Consultation Report
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Part of a Former Cattle Ranching Area, Land There Was Gazetted by the Ugandan Government for Use by Refugees in 1990
NEW ISSUES IN REFUGEE RESEARCH Working Paper No. 32 UNHCR’s withdrawal from Kiryandongo: anatomy of a handover Tania Kaiser Consultant UNHCR CP 2500 CH-1211 Geneva 2 Switzerland e-mail: [email protected] October 2000 These working papers provide a means for UNHCR staff, consultants, interns and associates to publish the preliminary results of their research on refugee-related issues. The papers do not represent the official views of UNHCR. They are also available online at <http://www.unhcr.org/epau>. ISSN 1020-7473 Introduction The Kiryandongo settlement for Sudanese refugees is located in the north-eastern corner of Uganda’s Masindi district. Part of a former cattle ranching area, land there was gazetted by the Ugandan government for use by refugees in 1990. The first transfers of refugees took place shortly afterwards, and the settlement is now well established, with land divided into plots on which people have built houses and have cultivated crops on a small scale. Anthropological field research (towards a D.Phil. in anthropology, Oxford University) was conducted in the settlement from October 1996 to March 1997 and between June and November 1997. During the course of the fieldwork UNHCR was involved in a definitive process whereby it sought to “hand over” responsibility for the settlement at Kiryandongo to the Ugandan government, arguing that the refugees were approaching self-sufficiency and that it was time for them to be absorbed completely into local government structures. The Ugandan government was reluctant to accept this new role, and the refugees expressed their disbelief and feelings of betrayal at the move. -

And Bulima – Kabwoya Roads (66 Km) from Gravel to Bitumen Standard
UGANDA ROAD SECTOR SUPPORT PROJECT 4 (RSSP 4) UPGRADING OF KIGUMBA – MASINDI - HOIMA – KABWOYA ROAD (135 Km) FROM GRAVEL TO CLASS II BITUMEN STANDARD SPECIFIC PROCUREMENT NOTICE Invitation for Prequalification The Government of Uganda has applied for a loan from the African Development Fund (ADF) toward the cost of the Road Sector Support Project 4 (RSSP4) and it intends to apply part of the proceeds of this loan to payments under the contracts for the Upgrading of Kigumba – Bulima road (69 Km) and Bulima – Kabwoya roads (66 Km) from gravel to bitumen standard. Disbursement in respect of any contracts signed, will be subject to approval of the loan by the Bank. The Uganda National Roads Authority now intends to prequalify contractors and/or firms for: a) Lot 1: Upgrading of Kigumba – Bulima road (69Km) – Procurement No: No:UNRA/WORKS/2012-2013/00001/05/01 from gravel to class II bitumen standard. The Kigumba – Bulima road is located in the western part of Uganda and traverses the districts of Kiryandongo and Masindi. The project road starts from Kigumba which is located approximately 210 Km from Kampala along the Kampala – Gulu highway and follows a south-westerly direction via Masindi up to Bulima trading centre, located 36 Km on the Masindi – Hoima highway. The road works shall comprise upgrading the existing Class B gravel road to Class II bitumen standard 7.0m wide carriageway and 1.5 to 2.0m wide shoulders on either side, with a gravel sub-base, graded crushed stone base and double bituminous surface treatment. Also to be included are the associated drainage and ancillary works as well as implementation of environment and social mitigation measures. -

Speech to Parliament by H.E. Yoweri Kaguta Museveni President of The
Speech to Parliament By H.E. Yoweri Kaguta Museveni President of the Republic of Uganda Parliamentary Buildings - 13th December, 2012 1 Rt. Hon. Speaker, I have decided to use the rights of the President, under Article 101 (2) of the 1995 Constitution of the Republic of Uganda, to address Parliament. I am exercising this right in order to counter the nefarious and mendacious campaign of the foreign interests, using NGOs and some Members of Parliament, to try and cripple or disorient the development of the Oil sector. If the Ugandans may remember, this is not the first time these interests try to distort the development of our history. When we were fighting the Sudanese-sponsored terrorism of Kony or when we were fighting the armed cattle- rustlers in Karamoja, you remember, there were groups, including some religious leaders, Opposition Members of Parliament as well as NGOs, which would spend all the 2 time denouncing us, the Freedom Fighters. They were denouncing those who were fighting to defend the lives and properties of the people, rather than denouncing the terrorists, the cattle-rustlers and their external-backers (in the case of Kony) as well as their internal collaborators. It would appear as if the wrong-doer was the Government, the NRM, rather than the criminals. We, patiently, put up with that malignment at the same time as we fought, got injured or killed, against the enemy until we achieved victory. Eventually, we won, supported by the ordinary people and the different people’s militias. There is total peace in the whole country and yet the misleaders of those years have not apologized to the Ugandans for their mendacity. -

Uganda National Roads Authority
THE REPUBLIC OF UGANDA UGANDA NATIONAL ROADS AUTHORITY REPORT OF THE AUDITOR GENERAL ON THE FINANCIAL STATEMENTS OF THE ROAD SECTOR SUPPORT PROJECT 4 (RSSP– 4) KIGUMBA – MASINDI – HOIMA – KABWOYA ROAD PROJECT ADF LOAN – PROJECT ID NO P-UG-DB0-021 FOR THE YEAR ENDED 3OTH JUNE 2016 OFFICE OF THE AUDITOR GENERAL UGANDA TABLE OF CONTENTS REPORT OF THE AUDITOR GENERAL ON THE FINANCIAL STATEMENTS OF THE ROAD SECTOR SUPPORT PROJECT (RSSP 4) ADF LOAN-PROJECT ID NO P-UG-DB0-021 FOR THE YEAR ENDED 30TH JUNE 2016 .......................................................................... iii 1.0 INTRODUCTION .................................................................................................. 1 2.0 PROJECT BACKGROUND ...................................................................................... 1 3.0 PROJECT OBJECTIVES AND COMPONENTS ............................................................ 2 4.0 AUDIT OBJECTIVES ............................................................................................. 2 5.0 AUDIT PROCEDURES PERFORMED ....................................................................... 3 6.0 CATEGORIZATION AND SUMMARY OF FINDINGS .................................................. 4 6.1 Categorization of Findings .................................................................................... 4 6.2 Summary of Findings ........................................................................................... 5 7.0 DETAILED FINDINGS .......................................................................................... -

Kiryandongo Ple Results 2017
THE REPUBLIC OF UGANDA OFFICE OF THE DISTRICT INSPECTOR OF SCHOOLS KIRYANDONGO DISTRICT P.O. BOX 137, KIGUMBA UGANDA DISTRICT PERFORMANCE 2017 DIVISION MALE FEMALES TOTAL % ONE 192 82 274 5.8 TWO 1480 1046 2526 53.8 THREE 478 552 1030 21.9 Ref COU 01 FOUR 310 314 624 13.3 UNGRADED(U) 100 141 241 5.1 ABSENT(X) 36 38 74 1.6 TOTAL 2596 2173 4769 100 BEST TEN (10) GOVERNMENT AIDED SCHOOLS. S/N SCHOOL DIV1 TOTAL NO GRADE POINTS 1 KIRYANDONGO C.O.U 13 63 3.17 2 CANROM 27 158 3.16 3 ARNOLD MEMORIAL 19 128 3.09 4 KIGUMBA C.O.U 09 83 3.0 5 KIRYANDONGO BCS 01 63 2.94 6 KIHURA 01 65 2.93 7 JEEJA 01 33 2.81 8 BWEYALE COU 03 67 2.80 9 KIGUMBA MOSLEM 00 40 2.77 10 BWEYALE PUBLIC 05 75 2.76 BEST TEN (10) PRIVATE SCHOOLS S/N SCHOOL DIV1 TOTAL NO GRADE POINTS 1 KIRYANDONGO 27 36 3.75 INTENSIVE 2 KIGUMBA INTENSIVE 33 50 3.66 3 NEW BWEYALE PARENTS 26 40 3.65 4 KIGUMBA CENTER 31 49 3.63 5 MONTESSORI 04 15 3.26 6 KIGUMBA WESTIN 04 16 3.26 7 MASINDI PORT 02 35 3.05 PARENTS 8 STAR EDUCATION 22 156 3.01 CENTRE 9 BWEYALE PRIVATE 05 41 3.0 10 BWEYALE MODERN 04 42 2.95 BEST TEN (10) CANDIDATES PER CATEGORY S/N NAME SCHOOL AGGREGATES 1 ANNAH YAR ARNOLD MEMORIAL 7 2 ANGETH MAGOT CHOL KIRYANDONGO C.O.U 8 3 MONDAY FRANCIS YELEKENI 9 4 BIJANY LIEP ARNOLD 9 5 EDEMA JOEL ARNOLD 9 6 OCAYA JOHN OLWENY SIRIBA 9 7 MOHAMMAD SALEH ARNOLD 9 8 OMARA MARK KIRYANDONGO C.O.U 9 9 ACEIHICK BUL RAPHEAL CANROM 9 10 KATUSIIME BRENDA CANROM 9 GOVERNMENT AIDED SCHOOLS PRIVATE SCHOOLS S/N NAME SCHOOL AGGREGATES 1 OJWIGA BRIAN KIRYANDONGO INTENSIVE 6 2 MAMUKE MATHA KIGUMBA CENTRE 7 3 OJOK -
Assessment of the Capacity of Ugandan Health Facilities, Personnel, and Resources to Prevent and Control Noncommunicable Diseases
Yale University EliScholar – A Digital Platform for Scholarly Publishing at Yale Public Health Theses School of Public Health January 2014 Assessment Of The aC pacity Of Ugandan Health Facilities, Personnel, And Resources To Prevent And Control Noncommunicable Diseases Hilary Eileen Rogers Yale University, [email protected] Follow this and additional works at: http://elischolar.library.yale.edu/ysphtdl Recommended Citation Rogers, Hilary Eileen, "Assessment Of The aC pacity Of Ugandan Health Facilities, Personnel, And Resources To Prevent And Control Noncommunicable Diseases" (2014). Public Health Theses. 1246. http://elischolar.library.yale.edu/ysphtdl/1246 This Open Access Thesis is brought to you for free and open access by the School of Public Health at EliScholar – A Digital Platform for Scholarly Publishing at Yale. It has been accepted for inclusion in Public Health Theses by an authorized administrator of EliScholar – A Digital Platform for Scholarly Publishing at Yale. For more information, please contact [email protected]. ASSESSMENT OF THE CAPACITY OF UGANDAN HEALTH FACILITIES, PERSONNEL, AND RESOURCES TO PREVENT AND CONTROL NONCOMMUNICABLE DISEASES By Hilary Rogers A Thesis Presented to the Faculty of the Yale School of Public Health in Partial Fulfillment of the Requirements for the Degree of Masters of Public Health in the Department of Chronic Disease Epidemiology New Haven, Connecticut April 2014 Readers: Dr. Adrienne Ettinger, Yale School of Public Health Dr. Jeremy Schwartz, Yale School of Medicine ABSTRACT Due to the rapid rise of noncommunicable diseases (NCDs), the Uganda Ministry of Health (MoH) has prioritized NCD prevention, early diagnosis, and management. In partnership with the World Diabetic Foundation, MoH has embarked on a countrywide program to build capacity of the health facilities to address NCDs. -
Albertine Region Sustainable Development Project (Arsdp)
Republic of Uganda ALBERTINE REGION SUSTAINABLE DEVELOPMENT PROJECT (ARSDP) RESETTLEMENT POLICY FRAMEWORK (RPF) VOLUME 1 FINAL DRAFT REPORT NOVEMBER 2013 EXECUTIVE SUMMARY Background The Government of Uganda (GoU) with support of the World Bank (IDA) is preparing the Albertine Region Sustainable Development Project. The Albertine Rift Valley is a center for rapid growth which is likely to accelerate with the oil development underway in the region. To ensure that the benefits of the oil development reach the residents of the area, GoU is keen to improve connectivity to and within the region and local economic infrastructure. The two Districts of Buliisa and Hoima are the focus of the project as well as the Town Council of Buliisa. Hoima Municipality is already included in the USMID project, which is shortly to commence, and is thus not included in the ARSDP. Project Components The Project has three components which are outlined below. Component 1. upgrading of 238km of Kyenjojo-Kabwoya-Hoima-Masindi-Kigumba is to be funded by both the AfDB (138km) and The World Bank (IDA) (100km). The RAP for this component has already been prepared, comments reviewed by the Bank and an update of PAPs and property is on going therefore this RPF does not cover component 1. The project coverage for component 2 and 3 will be as described below but in the event that additional districts are added under component 2 and any additioanl technical colleges are added under component 3 this RPF will apply. Component 1: Regional Connectivity: Improvement of the Kyenjojo-Kabwoya-Hoima- Kigumba National Road. -

Uganda National Roads Authority
THE REPUBLIC OF UGANDA UGANDA NATIONAL ROADS AUTHORITY REPORT OF THE AUDITOR GENERAL ON THE FINANCIAL STATEMENTS OF THE ROAD SECTOR SUPPORT PROJECT 4 (RSSP– 4) KIGUMBA – MASINDI – HOIMA – KABWOYA ROAD PROJECT ADF LOAN – PROJECT ID NO P-UG-DB0-021 FOR THE YEAR ENDED 3OTH JUNE 2017 OFFICE OF THE AUDITOR GENERAL UGANDA TABLE OF CONTENTS Opinion ............................................................................................................... 2 Basis for Opinion .................................................................................................. 2 Key Audit Matters ................................................................................................ 3 Other Matter ........................................................................................................ 6 Management’s Responsibility for the financial Statements ..................................... 10 Auditor’s Responsibilities for the Audit of the Financial Statements ........................ 10 Other Reporting Requirements ............................................................................ 12 1 REPORT OF THE AUDITOR GENERAL ON THE FINANCIAL STATEMENTS OF THE ROAD SECTOR SUPPORT PROJECT (RSSP 4) ADF LOAN-PROJECT ID NO P-UG-DB0-021 FOR THE YEAR ENDED 30TH JUNE 2017 THE RT. HON. SPEAKER OF PARLIAMENT REPORT ON THE FINANCIAL STATEMENTS Opinion I have audited the accompanying financial statements of the Road Sector Support Project 4 (upgrading of the Kigumba – Masindi – Hoima – Kabwoya Road Project) for the year ended 30th June 2017. -
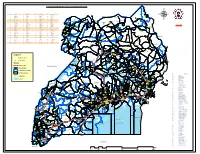
Legend " Wanseko " 159 !
CONSTITUENT MAP FOR UGANDA_ELECTORAL AREAS 2016 CONSTITUENT MAP FOR UGANDA GAZETTED ELECTORAL AREAS FOR 2016 GENERAL ELECTIONS CODE CONSTITUENCY CODE CONSTITUENCY CODE CONSTITUENCY CODE CONSTITUENCY 266 LAMWO CTY 51 TOROMA CTY 101 BULAMOGI CTY 154 ERUTR CTY NORTH 165 KOBOKO MC 52 KABERAMAIDO CTY 102 KIGULU CTY SOUTH 155 DOKOLO SOUTH CTY Pirre 1 BUSIRO CTY EST 53 SERERE CTY 103 KIGULU CTY NORTH 156 DOKOLO NORTH CTY !. Agoro 2 BUSIRO CTY NORTH 54 KASILO CTY 104 IGANGA MC 157 MOROTO CTY !. 58 3 BUSIRO CTY SOUTH 55 KACHUMBALU CTY 105 BUGWERI CTY 158 AJURI CTY SOUTH SUDAN Morungole 4 KYADDONDO CTY EST 56 BUKEDEA CTY 106 BUNYA CTY EST 159 KOLE SOUTH CTY Metuli Lotuturu !. !. Kimion 5 KYADDONDO CTY NORTH 57 DODOTH WEST CTY 107 BUNYA CTY SOUTH 160 KOLE NORTH CTY !. "57 !. 6 KIIRA MC 58 DODOTH EST CTY 108 BUNYA CTY WEST 161 OYAM CTY SOUTH Apok !. 7 EBB MC 59 TEPETH CTY 109 BUNGOKHO CTY SOUTH 162 OYAM CTY NORTH 8 MUKONO CTY SOUTH 60 MOROTO MC 110 BUNGOKHO CTY NORTH 163 KOBOKO MC 173 " 9 MUKONO CTY NORTH 61 MATHENUKO CTY 111 MBALE MC 164 VURA CTY 180 Madi Opei Loitanit Midigo Kaabong 10 NAKIFUMA CTY 62 PIAN CTY 112 KABALE MC 165 UPPER MADI CTY NIMULE Lokung Paloga !. !. µ !. "!. 11 BUIKWE CTY WEST 63 CHEKWIL CTY 113 MITYANA CTY SOUTH 166 TEREGO EST CTY Dufile "!. !. LAMWO !. KAABONG 177 YUMBE Nimule " Akilok 12 BUIKWE CTY SOUTH 64 BAMBA CTY 114 MITYANA CTY NORTH 168 ARUA MC Rumogi MOYO !. !. Oraba Ludara !. " Karenga 13 BUIKWE CTY NORTH 65 BUGHENDERA CTY 115 BUSUJJU 169 LOWER MADI CTY !. -

Uganda National Roads Network
UGANDA NATIONAL ROADS NETWORK REPUBLIC OF SOUTH SUDAN Musingo #" !P Kidepo a w K ± r i P !P e t Apoka gu a K m #" lo - g - L a o u k - #" g u P i #" n d Moyo!P g o i #"#" - t #"#" N i k #" KOBOKO M e g a #" #" #" l Nimule o #"!P a YUMBE #" u!P m ng m o #" e #" Laropi i #" ro ar KAABONG #" !P N m K #" (! - o - te o e om Kaabong#"!P g MOYO T c n o #" o #" L be Padibe !P - b K m !P LAMWO #" a oboko - Yu Yumbe #" om r K #" #" #" O #" Koboko #" #" - !P !P o Naam REGIONS AND STATIONS Moy n #" Lodonga Adjumani#" Atiak - #" Okora a #" Obongi #" !P #" #" a Loyoro #" p #" Ob #" KITGUM !P !P #" #" ong !P #" #" m A i o #" - #" - K #" Or u - o lik #" m L Omugo ul #" !P u d #" in itg o i g Kitgum t Maracha !P !P#" a K k #" !P #" #"#" a o !P p #" #" #" Atiak K #" e #" (!(! #" Kitgum Matidi l MARACHA P e - a #" A #"#" e #" #" ke d #" le G d #" #" i A l u a - Kitgum - P l n #" #" !P u ADJUMANI #" g n a Moyo e !P ei Terego b - r #" ot Kotido vu #" b A e Acholibur - K o Arua e g tr t u #" i r W #" o - O a a #" o n L m fe di - k Atanga KOTIDO eli #" ilia #" Rh #" l p N o r t h #"#" B ino Rhino !P o Ka Gulu !P ca #" #"#" aim ARUA mp - P #" #" !P Kotido Arua #" Camp Pajule go #" !P GULU on #" !P al im #" !PNariwo #" u #" - K b A ul r A r G de - i Lira a - Pa o a Bondo #" Amuru Jun w id m Moroto Aru #" ctio AMURU s ot !P #" n - A o #" !P A K i !P #" #" PADER N o r t h E a s t #" Inde w Kilak #" - #" e #" e AGAGO K #"#" !P a #" #" #" y #" a N o #" #" !P #" l w a Soroti e #"#" N Abim b - Gulu #" - K d ilak o b u !P #" Masindi !P i um !P Adilang n - n a O e #" -

Kiryandongo District HRV Profile.Pdf
Kiryandongo District Hazard, Risk and Vulnerability Profi le 2016 Acknowledgement On behalf of Office of the Prime Minister, I wish to express my sincere appreciation to all of the key stakeholders who provided their valuable inputs and support to this Multi-Hazard, Risk and Vulnerability mapping exercise that led to the production of comprehensive district Hazard, Risk and Vulnerability (HRV) profiles. I extend my sincere thanks to the Department of Relief, Disaster Preparedness and Management, under the leadership of the Commissioner, Mr. Martin Owor, for the oversight and management of the entire exercise. The HRV assessment team was led by Ms. Ahimbisibwe Catherine, Senior Disaster Preparedness Officer supported by Ogwang Jimmy, Disaster Preparedness Officer and the team of consultants (GIS/DRR specialists); Dr. Bernard Barasa, and Mr. Nsiimire Peter, who provided technical support. Our gratitude goes to UNDP for providing funds to support the Hazard, Risk and Vulnerability Mapping. The team comprised of Mr. Steven Goldfinch – Disaster Risk Management Advisor, Mr. Gilbert Anguyo - Disaster Risk Reduction Analyst, and Mr. Ongom Alfred- Early Warning system Database programmer. My appreciation also goes to Kiryandongo District Team. The entire body of stakeholders who in one way or another yielded valuable ideas and time to support the completion of this exercise. Hon. Hilary O. Onek Minister for Relief, Disaster Preparedness and Refugees KIRYANDONGO DISTRICT HAZARD, RISK AND VULNERABILITY PROFILE i TABLE OF CONTENTS ACKNOWLEDGEMENT .................................................................................................................i -

Uganda Hospital and Health Centre IV Census Survey 2014
THE REPUBLIC OF UGANDA MINISTRY OF HEALTH Uganda Hospital and Health Centre IV Census Survey 2014 THE REPUBLIC OF UGANDA MINISTRY OF HEALTH Uganda Hospital and Health Centre IV Census Survey 2014 2 4 6 Table of Contents FOREWORD MINISTER ............................................................................................................................ 3 ACKNOWLEDGEMENT ............................................................................................................................. 5 Table of Contents .................................................................................................................................... 7 List of tables ............................................................................................................................................ 9 List of figures ......................................................................................................................................... 11 List of Acronyms .................................................................................................................................... 17 EXECUTIVE SUMMARY .......................................................................................................................... 18 INTRODUCTION ..................................................................................................................................... 32 1.1. Background ............................................................................................................................