Treatment Resources for Opioid Use Disorder
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Medications to Treat Opioid Use Disorder Research Report
Research Report Revised Junio 2018 Medications to Treat Opioid Use Disorder Research Report Table of Contents Medications to Treat Opioid Use Disorder Research Report Overview How do medications to treat opioid use disorder work? How effective are medications to treat opioid use disorder? What are misconceptions about maintenance treatment? What is the treatment need versus the diversion risk for opioid use disorder treatment? What is the impact of medication for opioid use disorder treatment on HIV/HCV outcomes? How is opioid use disorder treated in the criminal justice system? Is medication to treat opioid use disorder available in the military? What treatment is available for pregnant mothers and their babies? How much does opioid treatment cost? Is naloxone accessible? References Page 1 Medications to Treat Opioid Use Disorder Research Report Discusses effective medications used to treat opioid use disorders: methadone, buprenorphine, and naltrexone. Overview An estimated 1.4 million people in the United States had a substance use disorder related to prescription opioids in 2019.1 However, only a fraction of people with prescription opioid use disorders receive tailored treatment (22 percent in 2019).1 Overdose deaths involving prescription opioids more than quadrupled from 1999 through 2016 followed by significant declines reported in both 2018 and 2019.2,3 Besides overdose, consequences of the opioid crisis include a rising incidence of infants born dependent on opioids because their mothers used these substances during pregnancy4,5 and increased spread of infectious diseases, including HIV and hepatitis C (HCV), as was seen in 2015 in southern Indiana.6 Effective prevention and treatment strategies exist for opioid misuse and use disorder but are highly underutilized across the United States. -
Understanding Addiction, Helping Clients and Colleagues
ALABAMA LAWYER ASSISTANCE PROGRAM Understanding Addiction, Helping Clients and Colleagues By Jeanne Marie Leslie rugs change the brain–they according to the American Bar change its structure and how it Association, is 15 to 18 percent.3 D works.1 Many of these changes Lawyers rank high in the incidences of are responsible for the behaviors we see depression compared to other professions in individuals addicted to drugs. and a disproportionate number of Neuroscience has made significant lawyers commit suicide;4 in Alabama advances in our ability to identify and there are about a dozen lawyer suicides understand the mechanisms involved in every year. And these are only the ones the addicted brain. These advancements about which we know. Many lawyers, clearly confirm what many in the addic- including some you know, may be strug- tion medicine field have known for some gling with an addiction or mental health time: the obsession and compulsion to problem when help is readily available use drugs in the addicted brain is instinc- through ALAP. tual and paramount to survival.2 Ignorance and stigma have contributed Addiction Facts to the confusion, moral judgments and Dr. Nora D. Volkow, director of the poor understanding of this destructive National Institute of Drug Abuse and often fatal disease. Our courts are (NIDA), explains how the neuro-chemi- overwhelmed by the behaviors, criminal cal mechanisms of drug abuse catalyze and civil, associated with addiction. and accelerate the onset addiction: Therefore, understanding addiction is “Recognizing drug addiction as a chron- essential for lawyers. Lawyers are in ic, relapsing disease characterized by com- unique positions to initiate change, to pulsive drug seeking and use is critical to advocate for medical treatment over tra- being able to identify and help those who ditional sanctions and to refer individuals have it. -

ASAM National Practice Guideline for the Treatment of Opioid Use Disorder: 2020 Focused Update
The ASAM NATIONAL The ASAM National Practice Guideline 2020 Focused Update Guideline 2020 Focused National Practice The ASAM PRACTICE GUIDELINE For the Treatment of Opioid Use Disorder 2020 Focused Update Adopted by the ASAM Board of Directors December 18, 2019. © Copyright 2020. American Society of Addiction Medicine, Inc. All rights reserved. Permission to make digital or hard copies of this work for personal or classroom use is granted without fee provided that copies are not made or distributed for commercial, advertising or promotional purposes, and that copies bear this notice and the full citation on the fi rst page. Republication, systematic reproduction, posting in electronic form on servers, redistribution to lists, or other uses of this material, require prior specifi c written permission or license from the Society. American Society of Addiction Medicine 11400 Rockville Pike, Suite 200 Rockville, MD 20852 Phone: (301) 656-3920 Fax (301) 656-3815 E-mail: [email protected] www.asam.org CLINICAL PRACTICE GUIDELINE The ASAM National Practice Guideline for the Treatment of Opioid Use Disorder: 2020 Focused Update 2020 Focused Update Guideline Committee members Kyle Kampman, MD, Chair (alpha order): Daniel Langleben, MD Chinazo Cunningham, MD, MS, FASAM Ben Nordstrom, MD, PhD Mark J. Edlund, MD, PhD David Oslin, MD Marc Fishman, MD, DFASAM George Woody, MD Adam J. Gordon, MD, MPH, FACP, DFASAM Tricia Wright, MD, MS Hendre´e E. Jones, PhD Stephen Wyatt, DO Kyle M. Kampman, MD, FASAM, Chair 2015 ASAM Quality Improvement Council (alpha order): Daniel Langleben, MD John Femino, MD, FASAM Marjorie Meyer, MD Margaret Jarvis, MD, FASAM, Chair Sandra Springer, MD, FASAM Margaret Kotz, DO, FASAM George Woody, MD Sandrine Pirard, MD, MPH, PhD Tricia E. -

What Are the Treatments for Heroin Addiction?
How is heroin linked to prescription drug abuse? See page 3. from the director: Research Report Series Heroin is a highly addictive opioid drug, and its use has repercussions that extend far beyond the individual user. The medical and social consequences of drug use—such as hepatitis, HIV/AIDS, fetal effects, crime, violence, and disruptions in family, workplace, and educational environments—have a devastating impact on society and cost billions of dollars each year. Although heroin use in the general population is rather low, the numbers of people starting to use heroin have been steadily rising since 2007.1 This may be due in part to a shift from abuse of prescription pain relievers to heroin as a readily available, cheaper alternative2-5 and the misperception that highly pure heroin is safer than less pure forms because it does not need to be injected. Like many other chronic diseases, addiction can be treated. Medications HEROIN are available to treat heroin addiction while reducing drug cravings and withdrawal symptoms, improving the odds of achieving abstinence. There are now a variety of medications that can be tailored to a person’s recovery needs while taking into account co-occurring What is heroin and health conditions. Medication combined with behavioral therapy is particularly how is it used? effective, offering hope to individuals who suffer from addiction and for those around them. eroin is an illegal, highly addictive drug processed from morphine, a naturally occurring substance extracted from the seed pod of certain varieties The National Institute on Drug Abuse (NIDA) has developed this publication to Hof poppy plants. -
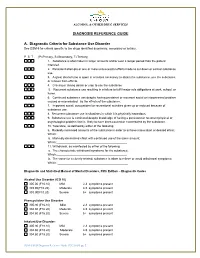
DIAGNOSIS REFERENCE GUIDE A. Diagnostic Criteria for Substance
ALCOHOL & OTHER DRUG SERVICES DIAGNOSIS REFERENCE GUIDE A. Diagnostic Criteria for Substance Use Disorder See DSM-5 for criteria specific to the drugs identified as primary, secondary or tertiary. P S T (P=Primary, S=Secondary, T=Tertiary) 1. Substance is often taken in larger amounts and/or over a longer period than the patient intended. 2. Persistent attempts or one or more unsuccessful efforts made to cut down or control substance use. 3. A great deal of time is spent in activities necessary to obtain the substance, use the substance, or recover from effects. 4. Craving or strong desire or urge to use the substance 5. Recurrent substance use resulting in a failure to fulfill major role obligations at work, school, or home. 6. Continued substance use despite having persistent or recurrent social or interpersonal problem caused or exacerbated by the effects of the substance. 7. Important social, occupational or recreational activities given up or reduced because of substance use. 8. Recurrent substance use in situations in which it is physically hazardous. 9. Substance use is continued despite knowledge of having a persistent or recurrent physical or psychological problem that is likely to have been caused or exacerbated by the substance. 10. Tolerance, as defined by either of the following: a. Markedly increased amounts of the substance in order to achieve intoxication or desired effect; Which:__________________________________________ b. Markedly diminished effect with continued use of the same amount; Which:___________________________________________ 11. Withdrawal, as manifested by either of the following: a. The characteristic withdrawal syndrome for the substance; Which:___________________________________________ b. -

Amphetamines Help People Struggling with Amphetamine Addiction
Reducing Harm & Finding Help, Continued detox facilities, and addiction treatment programs can help with withdrawal. Amphetamine addiction can be treated in a residential setting (often called “rehab”) or in an outpatient setting (when the patient lives at home, but goes to treatment appointments 1-7 times per week). Effective types of counseling for benzodiazepine addiction include cognitive behavioral therapy, motivational interviewing, and twelve- step facilitation. There are also recovery support groups and online forums that can Amphetamines help people struggling with amphetamine addiction. Narcotics Anonymous, Alcoholics Anonymous, and groups like SMART Recovery or LifeRing are all available to support people with Information about amphetamine addiction. Recovery apps specific to amphetamine addiction can be downloaded to your smart phone that Your Health provide lists of recovery support meetings, reading material, tools like sobriety counters, and more. © 2016 Institute for Research, Education and Training in Addictions Amphetamines – Amphetamines & who inject amphetamines and/or share equipment can develop injection site What Are They? My Health, Continued infections, damage to their veins, Hepatitis B & C, HIV, and blood clots. Amphetamines are a category of drug that decisions. For some people, amphetamine include prescription medications (like intoxication can create or worsen mental Adderall), methamphetamine (often illness symptoms like anxiety, paranoia, and shortened to “meth”), and MDMA (often hallucinations. called “ecstasy” or “Molly”). Although these drugs are not identical, they are all included Unknown drugs: Because some amphetamines in the category of amphetamines. are illegal, they carry additional risks. Users of methamphetamine and MDMA cannot be Amphetamines are stimulants. They can sure of the drug’s contents or dose. -
Molecular Mechanisms of Addiction
Molecular Mechanisms of Addiction Eric J. Nestler Nash Family Professor The Friedman Brain Institute Medical Model of Addiction • Pathophysiology - To identify changes that drugs produce in a vulnerable brain to cause addiction. • Individual Risk - To identify specific genes and non-genetic factors that determine an individual’s risk for (or resistance to) addiction. - About 50% of the risk for addiction is genetic. Only through an improved understanding of the biology of addiction will it be possible to develop better treatments and eventually cures and preventive measures. Scope of Drug Addiction • 25% of the U.S. population has a diagnosis of drug abuse or addiction. • 50% of U.S. high school graduates have tried an illegal drug; use of alcohol and tobacco is more common. • >$400 billion incurred annually in the U.S. by addiction: - Loss of life and productivity - Medical consequences (e.g., AIDS, lung cancer, cirrhosis) - Crime and law enforcement Diverse Chemical Substances Cause Addiction • Opiates (morphine, heroin, oxycontin, vicodin) • Cocaine • Amphetamine and like drugs (methamphetamine, methylphenidate) • MDMA (ecstasy) • PCP (phencyclidine or angel dust; also ketamine) • Marijuana (cannabinoids) • Tobacco (nicotine) • Alcohol (ethanol) • Sedative/hypnotics (barbiturates, benzodiazepines) Chemical Structures of Some Drugs of Abuse Cocaine Morphine Ethanol Nicotine ∆9-tetrahydrocannabinol Drugs of Abuse Use of % of US population as weekly users 100 25 50 75 0 Definition of Drug Addiction • Loss of control over drug use. • Compulsive drug seeking and drug taking despite horrendous adverse consequences. • Increased risk for relapse despite years of abstinence. Definition of Drug Addiction • Tolerance – reduced drug effect after repeated use. • Sensitization – increased drug effect after repeated use. -

Everything You Wanted to Know but May Have Been Afraid to Ask
Wellness Tip Sheet Maryland State Bar Association’s Lawyer Assistance Program Everything you wanted to know but may have been afraid to ask What is Sexual Addiction? According to Dr. Founder of the International Institute for Trauma and Addiction Professionals (IITAP), sexual addiction is defined as any sexually related compulsive behavior which interferes with normal living and causes severe stress on family, friends, loved ones, or one’s work environment. Sexual addiction is sometimes referred to as sexual dependency or sexual compulsivity. By any name it is a compulsive behavior that completely dominates the addict’s life. Sexual addicts make sex a priority, making it more important than family, friends and work. Sex becomes the organizing principle of addicts’ lives. They are willing to sacrifice what they cherish most in order to preserve and continue their unhealthy behavior. Background Information: • It is estimated that 3 to 6% of the US population suffer from sexual addiction. That’s about 17 to 37 million people • Although it has traditionally been considered a middle aged male dominant addiction, females now represent more than 20% of the affected population. • Sex addiction does not discriminate. It crosses all educational, socioeconomic, racial and sexual-orientation lines, but one commonality among addicts is a sense of shame. • There has been progress in the medical field which includes sexual addiction being diagnosed as a disorder and having treatment options available. • In the past ten years treatment options have gone from fewer than 100 therapists to over 1,500, with treatment centers specializing in sexual addiction. What Causes Sexual Addiction? Sexual addiction, just like any addiction, is very complex. -

Randomized Controlled Trial of Dexamphetamine Maintenance for the Treatment of Methamphetamine
RESEARCH REPORT doi:10.1111/j.1360-0443.2009.02717.x Randomized controlled trial of dexamphetamine maintenance for the treatment of methamphetamine dependenceadd_2717 146..154 Marie Longo1, Wendy Wickes1, Matthew Smout1, Sonia Harrison1, Sharon Cahill1 & Jason M. White1,2 Pharmacotherapies Research Unit, Drug and Alcohol Services South Australia, Norwood, South Australia, Australia1 and Discipline of Pharmacology, University of Adelaide, Adelaide, South Australia, Australia2 ABSTRACT Aim To investigate the safety and efficacy of once-daily supervised oral administration of sustained-release dexam- phetamine in people dependent on methamphetamine. Design Randomized, double-blind, placebo-controlled trial. Participants Forty-nine methamphetamine-dependent drug users from Drug and Alcohol Services South Australia (DASSA) clinics. Intervention Participants were assigned randomly to receive up to 110 mg/day sustained- release dexamphetamine (n = 23) or placebo (n = 26) for a maximum of 12 weeks, with gradual reduction of the study medication over an additional 4 weeks. Medication was taken daily under pharmacist supervision. Measurements Primary outcome measures included treatment retention, measures of methamphetamine consump- tion (self-report and hair analysis), degree of methamphetamine dependence and severity of methamphetamine withdrawal. Hair samples were analysed for methamphetamine using liquid chromatography-mass spectrometry. Findings Treatment retention was significantly different between groups, with those who received dexamphetamine remaining in treatment for an average of 86.3 days compared with 48.6 days for those receiving placebo (P = 0.014). There were significant reductions in self-reported methamphetamine use between baseline and follow-up within each group (P < 0.0001), with a trend to a greater reduction among the dexamphetamine group (P = 0.086). -
Parenting Children Who Have Been Exposed to Methamphetamine
Non-Return Information Packet Assisting families on their lifelong journey Parenting Children Who Have Been Exposed to Methamphetamine A Brief Guide for Adoptive, Guardianship, and Foster Parents Oregon Post Adoption Resource Center 2950 SE Stark Street, Suite 130 Portland, Oregon 97214 503-241-0799 800-764-8367 503-241-0925 Fax [email protected] www.orparc.org ORPARC is a contracted service of the Oregon Department of Human Services. Please do not reproduce without permission. PARENTING CHILDREN WHO HAVE BEEN EXPOSED TO METHAMPHETAMINE A BRIEF GUIDE FOR ADOPTIVE, GUARDIANSHIP AND FOSTER PARENTS Table of Contents Introduction: ............................................................................................................. 1 Part I: Methamphetamine: An Overview ........................................................... 2 What is meth? What are its effects on the user? How prevalent is meth use? How is meth addiction treated? Part II: Meth’s Effects on Children ...................................................................... 7 What are the prenatal effects of exposure? What are the postnatal effects of prenatal exposure? What are the environmental effects on children? Part III: Parenting Meth-Exposed Children ....................................................... 11 Guiding principles Age-specific suggestions Part IV: Reprinted Articles .................................................................................. 20 Appendix A: Recommended Resources Appendix B: Sources Page i PARENTING CHILDREN WHO HAVE -

Cognitive Behavioral Therapy for Substance Use Disorders Among Veterans
Cognitive Behavioral Therapy for Substance Use Disorders Among Veterans Therapist Manual Josephine M. DeMarce, Ph.D. Maryann Gnys, Ph.D. Susan D. Raffa, Ph.D. Bradley E. Karlin, Ph.D. Cognitive Behavioral Therapy for Substance Use Disorders Among Veterans Therapist Manual Suggested Citation: DeMarce, J. M., Gnys, M., Raffa, S. D., & Karlin, B. E. (2014). Cognitive Behavioral Therapy for Substance Use Disorders Among Veterans: Therapist Manual. Washington, DC: U.S. Department of Veterans Affairs. Table of Contents Table of Figures ..............................................................................................................................................vii Acknowledgements .......................................................................................................................................... ix Preface ............................................................................................................................................................... x Part 1: Background, Theory, Case Conceptualization, and Treatment Structure ....................1 Introduction ....................................................................................................................................................... 2 What is Cognitive Behavioral Therapy? ........................................................................................................ 2 About the Manual ......................................................................................................................................... -
Pharmacotherapy for Methamphetamine Dependence: A
Annals of Clinical Psychiatry, 20[3]:145–155, 2008 Copyright © American Academy of Clinical Psychiatrists ISSN: 1040-1237 print / 1547-3325 online DOI: 10.1080/10401230802177656 PharmacotherapyUACP for Methamphetamine Dependence: A Review of the Pathophysiology of Methamphetamine Addiction and the Theoretical Basis and Efficacy of Pharmacotherapeutic Interventions MARKPharmacotherapy For Methamphetamine E. Dependence ROSE Licensed Psychologist, Private Practice and North Central Medical Communications, Inc., St. Paul, Minnesota, USA JON E. GRANT Department of Psychiatry, University of Minnesota, Minneapolis, Minnesota, USA Background. Methamphetamine (METH) dependence is a significant public health, criminal justice, and social service concern, and although abuse of this drug spans the past 40 years in the U.S., effective treatments have only recently been developed and evaluated. Psychosocial therapies comprise the mainstay of treatment, yet many patients experience ongoing impairments in mood, cognition, emotional control, and motivation, suggesting a role for pharmacotherapy. Methods. A search of the literature was performed to identify drug therapies utilized with METH dependent patients and the outcome of these trials. Results. With the exception of bupropion, most trials employing direct monoamine agonists yielded negative or inclusive results, a counterintuitive finding. Positive results were produced by a trial of the mixed monoamine agonist/antagonist mirtazapine and by several studies employing indirect dopamine- and glutamate-modulating