Decreases Ocular HSV-1 Recovery, but Not Herpetlc Lesions After Timolol Iontophoresis
Investigative Ophthalmology & Visual Science, Vol. 30, No. 4, April 1989 Copyright © Association for Research in Vision and Ophthalmology Trifluridine Decreases Ocular HSV-1 Recovery, but Not Herpetlc Lesions after Timolol Iontophoresis David S. Roorman,* James M. Hill, Yasuteru Harura, James J. Reidy, and Herbert E. Kaufman To determine the effect of a topically applied antiviral agent on shedding of herpes simplex virus type 1 (HSV-1) into the tear film and corneal epithelial lesions, ten rabbits latently infected with HSV-1 were subjected to transcorneal iontophoresis of 0.01% timolol once a day for 3 consecutive days to induce viral shedding and lesions. Iontophoretic induction was performed similarly in five uninfected rabbits as controls. Half of the infected rabbits and all of the uninfected controls received topical 1.0% trifluridine five times a day for 9 days, beginning the day after the first iontophoresis. All eyes were examined daily for 10 days by slit-lamp biomicroscopy and tear film samples collected on swabs were analyzed for virus. In the infected rabbits, the eyes treated with trifluridine had significantly fewer swabs positive for HSV-1 than the untreated eyes (P < 0.001); however, there was no significant difference in the numbers of lesions in the treated and untreated eyes. The uninfected controls had no positive swabs and developed no lesions. These results suggest that topical treatment with trifluridine may reduce recovery of HSV-1 from the tear film, but does not affect the incidence of iontophoretically induced cornea! epithelial lesions. Invest Ophthalmol Vis Sci 30:678-683,1989 Herpes simplex virus type 1 (HSV-1) causes an ini- ing epinephrine iontophoresis with concomitant in- tial ocular infection followed by latency in the auto- travenous and topical acyclovir, as well as a signifi- nomic and sensory ganglia of the head and neck.1"3 cant quantitative reduction in recovery of HSV-1 Stimuli such as fever, UV radiation, stress and radial from the trigeminal ganglia. -

September 2017 ~ Resource #330909
−This Clinical Resource gives subscribers additional insight related to the Recommendations published in− September 2017 ~ Resource #330909 Medications Stored in the Refrigerator (Information below comes from current U.S. and Canadian product labeling and is current as of date of publication) Proper medication storage is important to ensure medication shelf life until the manufacturer expiration date and to reduce waste. Many meds are recommended to be stored at controlled-room temperature. However, several meds require storage in the refrigerator or freezer to ensure stability. See our toolbox, Medication Storage: Maintaining the Cold Chain, for helpful storage tips and other resources. Though most meds requiring storage at temperatures colder than room temperature should be stored in the refrigerator, expect to see a few meds require storage in the freezer. Some examples of medications requiring frozen storage conditions include: anthrax immune globulin (Anthrasil [U.S. only]), carmustine wafer (Gliadel [U.S. only]), cholera (live) vaccine (Vaxchora), dinoprostone vaginal insert (Cervidil), dinoprostone vaginal suppository (Prostin E2 [U.S.]), varicella vaccine (Varivax [U.S.]; Varivax III [Canada] can be stored in the refrigerator or freezer), zoster vaccine (Zostavax [U.S.]; Zostavax II [Canada] can be stored in the refrigerator or freezer). Use the list below to help identify medications requiring refrigerator storage and become familiar with acceptable temperature excursions from recommended storage conditions. Abbreviations: RT = room temperature Abaloparatide (Tymlos [U.S.]) Aflibercept (Eylea) Amphotericin B (Abelcet, Fungizone) • Once open, may store at RT (68°F to 77°F • May store at RT (77°F [25°C]) for up to Anakinra (Kineret) [20°C to 25°C]) for up to 30 days.