The Glucagon Receptor As a Drug Target
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

The Activation of the Glucagon-Like Peptide-1 (GLP-1) Receptor by Peptide and Non-Peptide Ligands
The Activation of the Glucagon-Like Peptide-1 (GLP-1) Receptor by Peptide and Non-Peptide Ligands Clare Louise Wishart Submitted in accordance with the requirements for the degree of Doctor of Philosophy of Science University of Leeds School of Biomedical Sciences Faculty of Biological Sciences September 2013 I Intellectual Property and Publication Statements The candidate confirms that the work submitted is her own and that appropriate credit has been given where reference has been made to the work of others. This copy has been supplied on the understanding that it is copyright material and that no quotation from the thesis may be published without proper acknowledgement. The right of Clare Louise Wishart to be identified as Author of this work has been asserted by her in accordance with the Copyright, Designs and Patents Act 1988. © 2013 The University of Leeds and Clare Louise Wishart. II Acknowledgments Firstly I would like to offer my sincerest thanks and gratitude to my supervisor, Dr. Dan Donnelly, who has been nothing but encouraging and engaging from day one. I have thoroughly enjoyed every moment of working alongside him and learning from his guidance and wisdom. My thanks go to my academic assessor Professor Paul Milner whom I have known for several years, and during my time at the University of Leeds he has offered me invaluable advice and inspiration. Additionally I would like to thank my academic project advisor Dr. Michael Harrison for his friendship, help and advice. I would like to thank Dr. Rosalind Mann and Dr. Elsayed Nasr for welcoming me into the lab as a new PhD student and sharing their experimental techniques with me, these techniques have helped me no end in my time as a research student. -

Structure-Function of the Glucagon Receptor Family of G Protein–Coupled Receptors: the Glucagon, GIP, GLP-1, and GLP-2 Receptors
Receptors and Channels, 8:179–188, 2002 Copyright c 2002 Taylor & Francis 1060-6823/02 $12.00 + .00 DOI: 10.1080/10606820290005155 Structure-Function of the Glucagon Receptor Family of G Protein–Coupled Receptors: The Glucagon, GIP, GLP-1, and GLP-2 Receptors P. L. Brubaker Departments of Physiology and Medicine, University of Toronto, Toronto, Ontario, Canada D. J. Drucker Department of Medicine, Banting and Best Diabetes Centre, Toronto General Hospital, Toronto, Ontario, Canada convertases results in the liberation of glucagon in the pancreatic The glucagon-like peptides include glucagon, GLP-1, and A cell, and GLP-1 and GLP-2 in the intestinal L cell and brain GLP-2, and exert diverse actions on nutrient intake, gastrointesti- (Mojsov et al. 1986; Orskov et al. 1987). As discussed below, nal motility, islet hormone secretion, cell proliferation and apopto- all three proglucagon-derived peptides (PGDPs) play impor- sis, nutrient absorption, and nutrient assimilation. GIP, a related member of the glucagon peptide superfamily, also regulates nutri- tant roles in the physiologic regulation of nutrient homeosta- ent disposal via stimulation of insulin secretion. The actions of these sis, through effects on energy intake and satiety, nutrient fluxes peptides are mediated by distinct members of the glucagon recep- through and across the gastrointestinal tract, and energy as- tor superfamily of G protein–coupled receptors. These receptors similation. Several of these biological activities are shared by exhibit unique patterns of tissue-specific expression, exhibit consid- a fourth glucagon-related peptide hormone, glucose-dependent erable amino acid sequence identity, and share similar structural and functional properties with respect to ligand binding and sig- insulinotropic peptide (GIP) (Table 1). -

Current Topics in Medicinal Chemistry, 2019, 19, 1399-1417 REVIEW ARTICLE
Send Orders for Reprints to [email protected] 1399 Current Topics in Medicinal Chemistry, 2019, 19, 1399-1417 REVIEW ARTICLE ISSN: 1568-0266 eISSN: 1873-4294 Impact Factor: Targeting the PAC1 Receptor for Neurological and Metabolic Disorders 3.442 The international journal for in-depth reviews on Current Topics in Medicinal Chemistry BENTHAM SCIENCE Chenyi Liao1, Mathilde P. de Molliens2, Severin T. Schneebeli1, Matthias Brewer1, Gaojie Song3, David Chatenet2, Karen M. Braas4, Victor May4,* and Jianing Li1,* 1Department of Chemistry, University of Vermont, Burlington, VT 05405, USA; 2INRS – Institut Armand-Frappier, 531 boul. des Prairies, Laval, QC H7V 1B7, Canada; 3Shanghai Key Laboratory of Regulatory Biology, Institute of Bio- medical Sciences and School of Life Sciences, East China Normal University, Shanghai, 200241, P.R. China; 4Department of Neurological Sciences, University of Vermont, Larner College of Medicine, 149 Beaumont Avenue, Bur- lington, VT 05405, USA Abstract: The pituitary adenylate cyclase-activating polypeptide (PACAP)-selective PAC1 receptor (PAC1R, ADCYAP1R1) is a member of the vasoactive intestinal peptide (VIP)/secretin/glucagon fam- ily of G protein-coupled receptors (GPCRs). PAC1R has been shown to play crucial roles in the central and peripheral nervous systems. The activation of PAC1R initiates diverse downstream signal transduc- tion pathways, including adenylyl cyclase, phospholipase C, MEK/ERK, and Akt pathways that regu- late a number of physiological systems to maintain functional homeostasis. Accordingly, at times of tissue injury or insult, PACAP/PAC1R activation of these pathways can be trophic to blunt or delay apoptotic events and enhance cell survival. Enhancing PAC1R signaling under these conditions has the potential to mitigate cellular damages associated with cerebrovascular trauma (including stroke), neu- A R T I C L E H I S T O R Y rodegeneration (such as Parkinson’s and Alzheimer's disease), or peripheral organ insults. -

Glucagon-Like Peptide-1 and Its Class BG Protein–Coupled Receptors
1521-0081/68/4/954–1013$25.00 http://dx.doi.org/10.1124/pr.115.011395 PHARMACOLOGICAL REVIEWS Pharmacol Rev 68:954–1013, October 2016 Copyright © 2016 by The Author(s) This is an open access article distributed under the CC BY-NC Attribution 4.0 International license. ASSOCIATE EDITOR: RICHARD DEQUAN YE Glucagon-Like Peptide-1 and Its Class B G Protein–Coupled Receptors: A Long March to Therapeutic Successes Chris de Graaf, Dan Donnelly, Denise Wootten, Jesper Lau, Patrick M. Sexton, Laurence J. Miller, Jung-Mo Ahn, Jiayu Liao, Madeleine M. Fletcher, Dehua Yang, Alastair J. H. Brown, Caihong Zhou, Jiejie Deng, and Ming-Wei Wang Division of Medicinal Chemistry, Faculty of Sciences, Vrije Universiteit Amsterdam, Amsterdam, The Netherlands (C.d.G.); School of Biomedical Sciences, University of Leeds, Leeds, United Kingdom (D.D.); Drug Discovery Biology Theme and Department of Pharmacology, Monash Institute of Pharmaceutical Sciences, Parkville, Victoria, Australia (D.W., P.M.S., M.M.F.); Protein and Peptide Chemistry, Global Research, Novo Nordisk A/S, Måløv, Denmark (J.La.); Department of Molecular Pharmacology and Experimental Therapeutics, Mayo Clinic, Scottsdale, Arizona (L.J.M.); Department of Chemistry and Biochemistry, University of Texas at Dallas, Richardson, Texas (J.-M.A.); Department of Bioengineering, Bourns College of Engineering, University of California at Riverside, Riverside, California (J.Li.); National Center for Drug Screening and CAS Key Laboratory of Receptor Research, Shanghai Institute of Materia Medica, Chinese Academy of Sciences, Shanghai, China (D.Y., C.Z., J.D., M.-W.W.); Heptares Therapeutics, BioPark, Welwyn Garden City, United Kingdom (A.J.H.B.); and School of Pharmacy, Fudan University, Zhangjiang High-Tech Park, Shanghai, China (M.-W.W.) Downloaded from Abstract. -

Gpcrs Globally Coevolved with Receptor Activity-Modifying Proteins, Ramps
GPCRs globally coevolved with receptor activity-modifying proteins, RAMPs Shahar Barbasha, Emily Lorenzena, Torbjörn Perssona,b, Thomas Hubera,1, and Thomas P. Sakmara,b,1 aLaboratory of Chemical Biology and Signal Transduction, The Rockefeller University, New York, NY, 10065; and bDepartment of Neurobiology, Care Sciences and Society, Division for Neurogeriatrics, Center for Alzheimer Research, Karolinska Institutet, 141 57 Huddinge, Sweden Edited by Andrew C. Kruse, Harvard University, and accepted by Editorial Board Member K. C. Garcia September 28, 2017 (received for review July 22, 2017) Receptor activity-modifying proteins (RAMPs) are widely expressed between the two. Therefore, highly coevolved protein pairs could in human tissues and, in some cases, have been shown to affect be members in the same pathway, or they could be components surface expression or ligand specificity of G-protein–coupled recep- of the same complex. tors (GPCRs). However, whether RAMP−GPCR interactions are wide- Previously, several cases of coevolution of receptor genes and spread, and the nature of their functional consequences, remains their endogenous protein−ligand genes were reported (13), but largely unknown. In humans, there are three RAMPs and over large-scale coevolution of different signal transduction components 800 expressed GPCRs, making direct experimental approaches chal- was not examined. Phylogenetic analysis to conclude coevolution lenging. We analyzed relevant genomic data from all currently avail- could be implemented by two complementary approaches. The able sequenced organisms. We discovered that RAMPs and GPCRs first searches for ortholog genes across species with the assumption tend to have orthologs in the same species and have correlated that interacting proteins would tend to coexist in genomes (10). -
Homology Modeling and Molecular Docking of Antagonists to Class B G
University of Vermont ScholarWorks @ UVM Graduate College Dissertations and Theses Dissertations and Theses 2016 Homology Modeling and Molecular Docking of Antagonists to Class B G-Protein Coupled Receptor Pituitary Adenylate Cyclase Type 1 (PAC1R) Suzanne Louise Stanton University of Vermont Follow this and additional works at: https://scholarworks.uvm.edu/graddis Part of the Chemistry Commons Recommended Citation Stanton, Suzanne Louise, "Homology Modeling and Molecular Docking of Antagonists to Class B G-Protein Coupled Receptor Pituitary Adenylate Cyclase Type 1 (PAC1R)" (2016). Graduate College Dissertations and Theses. 624. https://scholarworks.uvm.edu/graddis/624 This Thesis is brought to you for free and open access by the Dissertations and Theses at ScholarWorks @ UVM. It has been accepted for inclusion in Graduate College Dissertations and Theses by an authorized administrator of ScholarWorks @ UVM. For more information, please contact [email protected]. HOMOLOGY MODELING AND MOLECULAR DOCKING OF ANTAGONISTS TO CLASS B G-PROTEIN COUPLED RECEPTOR PITUITARY ADENYLATE CYLCASE TYPE 1 (PAC1R) A Thesis Presented by Suzanne Louise Stanton to The Faculty of the Graduate College of The University of Vermont In Partial Fulfillment of the Requirements for the Degree of Master of Science Specializing in Organic Chemistry/Chemistry October, 2016 Defense Date: May 9, 2016 Thesis Examination Committee: Matthias Brewer, Ph.D., Advisor Jose Madalengoitia, Ph.D. Victor May, Ph.D. Rory Waterman, Ph.D. Cynthia J. Forehand, PhD., Dean of the Graduate College ABSTRACT Recent studies have identified the Class B g-protein coupled receptor (GPCR) pituitary adenylate cyclase activating polypeptide type 1 (PAC1R) as a key component in physiological stress management. -
Transcriptomic Analysis by RNA Sequencing Characterises Malignant Progression of Canine Insulinoma from Normal Tissue to Metastatic Disease Y
www.nature.com/scientificreports OPEN Transcriptomic analysis by RNA sequencing characterises malignant progression of canine insulinoma from normal tissue to metastatic disease Y. Capodanno1,2*, F. O. Buishand 2,3, L. Y. Pang2, J. Kirpensteijn3,5, J. A. Mol3, R. Elders2,4 & D. J. Argyle2 Insulinomas (INS) are the most common human and canine functioning pancreatic neuroendocrine tumours. The long-term prognosis for malignant INS is poor, because micrometastases are frequently missed during surgery. As human and canine malignant INS share clinical and histopathological features, dogs have been proposed as models for INS research. Using RNA-sequencing, we conducted a pilot study to better understand the underlying molecular mechanisms of canine INS. Normal canine pancreas and lymph node control tissues were compared with primary INS and INS-metastatic lymph nodes, revealing more than 3,000 genes diferentially expressed in normal pancreas compared to primary INS. Only 164 genes were diferentially expressed between primary INS and INS-metastatic lymph nodes. Hierarchical clustering analysis demonstrated similar genetic profles in normal pancreas and early clinical stage primary INS, whereas late clinical stage primary INS resembled the genetic profle of INS-metastatic lymph nodes. These fndings suggest that markers of malignant behaviour could be identifed at the primary site of the disease. Finally, using the REACTOME pathways database, we revealed that an active collagen metabolism, extracellular matrix remodelling, beta- cell diferentiation and non-beta-cell trans-diferentiation might cause disease progression and hyperinsulinism in INS, identifying major pathways worthy of future research in this currently poorly controlled disease. Insulinomas (INS) are the most commonly diagnosed functioning pancreatic neuroendocrine tumours in humans and dogs1,2. -

Heparanase Overexpression Induces Glucagon Resistance and Protects
Page 1 of 85 Diabetes Heparanase overexpression induces glucagon resistance and protects animals from chemically-induced diabetes Dahai Zhang1, Fulong Wang1, Nathaniel Lal1, Amy Pei-Ling Chiu1, Andrea Wan1, Jocelyn Jia1, Denise Bierende1, Stephane Flibotte1, Sunita Sinha1, Ali Asadi2, Xiaoke Hu2, Farnaz Taghizadeh2, Thomas Pulinilkunnil3, Corey Nislow1, Israel Vlodavsky4, James D. Johnson2, Timothy J. Kieffer2, Bahira Hussein1 and Brian Rodrigues1 1Faculty of Pharmaceutical Sciences, UBC, 2405 Wesbrook Mall, Vancouver, BC, Canada V6T 1Z3; 2Department of Cellular & Physiological Sciences, Life Sciences Institute, UBC, 2350 Health Sciences Mall, Vancouver, BC, Canada V6T 1Z3; 3Department of Biochemistry and Molecular Biology, Faculty of Medicine, Dalhousie University, 100 Tucker Park Road, Saint John, NB, Canada E2L 4L5; 4Cancer and Vascular Biology Research Center, Rappaport Faculty of Medicine, Technion, Haifa, Israel 31096 Running Title: Heparanase overexpression and the pancreatic islet Corresponding author: Dr. Brian Rodrigues Faculty of Pharmaceutical Sciences University of British Columbia, 2405 Wesbrook Mall, Vancouver, B.C., Canada V6T 1Z3 TEL: (604) 822-4758; FAX: (604) 822-3035 E-mail: [email protected] Key Words: Heparanase, heparan sulfate proteoglycan, glucose homeostasis, glucagon resistance, pancreatic islet, STZ Word Count: 4761 Total Number of DiabetesFigures: Publish 6 Ahead of Print, published online October 7, 2016 Diabetes Page 2 of 85 Abstract Heparanase, a protein with enzymatic and non-enzymatic properties, contributes towards disease progression and prevention. In the current study, a fortuitous observation in transgenic mice globally overexpressing heparanase (hep-tg) was the discovery of improved glucose homeostasis. We examined the mechanisms that contribute towards this improved glucose metabolism. Heparanase overexpression was associated with enhanced GSIS and hyperglucagonemia, in addition to changes in islet composition and structure. -

Adenylyl Cyclase 2 Selectively Regulates IL-6 Expression in Human Bronchial Smooth Muscle Cells Amy Sue Bogard University of Tennessee Health Science Center
University of Tennessee Health Science Center UTHSC Digital Commons Theses and Dissertations (ETD) College of Graduate Health Sciences 12-2013 Adenylyl Cyclase 2 Selectively Regulates IL-6 Expression in Human Bronchial Smooth Muscle Cells Amy Sue Bogard University of Tennessee Health Science Center Follow this and additional works at: https://dc.uthsc.edu/dissertations Part of the Medical Cell Biology Commons, and the Medical Molecular Biology Commons Recommended Citation Bogard, Amy Sue , "Adenylyl Cyclase 2 Selectively Regulates IL-6 Expression in Human Bronchial Smooth Muscle Cells" (2013). Theses and Dissertations (ETD). Paper 330. http://dx.doi.org/10.21007/etd.cghs.2013.0029. This Dissertation is brought to you for free and open access by the College of Graduate Health Sciences at UTHSC Digital Commons. It has been accepted for inclusion in Theses and Dissertations (ETD) by an authorized administrator of UTHSC Digital Commons. For more information, please contact [email protected]. Adenylyl Cyclase 2 Selectively Regulates IL-6 Expression in Human Bronchial Smooth Muscle Cells Document Type Dissertation Degree Name Doctor of Philosophy (PhD) Program Biomedical Sciences Track Molecular Therapeutics and Cell Signaling Research Advisor Rennolds Ostrom, Ph.D. Committee Elizabeth Fitzpatrick, Ph.D. Edwards Park, Ph.D. Steven Tavalin, Ph.D. Christopher Waters, Ph.D. DOI 10.21007/etd.cghs.2013.0029 Comments Six month embargo expired June 2014 This dissertation is available at UTHSC Digital Commons: https://dc.uthsc.edu/dissertations/330 Adenylyl Cyclase 2 Selectively Regulates IL-6 Expression in Human Bronchial Smooth Muscle Cells A Dissertation Presented for The Graduate Studies Council The University of Tennessee Health Science Center In Partial Fulfillment Of the Requirements for the Degree Doctor of Philosophy From The University of Tennessee By Amy Sue Bogard December 2013 Copyright © 2013 by Amy Sue Bogard. -

Capturing Peptide–GPCR Interactions and Their Dynamics
molecules Review Capturing Peptide–GPCR Interactions and Their Dynamics Anette Kaiser * and Irene Coin Faculty of Life Sciences, Institute of Biochemistry, Leipzig University, Brüderstr. 34, D-04103 Leipzig, Germany; [email protected] * Correspondence: [email protected] Academic Editor: Paolo Ruzza Received: 31 August 2020; Accepted: 9 October 2020; Published: 15 October 2020 Abstract: Many biological functions of peptides are mediated through G protein-coupled receptors (GPCRs). Upon ligand binding, GPCRs undergo conformational changes that facilitate the binding and activation of multiple effectors. GPCRs regulate nearly all physiological processes and are a favorite pharmacological target. In particular, drugs are sought after that elicit the recruitment of selected effectors only (biased ligands). Understanding how ligands bind to GPCRs and which conformational changes they induce is a fundamental step toward the development of more efficient and specific drugs. Moreover, it is emerging that the dynamic of the ligand–receptor interaction contributes to the specificity of both ligand recognition and effector recruitment, an aspect that is missing in structural snapshots from crystallography. We describe here biochemical and biophysical techniques to address ligand–receptor interactions in their structural and dynamic aspects, which include mutagenesis, crosslinking, spectroscopic techniques, and mass-spectrometry profiling. With a main focus on peptide receptors, we present methods to unveil the ligand–receptor contact interface and methods that address conformational changes both in the ligand and the GPCR. The presented studies highlight a wide structural heterogeneity among peptide receptors, reveal distinct structural changes occurring during ligand binding and a surprisingly high dynamics of the ligand–GPCR complexes. Keywords: GPCR activation; peptide–GPCR interactions; structural dynamics of GPCRs; peptide ligands; crosslinking; NMR; EPR 1. -
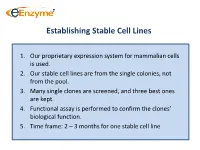
Establishing Stable Cell Lines
Establishing Stable Cell Lines 1. Our proprietary expression system for mammalian cells is used. 2. Our stable cell lines are from the single colonies, not from the pool. 3. Many single clones are screened, and three best ones are kept. 4. Functional assay is performed to confirm the clones’ biological function. 5. Time frame: 2 – 3 months for one stable cell line List of In-Stock ACTOne GPCR Stable Clones Transduced Gi-coupled receptors (22) Transduced Gs coupled receptors (34) Cannabinoid receptor 1 (CB1) Vasoactive Intestinal Peptide Receptor 2 (VIPR2) Dopamine Receptor 2 (DRD2) Melanocortin 4 Receptor (MC4R) Melanocortin 5 Receptor (MC5R) Somatostatin Receptor 5 (SSTR5) Parathyroid Hormone Receptor 1 (PTHR1) Adenosine A1 Receptor (ADORA1) Glucagon Receptor (GCGR) Chemokine (C-C motif) receptor 5 (CCR5) Dopamine Receptor 1 (DRD1) Melanin-concentrating Hormone Receptor 1 (MCHR1) Prostaglandin E Receptor 4 (EP4) Vasoactive Intestinal Peptide Receptor 1 (VIPR1) Cannabinoid receptor 2 (CB2) Gastric Inhibitor Peptide Receptor (GIPR) Glutamate receptor, metabotropic 8 (GRM8) Dopamine Receptor 5 (DRD5) Opioid receptor, kappa 1 (OPRK1) Parathyroid Hormone Receptor 2 (PTHR2) Adenosine A3 receptor (ADORA3) 5-hydroxytryptamine (serotonin) receptor 6 (HTR4) Corticotropin Releasing Hormone Receptor 2 (CRHR2) Glutamate receptor, metabotropic 8 (GRM8) Adenylate Cyclase Activating Polypeptide 1 Receptor type I (ADCYAP1R1) Neuropeptide Y Receptor Y1 (NPY1R) Secretin Receptor (SCTR) Neuropeptide Y Receptor Y2 (NPY2R) Follicle -

Characterization of Glucagon-Like Peptide-1 Receptor-Binding Determinants
321 Characterization of glucagon-like peptide-1 receptor-binding determinants Q Xiao, W Jeng and M B Wheeler Departments of Medicine and Physiology, University of Toronto, Toronto, Ontario, Canada M5S 1A8 (Requests for offprints should be addressed toMBWheeler, Department of Physiology, University of Toronto, 1 Kings College Circle, Toronto, Ontario, Canada M5S 1A8; Email: [email protected]) ABSTRACT Glucagon-like peptide 1 (GLP-1) is a potent supported by studies using chimeric glucose- insulinotropic hormone currently under study as a dependent insulinotropic polypeptide (GIP)/GLP-1 therapeutic agent for type 2 diabetes. Since an receptors. GIP(1–151)/GLP-1R, but not GIP(1– understanding of the molecular mechanisms leading 222)/GLP-1R, exhibited specific GLP-1 binding to high-affinity receptor (R) binding and activation and GLP-1-induced cAMP production, suggesting may facilitate the development of more potent that the region encompassing transmembrane (TM) GLP-1R agonists, we have localized specific regions domain 1 through to TM3 was required for of GLP-1R required for binding. The purified binding. Since it was hypothesized that certain N-terminal fragment (hereafter referred to as NT) charged or polar amino acids in this region might be of the GLP-1R produced in either insect (Sf9) or involved in binding, these residues (TM2–TM3) mammalian (COS-7) cells was shown to bind were analyzed by substitution mutagenesis. Five GLP-1. The physical interaction of NT with mutants (K197A, D198A, K202A, D215A, R227A) GLP-1 was first demonstrated by cross-linking displayed remarkably reduced binding affinity. (125I-GLP-1/NT complex band at 28 kDa) and These studies indicate that the NT domain of the secondly by attachment to Ni2+-NTA beads.