Pdf 123 PMID: 24620729 [Cited 2016 Nov 11]
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Land Commission Consultations
Republic of Liberia REPORT 2010 Land Commission Consultations Land Commission Consultations 2010 ACKNOWLEDGMENTS This report was compiled and written by the Program Staff of the Technical Secretariat of the Land Commission (LC) under the guidance and supervision of Mr. Stanley N. Toe, Land Policy and Program Development Officer. The Technical Secretariat extends its profound appreciation and gratitude to Chairman Brandy and other Commissioners of the LC for their unflinching support to this undertaking from the inception stage to the conclusion. We also acknowledge with thanks, the vital role played by Mrs. Guglielma da Passano, UN-Habitat Technical Advisor to the Land Commission in providing editorial guidance and useful feed- back during the entire exercise. An array of individuals and institutions also contributed immensely to the successful conduct of the county meetings. We hereby mention some of their names in recognition of their contributions in the form of financial and logistical support: the Minister and staff of the Ministry of Internal Affairs (MIA), superintendents and local officials of the counties, our international partners in particular, the UN-Habitat for providing the funding and logistical support for these consultative meetings. Also, the Norwegian Refugee Council (NRC) for logistical and related support during the consultative meetings in Nimba, Bong and Lofa Counties respectively and the United Nations Mission in Liberia (UNMIL). Finally, to the participants from the various counties, normally unheralded and acknowledged in matters such as this, we say in the proverbial Liberian jargon ‘thank you yah’ for taking time off your engaging schedules to honor our invitation to participate in these meetings. -

Grand Gedeh County Development Agenda
Grand Gedeh County Development Agenda Republic of Liberia 2008 – 2012 Grand Gedeh County Development Agenda County Vision Statement Grand Gedeh: an icon of unity, peace, good governance and quality social, economic and infrastructure development for all. Core Values Equal access to opportunities for all Grand Gedeh Citizens; Assurance of peace, security and the rule of law; Transparent and effective governance; Sustainable economic growth; and Preservation of natural resources and environment. Republic of Liberia Prepared by the County Development Committee, in collaboration with the Ministries of Planning and Economic Affairs and Internal Affairs. Supported by the UN County Support Team project, funded by the Swedish Government and UNDP. Table of Contents A MESSAGE FROM THE MINISTER OF INTERNAL AFFAIRS........! iii FOREWORD..........................................................................! iv PREFACE!!............................................................................. vi GRAND GEDEH COUNTY OFFICIALS......................................! vii EXECUTIVE SUMMARY..........................................................! xi PART 1 - INTRODUCTION AND BACKGROUND 1.1.!Introduction................................................................................................! 1 1.2 History........................................................................................................! 2 1.3 Geography..................................................................................................! 2 1.4 Demography -
GEOLEV2 Label Updated October 2020
Updated October 2020 GEOLEV2 Label 32002001 City of Buenos Aires [Department: Argentina] 32006001 La Plata [Department: Argentina] 32006002 General Pueyrredón [Department: Argentina] 32006003 Pilar [Department: Argentina] 32006004 Bahía Blanca [Department: Argentina] 32006005 Escobar [Department: Argentina] 32006006 San Nicolás [Department: Argentina] 32006007 Tandil [Department: Argentina] 32006008 Zárate [Department: Argentina] 32006009 Olavarría [Department: Argentina] 32006010 Pergamino [Department: Argentina] 32006011 Luján [Department: Argentina] 32006012 Campana [Department: Argentina] 32006013 Necochea [Department: Argentina] 32006014 Junín [Department: Argentina] 32006015 Berisso [Department: Argentina] 32006016 General Rodríguez [Department: Argentina] 32006017 Presidente Perón, San Vicente [Department: Argentina] 32006018 General Lavalle, La Costa [Department: Argentina] 32006019 Azul [Department: Argentina] 32006020 Chivilcoy [Department: Argentina] 32006021 Mercedes [Department: Argentina] 32006022 Balcarce, Lobería [Department: Argentina] 32006023 Coronel de Marine L. Rosales [Department: Argentina] 32006024 General Viamonte, Lincoln [Department: Argentina] 32006025 Chascomus, Magdalena, Punta Indio [Department: Argentina] 32006026 Alberti, Roque Pérez, 25 de Mayo [Department: Argentina] 32006027 San Pedro [Department: Argentina] 32006028 Tres Arroyos [Department: Argentina] 32006029 Ensenada [Department: Argentina] 32006030 Bolívar, General Alvear, Tapalqué [Department: Argentina] 32006031 Cañuelas [Department: Argentina] -

A National Biodiversity Offset Scheme: a Road Map for Liberia S
Public Disclosure Authorized A National Biodiversity Offset Scheme: A Road Map for Liberias Mining Sector Public Disclosure Authorized Public Disclosure Authorized Public Disclosure Authorized Joseph Onoja Joseph March 2015 9200_Liberia_FM.indd 1 3/23/15 12:33 PM 9200_Liberia_FM.indd 2 3/23/15 12:33 PM Contents Acknowledgments vii Executive Summary: A Road Map for Liberia ix Introduction ix The Conservation Imperative for Liberia: Remarkable Biodiversity at Risk x The Challenge of Securing Lasting Conservation Outcomes in Liberia xiii A Role for Biodiversity Offsets in Securing Conservation Outcomes xiv Legal, Policy, and Institutional Framework in Support of a National Biodiversity Offset Scheme xviii Methodological Challenges and Approach to Implementing a National Offset Scheme xxi Conclusion and Summary Road Map xxiv Notes xxvi References xxvi 1 Introduction 1 Project Background 1 Scope of the Report 2 Report Structure 3 Notes 3 References 3 2 The Conservation Imperative for Liberia: Remarkable Biodiversity at Risk 4 Introduction 4 Overview of International Designations within Liberia 4 Protected Areas and Proposed Protected Areas 7 Summary of Findings and Way Forward 18 Notes 19 References 19 3 The Challenge of Securing Lasting Conservation Outcomes in Liberia 22 Introduction 22 Key Threats to Biodiversity in Liberia 23 The Implications of Land Tenure for Establishing Protected Areas 24 Competition for Land and Overlapping Concessions 27 Summary of Findings and Way Forward 31 Notes 32 References 33 4 A Role for Offsets in Securing -
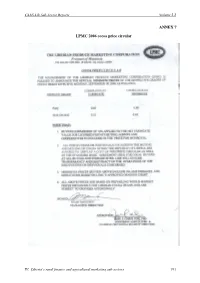
ANNEX 7 LPMC 2006 Cocoa Price Circular
CAAS-Lib Sub-Sector Reports Volume 2.2 ANNEX 7 LPMC 2006 cocoa price circular IV. Liberia’s rural finance and agricultural marketing sub-sectors 191 V. INSTITUTIONAL CAPACITIES AND RENEWAL STRATEGIES FOR RURAL DEVELOPMENT IN LIBERIA By Consultants, FAO: Dr Michael Connolly Dr Peter Smith Dr Othello Brandy and Dr Ponniah Anandajayasekeram, Consultant, IFPRI Liberia 2007 CAAS-Lib Sub-Sector Reports Volume 2.2 ACRONYMS ACDB Agricultural Cooperative Development Bank AIDS Acquired immune deficiency syndrome BCADP Bong County Agricultural Development Project BOB Bureau of the Budget BWI Booker Washington Institute CAC County Agricultural Coordinator CARI Central Agricultural Research Institute CBO Community-based Organization CDA Cooperative Development Authority CDT County Development Team CGIAR Consultative Group on International Agricultural Research CIPs County information packs CST County Support Team CD Capacity development CFA Core functional analysis CMP Change management programme DDC District Development Committee DEC Decadal computions of crop water requirements, irrigation water requirements, rainfall, and effective rainfall. DRDE Department of Regional Development and Extension (in MOA) FAO Food and Agriculture Organization of the UN FARA Forum for Agricultural Research in Africa FDA Forestry Development Authority FFS Farmer field schools FOD Farmer organization development FY Financial year GDP Gross domestic product GOL Government of Liberia GRC Governance Reform Commission GTZ German Technical Cooperation HIV Human immunodeficiency -

Peace in Liberia Challenges to Consolidation of Peace
JOINT PROGRAMME UNIT FOR UN/INTERPEACE INITIATIVES JPU Peace in Liberia Challenges to Consolidation of Peace in the eyes of the communities A Report by the Platform for Dialogue and Peace in Liberia Made possible with the support of the UN Peacebuilding Fund Foreword Interpeace and all of its collaborating partners are immensely pleased to release this report that highlights local communities’ views of conflict as they feel its pinch in their respective communities. We release it with the fond hope that the government and people of Liberia, the United Nations Mission in Liberia (UNMIL) and all stakeholders -those like us, with the avowed and common pursuit of consolidating peace and stability in Liberia- will pay keen heed to its prescriptions. The report covers diverse issues of conflict generated after nearly one year of intense field work, copious record keeping, and audio-visual tracking of the field processes. Research teams from our local partners applied lessons from participatory methodologies developed by Interpeace, along with their own knowledge of the socio-economic, political and cultural context of three regions, in a nationwide research consultation. They reached remote villages and towns in northwestern, central and southeastern Liberia using introductory letters from the Ministry of Internal Affairs and obtained essential briefings by UNMIL regional military commanders and civil authorities in designing strategies for sampling key communities for consultation in the fifteen counties. Those consulted included local authorities, traditional leaders, youth, women, elders, religious and other citizens and residents, ensuring the participation of marginalized and disabled persons. Key findings of the research are diverse. -
World Bank Document
43176 v3 Public Disclosure Authorized Public Disclosure Authorized Public Disclosure Authorized Public Disclosure Authorized MINISTRY OF AGRICULTURE COMPREHENSIVE ASSESSMENT OF THE AGRICULTURE SECTOR IN LIBERIA (CAAS-Lib) Volume 2.2 - Sub-Sector Reports Liberia 2007 CAAS-Lib Sub-Sector Reports Volume 2.2 TABLE OF CONTENTS I. LAND AND WATER MANAGEMENT COMPONENT ...............................................3 EXECUTIVE SUMMARY ...................................................................................................3 1. Introduction..................................................................................................................16 2. Terms of Reference......................................................................................................16 3. Background..................................................................................................................16 4. Water Resources Legislation and Administration in Liberia.......................................18 4.1 Water resources legislation.................................................................................18 4.2 Water resources administration and institutions.................................................19 4.3 Agricultural water management..........................................................................22 4.4 Hydrometeorology ..............................................................................................23 4.5 Surface water ......................................................................................................25 -
World Food Programme Liberia
WWWOOORRRLLLDDD FFFOOOOOODDD PPPRRROOOGGGRRRAAAMMMMMMEEE LLLIIIBBBEEERRRIIIAAA Grand Gedeh County FOOD SECURITY AND NUTRITION SURVEY TABLE OF CONTENTS 3 Acknowledgement 3 Executive Summary 4 Background and Introduction Economy of Grand Gedeh County Survey justification Objectives and methodology 7 Part I—Community Level Findings Demographic information Land and resource access Education services Community perception of needs 10 Part II—Household Level Findings Household Demography Household Circumstances Housing Assets ownership Agriculture Sources of Incomes Household Expenditures Frequency of food consumption Food aid Shocks and coping strategies 17 Part III—Nutrition and Health Child nutritional status Health services HIV/AIDS knowledge 26 Part IV—Household Food Security and Consumption Typologies Classification by Food consumption Description of the consumption groups 30 Recommendations 31 Appendices Page 2 of 51 ACKNOWLEDGEMENT households were assessed. Food security, nutrition, mortality and other health indicators were collected WFP Liberia sponsored the Grand Gedeh County during the assessment. Food Security and Nutrition Survey in March 2005. WFP wishes to acknowledge the assistance provided The assessment indicates unstable food security by Government counterparts, NGOs and UN sister situation in the county. The survey reveals that some agencies. In particular, WFP is grateful to LRRRC and populations are not attaining adequate food ICRC in providing basic statistics and population consumption levels; characterized by low food figures, which were crucial for the development of the diversity, high proportion (over 60%) of household sampling frame and cluster identification. UNICEF’s expenditure used for food purchases at the expense support in the training of enumerators and supervision of other basic needs, low frequency of daily food of the whole exercise is also appreciated. -

Liberia August 2016 Livelihood Zones
Liberia August 2016 Livelihood Zones The present document has been produced with the funding from the European Union. The contents of the document are the responsibility of its author and do not necessarily reflect the views of the European Union. Table of Contents ACKNOWLEDGEMENTS / BACKGROUND ................................................................................. 3 ACRONYMS AND ABBREVIATIONS ............................................................................................ 4 INTRODUCTION................................................................................................................................ 5 ZONE 01: Gold and Diamond Mining Livelihood Zone ..................................................... 13 Zone 02: Coastal Fishing Livelihood Zone ........................................................................... 15 ZONE 03: Northern Border Cocoa and Coffee Livelihood Zone ..................................... 17 ZONE 04: Rubber, Palm Oil and Iron Ore Concession Livelihood Zone ...................... 19 ZONE 05: North and Northeast Rice Farming and Wild Palm Livelihood Zone ....... 20 ZONE 06: River Cess Rice and Cassava Farming Livelihood Zone ................................ 21 ZONE 07: Southeast Rice and Cassava Farming Livelihood Zone ................................. 23 ZONE 08: Coastal Plain Cassava with Rice and Inland Fishing Livelihood Zone ..... 25 ZONE 09: Vegetable Gardening and Rice Farming Livelihood Zone ............................ 27 ZONE 10: Charcoal Livelihood Zone ....................................................................................... -
A-Ai565e.Pdf
MINISTRY OF AGRICULTURE COMPREHENSIVE ASSESSMENT OF THE AGRICULTURE SECTOR IN LIBERIA (CAAS-Lib) Volume 2.2 - Sub-Sector Reports Liberia 2007 CAAS-Lib Sub-Sector Reports Volume 2.2 TABLE OF CONTENTS I. LAND AND WATER MANAGEMENT COMPONENT ...............................................3 EXECUTIVE SUMMARY ...................................................................................................3 1. Introduction..................................................................................................................16 2. Terms of Reference......................................................................................................16 3. Background..................................................................................................................16 4. Water Resources Legislation and Administration in Liberia.......................................18 4.1 Water resources legislation.................................................................................18 4.2 Water resources administration and institutions.................................................19 4.3 Agricultural water management..........................................................................22 4.4 Hydrometeorology..............................................................................................23 4.5 Surface water ......................................................................................................25 4.6 Groundwater .......................................................................................................26 -

Liberian Studies Journal
VOLUME XXVIII 2003 Number 2 LIBERIAN STUDIES JOURNAL Published by THE LIBERIAN STUDIES ASSOCIATION, INC. VOLUME XXVIX 2004 Number 1 PDF compression, OCR, web optimization using a watermarked evaluation copy of CVISION PDFCompressor LIBERIAN STUDIES JOURNAL Editorial Policy The Liberian Studies Journal is dedicated to the publication of original research on social, politi- cal, economic, scientific, and other issues about Liberia or with implications for Liberia. Opin- ions of contributors to the Journal do not necessarily reflect the policy of the organizations they represent or the Liberian Studies Association, publisher of the Journal. Manuscript Requirements Manuscripts submitted for publication should not exceed 25 typewritten, double-spaced pages, with margins of one-and a-half inches. The page limit includes graphs, references, tables and appendices. Authors may, in addition to their manuscripts, submit a computer disk of their work preferably in MS Word 2000 or WordPerfect 6.1 for Windows. Notes and references should be placed at the end of the text with headings, e.g., Notes; References. Notes, if any, should precede the references. The Journal is published in June and December. Deadline for the first issue is February, and for the second, August. Manuscripts should include a cover page that provides the title of the text, author's name, address, phone number, e-mail address, and affiliation. Anonymous referees will review all works. Manuscripts are accepted in English and French. Manuscripts must conform to the editorial style of either the Chicago Manual of Style, or The American Psychological Association (APA), or Modern Language Association (MLA). Authors should send their manuscripts for consideration by regular mail or e-mail attachments to: Amos J. -

1848 Ministries and Agencies in Liberia Name
Ministries and Agencies in Liberia Ministry of Foreign Affairs Creation: 1848 Name: Its current, Ministry of Foreign Affairs, came into being in 1972 Former Name: Department of State (DoS). The DoS was headed, initially, by a Secretary of State. Hilary Teague, who also drafted the Liberian Declaration of Independence, became Liberia’s first secretary of State in 1848. Current Function: It implements Liberia’s external policies and relations and manages its Diplomatic missions accredited abroad. Former Function: Same as the new function Order of Succession: 3. The Minister of Foreign Affairs is the dean of the cabinet and therefore ascends to the presidency after the Speaker of the House of Representatives and the Pro Tempore of the Liberian Senate. Employees: Outlays: Ministry of Finance & Development Planning Creation: 2014 Name: Ministry of Finance & Development Planning Former Name: Ministry of Finance Function: MFDP formulates and administers economic development, fiscal and tax policies for the promotion of sound and efficient management of the financial resources of the Government, administers the revenue program of the Government, including supervision of the collection of the revenues; reports the financial activities and financial position of the Government to the President and the Legislature; maintains the central accounting records of the Government and prescribe for all Government agencies of accounts reporting and documentation necessary to safeguard the assets of the Government. MFDP also formulates fiscal policies for