The Cerebral Circulation Second Edition Ii
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Endovascular Treatment of Stroke Caused by Carotid Artery Dissection
brain sciences Case Report Endovascular Treatment of Stroke Caused by Carotid Artery Dissection Grzegorz Meder 1,* , Milena Swito´ ´nska 2,3 , Piotr Płeszka 2, Violetta Palacz-Duda 2, Dorota Dzianott-Pabijan 4 and Paweł Sokal 3 1 Department of Interventional Radiology, Jan Biziel University Hospital No. 2, Ujejskiego 75 Street, 85-168 Bydgoszcz, Poland 2 Stroke Intervention Centre, Department of Neurosurgery and Neurology, Jan Biziel University Hospital No. 2, Ujejskiego 75 Street, 85-168 Bydgoszcz, Poland; [email protected] (M.S.);´ [email protected] (P.P.); [email protected] (V.P.-D.) 3 Department of Neurosurgery and Neurology, Faculty of Health Sciences, Nicolaus Copernicus University in Toru´n,Ludwik Rydygier Collegium Medicum, Ujejskiego 75 Street, 85-168 Bydgoszcz, Poland; [email protected] 4 Neurological Rehabilitation Ward Kuyavian-Pomeranian Pulmonology Centre, Meysnera 9 Street, 85-472 Bydgoszcz, Poland; [email protected] * Correspondence: [email protected]; Tel.: +48-52-3655-143; Fax: +48-52-3655-364 Received: 23 September 2020; Accepted: 27 October 2020; Published: 30 October 2020 Abstract: Ischemic stroke due to large vessel occlusion (LVO) is a devastating condition. Most LVOs are embolic in nature. Arterial dissection is responsible for only a small proportion of LVOs, is specific in nature and poses some challenges in treatment. We describe 3 cases where patients with stroke caused by carotid artery dissection were treated with mechanical thrombectomy and extensive stenting with good outcome. We believe that mechanical thrombectomy and stenting is a treatment of choice in these cases. Keywords: stroke; artery dissection; endovascular treatment; stenting; mechanical thrombectomy 1. -

Download PDF File
ONLINE FIRST This is a provisional PDF only. Copyedited and fully formatted version will be made available soon. ISSN: 0015-5659 e-ISSN: 1644-3284 Two cases of combined anatomical variations: maxillofacial trunk, vertebral, posterior communicating and anterior cerebral atresia, linguofacial and labiomental trunks Authors: M. C. Rusu, A. M. Jianu, M. D. Monea, A. C. Ilie DOI: 10.5603/FM.a2021.0007 Article type: Case report Submitted: 2020-11-28 Accepted: 2021-01-08 Published online: 2021-01-29 This article has been peer reviewed and published immediately upon acceptance. It is an open access article, which means that it can be downloaded, printed, and distributed freely, provided the work is properly cited. Articles in "Folia Morphologica" are listed in PubMed. Powered by TCPDF (www.tcpdf.org) Two cases of combined anatomical variations: maxillofacial trunk, vertebral, posterior communicating and anterior cerebral atresia, linguofacial and labiomental trunks M.C. Rusu et al., The maxillofacial trunk M.C. Rusu1, A.M. Jianu2, M.D. Monea2, A.C. Ilie3 1Division of Anatomy, Faculty of Dental Medicine, “Carol Davila” University of Medicine and Pharmacy, Bucharest, Romania 2Department of Anatomy, Faculty of Medicine, “Victor Babeş” University of Medicine and Pharmacy, Timişoara, Romania 3Department of Functional Sciences, Discipline of Public Health, Faculty of Medicine, “Victor Babes” University of Medicine and Pharmacy, Timisoara, Romania Address for correspondence: M.C. Rusu, MD, PhD (Med.), PhD (Biol.), Dr. Hab., Prof., Division of Anatomy, Faculty of Dental Medicine, “Carol Davila” University of Medicine and Pharmacy, 8 Eroilor Sanitari Blvd., RO-76241, Bucharest, Romania, , tel: +40722363705 e-mail: [email protected] ABSTRACT Background: Commonly, arterial anatomic variants are reported as single entities. -

Mechanical Thrombectomy in Basilar Artery Occlusion Presence of Bilateral Posterior Communicating Arteries Is a Predictor of Favorable Clinical Outcome
Clin Neuroradiol (2019) 29:153–160 https://doi.org/10.1007/s00062-017-0651-3 ORIGINAL ARTICLE Mechanical Thrombectomy in Basilar Artery Occlusion Presence of Bilateral Posterior Communicating Arteries is a Predictor of Favorable Clinical Outcome Volker Maus 1 ·AlevKalkan1 · Christoph Kabbasch1 · Nuran Abdullayev1 · Henning Stetefeld2 · Utako Birgit Barnikol3 · Thomas Liebig4 · Christian Dohmen2 · Gereon Rudolf Fink2,5 · Jan Borggrefe1 · Anastasios Mpotsaris6 Received: 17 August 2017 / Accepted: 21 November 2017 / Published online: 19 December 2017 © Springer-Verlag GmbH Germany, part of Springer Nature 2017 Abstract Results The favorable clinical outcome at 90 days was 25% Background Mechanical thrombectomy (MT) of basilar and mortality was 43%. The rate of successful reperfusion, artery occlusions (BAO) is a subject of debate. We inves- i.e. modified thrombolysis in cerebral infarction (mTICI) ≥ tigated the clinical outcome of MT in BAO and predictors 2b was 82%. Presence of bilateral PcoAs (area under the of a favorable outcome. curve, AUC: 0.81, odds ratio, OR: 4.2, 2.2–8.2; p < 0.0001), Material and Methods A total of 104 MTs of BAO (carried lower National Institute of Health Stroke Scale (NIHSS) out between 2010 and 2016) were analyzed. Favorable out- on admission (AUC: 0.74, OR: 2.6, 1.3–5.2; p < 0.01), PC- come as a modified Rankin scale (mRS) Ä 2at90days ASPECTS ≥ 9 (AUC: 0.72, OR: 4.2, 1.5–11.9; p < 0.01), was the primary endpoint. The influence of the follow- incomplete BAO (AUC: 0.66, OR: 2.6, 1.4–4.8; p < 0.001), ing variables on outcome was investigated: number of de- and basilar tip patency (AUC: 0.66, OR: 2.5, 1.3–4.8; p < tectable posterior communicating arteries (PcoAs), patency 0.01) were associated with a favorable outcome. -

Dural Venous Channels: Hidden in Plain Sight–Reassessment of an Under-Recognized Entity
Published July 16, 2020 as 10.3174/ajnr.A6647 ORIGINAL RESEARCH INTERVENTIONAL Dural Venous Channels: Hidden in Plain Sight–Reassessment of an Under-Recognized Entity M. Shapiro, K. Srivatanakul, E. Raz, M. Litao, E. Nossek, and P.K. Nelson ABSTRACT BACKGROUND AND PURPOSE: Tentorial sinus venous channels within the tentorium cerebelli connecting various cerebellar and su- pratentorial veins, as well as the basal vein, to adjacent venous sinuses are a well-recognized entity. Also well-known are “dural lakes” at the vertex. However, the presence of similar channels in the supratentorial dura, serving as recipients of the Labbe, super- ficial temporal, and lateral and medial parieto-occipital veins, among others, appears to be underappreciated. Also under-recog- nized is the possible role of these channels in the angioarchitecture of certain high-grade dural fistulas. MATERIALS AND METHODS: A retrospective review of 100 consecutive angiographic studies was performed following identification of index cases to gather data on the angiographic and cross-sectional appearance, location, length, and other features. A review of 100 consecutive dural fistulas was also performed to identify those not directly involving a venous sinus. RESULTS: Supratentorial dural venous channels were found in 26% of angiograms. They have the same appearance as those in the tentorium cerebelli, a flattened, ovalized morphology owing to their course between 2 layers of the dura, in contradistinction to a rounded cross-section of cortical and bridging veins. They are best appreciated on angiography and volumetric postcontrast T1- weighted images. Ten dural fistulas not directly involving a venous sinus were identified, 6 tentorium cerebelli and 4 supratentorial. -

Cerebellar Disease in the Dog and Cat
CEREBELLAR DISEASE IN THE DOG AND CAT: A LITERATURE REVIEW AND CLINICAL CASE STUDY (1996-1998) b y Diane Dali-An Lu BVetMed A thesis submitted for the degree of Master of Veterinary Medicine (M.V.M.) In the Faculty of Veterinary Medicine University of Glasgow Department of Veterinary Clinical Studies Division of Small Animal Clinical Studies University of Glasgow Veterinary School A p ril 1 9 9 9 © Diane Dali-An Lu 1999 ProQuest Number: 13815577 All rights reserved INFORMATION TO ALL USERS The quality of this reproduction is dependent upon the quality of the copy submitted. In the unlikely event that the author did not send a com plete manuscript and there are missing pages, these will be noted. Also, if material had to be removed, a note will indicate the deletion. uest ProQuest 13815577 Published by ProQuest LLC(2018). Copyright of the Dissertation is held by the Author. All rights reserved. This work is protected against unauthorized copying under Title 17, United States C ode Microform Edition © ProQuest LLC. ProQuest LLC. 789 East Eisenhower Parkway P.O. Box 1346 Ann Arbor, Ml 48106- 1346 GLASGOW UNIVERSITY lib ra ry ll5X C C ^ Summary SUMMARY________________________________ The aim of this thesis is to detail the history, clinical findings, ancillary investigations and, in some cases, pathological findings in 25 cases of cerebellar disease in dogs and cats which were presented to Glasgow University Veterinary School and Hospital during the period October 1996 to June 1998. Clinical findings were usually characteristic, although the signs could range from mild tremor and ataxia to severe generalised ataxia causing frequent falling over and difficulty in locomotion. -

THE SYNDROMES of the ARTERIES of the BRAIN AND, SPINAL CORD Part II by LESLIE G
I19 Postgrad Med J: first published as 10.1136/pgmj.29.329.119 on 1 March 1953. Downloaded from - N/ THE SYNDROMES OF THE ARTERIES OF THE BRAIN AND, SPINAL CORD Part II By LESLIE G. KILOH, M.D., M.R.C.P., D.P.M. First Assistant in the Joint Department of Psychological Medicine, Royal Victoria Infirmary and University of Durham The Vertebral Artery (See also Cabot, I937; Pines and Gilensky, Each vertebral artery enters the foramen 1930.) magnum in front of the roots of the hypoglossal nerve, inclines forwards and medially to the The Posterior Inferior Cerebellar Artery anterior aspect of the medulla oblongata and unites The posterior inferior cerebellar artery arises with its fellow at the lower border of the pons to from the vertebral artery at the level of the lower form the basilar artery. border of the inferior olive and winds round the The posterior inferior cerebellar and the medulla oblongata between the roots of the hypo- Protected by copyright. anterior spinal arteries are its principal branches glossal nerve. It passes rostrally behind the root- and it sometimes gives off the posterior spinal lets of the vagus and glossopharyngeal nerves to artery. A few small branches are supplied directly the lower border of the pons, bends backwards and to the medulla oblongata. These are in line below caudally along the inferolateral boundary of the with similar branches of the anterior spinal artery fourth ventricle and finally turns laterally into the and above with the paramedian branches of the vallecula. basilar artery. Branches: From the trunk of the artery, In some cases of apparently typical throm- twigs enter the lateral aspect of the medulla bosis of the posterior inferior cerebellar artery, oblongata and supply the region bounded ventrally post-mortem examination has demonstrated oc- by the inferior olive and medially by the hypo- clusion of the entire vertebral artery (e.g., Diggle glossal nucleus-including the nucleus ambiguus, and Stcpford, 1935). -

SŁOWNIK ANATOMICZNY (ANGIELSKO–Łacinsłownik Anatomiczny (Angielsko-Łacińsko-Polski)´ SKO–POLSKI)
ANATOMY WORDS (ENGLISH–LATIN–POLISH) SŁOWNIK ANATOMICZNY (ANGIELSKO–ŁACINSłownik anatomiczny (angielsko-łacińsko-polski)´ SKO–POLSKI) English – Je˛zyk angielski Latin – Łacina Polish – Je˛zyk polski Arteries – Te˛tnice accessory obturator artery arteria obturatoria accessoria tętnica zasłonowa dodatkowa acetabular branch ramus acetabularis gałąź panewkowa anterior basal segmental artery arteria segmentalis basalis anterior pulmonis tętnica segmentowa podstawna przednia (dextri et sinistri) płuca (prawego i lewego) anterior cecal artery arteria caecalis anterior tętnica kątnicza przednia anterior cerebral artery arteria cerebri anterior tętnica przednia mózgu anterior choroidal artery arteria choroidea anterior tętnica naczyniówkowa przednia anterior ciliary arteries arteriae ciliares anteriores tętnice rzęskowe przednie anterior circumflex humeral artery arteria circumflexa humeri anterior tętnica okalająca ramię przednia anterior communicating artery arteria communicans anterior tętnica łącząca przednia anterior conjunctival artery arteria conjunctivalis anterior tętnica spojówkowa przednia anterior ethmoidal artery arteria ethmoidalis anterior tętnica sitowa przednia anterior inferior cerebellar artery arteria anterior inferior cerebelli tętnica dolna przednia móżdżku anterior interosseous artery arteria interossea anterior tętnica międzykostna przednia anterior labial branches of deep external rami labiales anteriores arteriae pudendae gałęzie wargowe przednie tętnicy sromowej pudendal artery externae profundae zewnętrznej głębokiej -

High-Yield Neuroanatomy, FOURTH EDITION
LWBK110-3895G-FM[i-xviii].qxd 8/14/08 5:57 AM Page i Aptara Inc. High-Yield TM Neuroanatomy FOURTH EDITION LWBK110-3895G-FM[i-xviii].qxd 8/14/08 5:57 AM Page ii Aptara Inc. LWBK110-3895G-FM[i-xviii].qxd 8/14/08 5:57 AM Page iii Aptara Inc. High-Yield TM Neuroanatomy FOURTH EDITION James D. Fix, PhD Professor Emeritus of Anatomy Marshall University School of Medicine Huntington, West Virginia With Contributions by Jennifer K. Brueckner, PhD Associate Professor Assistant Dean for Student Affairs Department of Anatomy and Neurobiology University of Kentucky College of Medicine Lexington, Kentucky LWBK110-3895G-FM[i-xviii].qxd 8/14/08 5:57 AM Page iv Aptara Inc. Acquisitions Editor: Crystal Taylor Managing Editor: Kelley Squazzo Marketing Manager: Emilie Moyer Designer: Terry Mallon Compositor: Aptara Fourth Edition Copyright © 2009, 2005, 2000, 1995 Lippincott Williams & Wilkins, a Wolters Kluwer business. 351 West Camden Street 530 Walnut Street Baltimore, MD 21201 Philadelphia, PA 19106 Printed in the United States of America. All rights reserved. This book is protected by copyright. No part of this book may be reproduced or transmitted in any form or by any means, including as photocopies or scanned-in or other electronic copies, or utilized by any information storage and retrieval system without written permission from the copyright owner, except for brief quotations embodied in critical articles and reviews. Materials appearing in this book prepared by individuals as part of their official duties as U.S. government employees are not covered by the above-mentioned copyright. To request permission, please contact Lippincott Williams & Wilkins at 530 Walnut Street, Philadelphia, PA 19106, via email at [email protected], or via website at http://www.lww.com (products and services). -

Special Report Vein of Galen Aneurysms
Special Report Vein of Galen Aneurysms: A Review and Current Perspective Michael Bruce Horowitz, Charles A. Jungreis, Ronald G. Quisling, and lan Pollack The term vein of Galen aneurysm encom the internal cerebral vein to form the vein of passes a diverse group of vascular anomalies Galen (4). sharing a common feature, dilatation of the vein Differentiation of the venous sinuses occurs of Galen. The name, therefore, is a misnomer. concurrently with development of arterial and Although some investigators speculate that vein venous drainage systems. By week 4, a primi of Galen aneurysms comprise up to 33% of gi tive capillary network is drained by anterior, ant arteriovenous malformations in infancy and middle, and posterior meningeal plexi (3, 4). childhood ( 1), the true incidence of this a nom Each plexus has a stem that drains into one of aly remains uncertain. A review of the literature the paired longitudinal head sinuses, which in reveals fewer than 300 reported cases since turn drain into the jugular veins ( 3, 4). Atresia of Jaeger et al 's clinical description in 1937 (2). the longitudinal sinuses leads to the develop As we will outline below, our understanding of ment of the transverse and sigmoid sinuses by the embryology, anatomy, clinical presentation, week 7 (3, 4). At birth only the superior and and management of these difficult vascular inferior sagittal, straight, transverse, occipital, malformations has progressed significantly and sigmoid sinuses remain, along with a still over the past 50 years. plexiform torcula (3, 4). On occasion, a tran sient falcine sinus extending from the vein of Embryology and Vascular Anatomy of the Galen to the superior sagittal sinus is seen ( 4). -
27. Veins of the Head and Neck
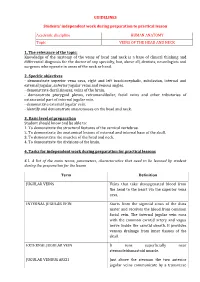
GUIDELINES Students’ independent work during preparation to practical lesson Academic discipline HUMAN ANATOMY Topic VEINS OF THE HEAD AND NECK 1. The relevance of the topic: Knowledge of the anatomy of the veins of head and neck is a base of clinical thinking and differential diagnosis for the doctor of any specialty, but, above all, dentists, neurologists and surgeons who operate in areas of the neck or head. 2. Specific objectives - demonstrate superior vena cava, right and left brachiocephalic, subclavian, internal and external jugular, anterior jugular veins and venous angles. - demonstrate dural sinuses, veins of the brain. - demonstrate pterygoid plexus, retromandibular, facial veins and other tributaries of extracranial part of internal jugular vein. - demonstrate external jugular vein. - identify and demonstrate anastomoses on the head and neck. 3. Basic level of preparation Student should know and be able to: 1. To demonstrate the structural features of the cervical vertebrae. 2. To demonstrate the anatomical lesions of external and internal base of the skull. 3. To demonstrate the muscles of the head and neck. 4. To demonstrate the divisions of the brain. 4. Tasks for independent work during preparation for practical lessons 4.1. A list of the main terms, parameters, characteristics that need to be learned by student during the preparation for the lesson Term Definition JUGULAR VEINS Veins that take deoxygenated blood from the head to the heart via the superior vena cava. INTERNAL JUGULAR VEIN Starts from the sigmoid sinus of the dura mater and receives the blood from common facial vein. The internal jugular vein runs with the common carotid artery and vagus nerve inside the carotid sheath. -

Vascularization of the Alouatta Belzebul Brain Base1 Dayane Kelly Sabec-Pereira2*, Fabiano C
Pesq. Vet. Bras. 40(4):315-323, April 2020 DOI: 10.1590/1678-5150-PVB-6536 Original Article Animal Morphophysiology ISSN 0100-736X (Print) ISSN 1678-5150 (Online) PVB-6536 MF Vascularization of the Alouatta belzebul brain base1 Dayane Kelly Sabec-Pereira2*, Fabiano C. Lima3, Fabiano R. Melo4, Fabiana Cristina S.A. Melo4, Kleber Fernando Pereira5 and Valcinir Aloisio S. Vulcani2.3 ABSTRACT.- Sabec-Pereira D.K., Lima F.C., Melo F.R., Melo F.C.S.A., Pereira K.F. & Vulcani V.A.S. 2020. Vascularization of the Alouatta belzebul brain base. Pesquisa Veterinária Brasileira 40(4):315-323. Escola de Veterinária e Zootecnia, Universidade Federal de Goiás, Avenida Esperança s/n, Campus Samambaia, Goiânia, GO 74690-900, Brazil. E-mail: [email protected] Alouatta belzebul primate. The material had the arterial system perfused (water at 40°C), injected with stained We studied the arterial circle in the brain of five specimens of the Título Original latexthe vertebra-basilar (Neoprene 650), and fixed the carotidin aqueous ones, formaldehyde which anastomose solution to close (10%) the andarterial dissected circuit. for In vesselthe caudal verification. portion ofThe the arterial arterial circle circle, of therethis primate are the isvertebral composed arteries of two and vascular their branches: systems: the rostral spinal artery and the caudal inferior cerebellar artery. The anastomosis of the [Título traduzido]. vertebral arteries gives rise to the basilar artery. It presented an anatomical variation at the beginning of its path, forming a double basilar artery, called arterial island. In its course, it emitted branches giving rise to the rostral inferior cerebellar artery, the pontine arteries, the rostral cerebellar arteries, the satellite rostral cerebellar arteries and its terminal branch, Autores the caudal cerebral artery, which presented itself in two segments: the pre-communicating one and post-communicating, joining the internal carotid artery and originating the caudal communicating artery. -

Controversies in the Assessment of Bodily Injury. Institute of Legal Medicine of Catalonia
Controversies in the assessment of bodily injury. Institute of Legal Medicine of Catalonia Centre d’Estudis Jurídics i Formació Especialitzada Institut de Medicina Legal de Catalunya Acknowledgement As ever the contribution of senior management at the Centre for Legal Studies and Specialised Training and the highly professional staff at the Centre’s Legal and Forensic Training Unit has been essen- tial and made it possible to publish the papers about the controversial issues presented below. I would also like to express my appreciation for the enthusiastic collaboration of all the authors referred to in their relevant sections and the computer support provided by Mr. Gabriel Martí Agustí, a psychologist in the Barcelona Forensic Medicine Clin- ic Service, which has made it possible to unify the work of the various authors. All of this has been done at the Institute of Legal Medicine of Catalonia under the supervision of Dr. Jordi Medallo Muñiz who has encouraged, supported and taken part in this project. Finally I would like to mention in particular the ongoing assistance of Dr. Amadeu Pu- jol Robinat, Head of the Forensic Medicine Clinic Service of IMLC. My sincere thanks go to all of them. Dr. Lluïsa Puig Coordinator CONTROVERSIES IN THE ASSESSMENT OF BODILY INJURY. INSTITUTE OF LEGAL MEDICINE OF CATALONIA COORDINATION: DRA. LLUÏSA PUIG BAUSILI Centre d’Estudis Jurídics i Formació Especialitzada Institut de Medicina Legal de Catalunya CONTROVERSIES IN THE ASSESSMENT OF BODILY INJURY. INSTITUTE OF LEGAL MEDICINE OF CATALONIA Centre d’Estudis Jurídics i Formació Especialitzada Institut de Medicina Legal de Catalunya 5 © Generalitat de Catalunya Centre d’Estudis Jurídics i Formació Especialitzada Disclaimer: The contents of this work are licensed under a Attribution-NonCommercial- NoDerivs 3.0 Creative Commons.