Motion Palpation Assessment of the Sacroiliac Joint
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Synovial Joints Permit Movements of the Skeleton
8 Joints Lecture Presentation by Lori Garrett © 2018 Pearson Education, Inc. Section 1: Joint Structure and Movement Learning Outcomes 8.1 Contrast the major categories of joints, and explain the relationship between structure and function for each category. 8.2 Describe the basic structure of a synovial joint, and describe common accessory structures and their functions. 8.3 Describe how the anatomical and functional properties of synovial joints permit movements of the skeleton. © 2018 Pearson Education, Inc. Section 1: Joint Structure and Movement Learning Outcomes (continued) 8.4 Describe flexion/extension, abduction/ adduction, and circumduction movements of the skeleton. 8.5 Describe rotational and special movements of the skeleton. © 2018 Pearson Education, Inc. Module 8.1: Joints are classified according to structure and movement Joints, or articulations . Locations where two or more bones meet . Only points at which movements of bones can occur • Joints allow mobility while preserving bone strength • Amount of movement allowed is determined by anatomical structure . Categorized • Functionally by amount of motion allowed, or range of motion (ROM) • Structurally by anatomical organization © 2018 Pearson Education, Inc. Module 8.1: Joint classification Functional classification of joints . Synarthrosis (syn-, together + arthrosis, joint) • No movement allowed • Extremely strong . Amphiarthrosis (amphi-, on both sides) • Little movement allowed (more than synarthrosis) • Much stronger than diarthrosis • Articulating bones connected by collagen fibers or cartilage . Diarthrosis (dia-, through) • Freely movable © 2018 Pearson Education, Inc. Module 8.1: Joint classification Structural classification of joints . Fibrous • Suture (sutura, a sewing together) – Synarthrotic joint connected by dense fibrous connective tissue – Located between bones of the skull • Gomphosis (gomphos, bolt) – Synarthrotic joint binding teeth to bony sockets in maxillae and mandible © 2018 Pearson Education, Inc. -

Between Ligamentous Structures in the Thoracic Spine : a finite Element Investigation
View metadata, citation and similar papers at core.ac.uk brought to you by CORE provided by Queensland University of Technology ePrints Archive This is the author’s version of a work that was submitted/accepted for pub- lication in the following source: Little, J. Paige & Adam, Clayton J. (2011) Effects of surgical joint desta- bilization on load sharing between ligamentous structures in the thoracic spine : a finite element investigation. Clinical Biomechanics, 26(9), pp. 895-903. This file was downloaded from: http://eprints.qut.edu.au/48159/ c Copyright 2011 Elsevier Ltd. NOTICE: this is the author’s version of a work that was accepted for publication in the journal Clinical Biomechanics. Changes resulting from the publishing process, such as peer review, editing, corrections, struc- tural formatting, and other quality control mechanisms may not be re- flected in this document. Changes may have been made to this work since it was submitted for publication. A definitive version was sub- sequently published in Clinical Biomechanics 26 (2011) 895–903, DOI: 10.1016/j.clinbiomech.2011.05.004 Notice: Changes introduced as a result of publishing processes such as copy-editing and formatting may not be reflected in this document. For a definitive version of this work, please refer to the published source: http://dx.doi.org/10.1016/j.clinbiomech.2011.05.004 *Manuscript (including title page & abstract) Effect of surgical joint destabilization on ligament load-sharing 1 Effects of surgical joint destabilization on load sharing 2 between ligamentous structures in the thoracic spine: A 3 Finite Element investigation 4 5 Authors: 6 J. -

Canine Thoracic Costovertebral and Costotransverse Joints Three Case Reports of Dysfunction and Manual Therapy Guidelines for A
Topics in Compan An Med 29 (2014) 1–5 Topical review Canine Thoracic Costovertebral and Costotransverse Joints: Three Case Reports of Dysfunction and Manual Therapy Guidelines for Assessment and Treatment of These Structures Laurie Edge-Hughes, BScPT, MAnimSt (Animal Physiotherapy), CAFCI, CCRTn Keywords: The costovertebral and costotransverse joints receive little attention in research. However, pain costovertebral associated with rib articulation dysfunction is reported to occur in human patients. The anatomic costotransverse structures of the canine rib joints and thoracic spine are similar to those of humans. As such, it is ribs physical therapy proposed that extrapolation from human physical therapy practice could be used for the assessment and rehabilitation treatment of the canine patient with presumed rib joint pain. This article presents 3 case studies that manual therapy demonstrate signs of rib dysfunction and successful treatment using primarily physical therapy manual techniques. General assessment and select treatment techniques are described. & 2014 Elsevier Inc. All rights reserved. The Canine Fitness Centre Ltd, Calgary, Alberta, Canada nAddress reprint requests to Laurie Edge-Hughes, BScPT, MAnimSt (Animal Physiotherapy), CAFCI, CCRT, The Canine Fitness Centre Ltd, 509—42nd Ave SE, Calgary, Alberta, Canada T2G 1Y7 E-mail: [email protected] The articular structures of the thorax comprise facet joints, the erect spine and further presented that in reviewing the literature, intervertebral disc, and costal joints. Little research has been they were unable to find mention of natural development of conducted on these joints in human or animal medicine. However, idiopathic scoliosis in quadrupeds; however, there are reports of clinical case presentations in human journals, manual therapy avian models and adolescent models in man. -

Posterior Longitudinal Ligament Status in Cervical Spine Bilateral Facet Dislocations
Thomas Jefferson University Jefferson Digital Commons Department of Orthopaedic Surgery Faculty Papers Department of Orthopaedic Surgery November 2005 Posterior longitudinal ligament status in cervical spine bilateral facet dislocations John A. Carrino Harvard Medical School & Brigham and Women's Hospital Geoffrey L. Manton Thomas Jefferson University Hospital William B. Morrison Thomas Jefferson University Hospital Alex R. Vaccaro Thomas Jefferson University Hospital and The Rothman Institute Mark E. Schweitzer New York University & Hospital for Joint Diseases Follow this and additional works at: https://jdc.jefferson.edu/orthofp Part of the Orthopedics Commons LetSee next us page know for additional how authors access to this document benefits ouy Recommended Citation Carrino, John A.; Manton, Geoffrey L.; Morrison, William B.; Vaccaro, Alex R.; Schweitzer, Mark E.; and Flanders, Adam E., "Posterior longitudinal ligament status in cervical spine bilateral facet dislocations" (2005). Department of Orthopaedic Surgery Faculty Papers. Paper 3. https://jdc.jefferson.edu/orthofp/3 This Article is brought to you for free and open access by the Jefferson Digital Commons. The Jefferson Digital Commons is a service of Thomas Jefferson University's Center for Teaching and Learning (CTL). The Commons is a showcase for Jefferson books and journals, peer-reviewed scholarly publications, unique historical collections from the University archives, and teaching tools. The Jefferson Digital Commons allows researchers and interested readers anywhere in the world to learn about and keep up to date with Jefferson scholarship. This article has been accepted for inclusion in Department of Orthopaedic Surgery Faculty Papers by an authorized administrator of the Jefferson Digital Commons. For more information, please contact: [email protected]. -

Chapter 02: Netter's Clinical Anatomy, 2Nd Edition
Hansen: Netter's Clinical Anatomy, 2nd Edition - with Online Access 2 BACK 1. INTRODUCTION 4. MUSCLES OF THE BACK REVIEW QUESTIONS 2. SURFACE ANATOMY 5. SPINAL CORD 3. VERTEBRAL COLUMN 6. EMBRYOLOGY FINAL 1. INTRODUCTION ELSEVIERl VertebraeNOT prominens: the spinous process of the C7- vertebra, usually the most prominent The back forms the axis (central line) of the human process in the midline at the posterior base of body and consists of the vertebral column, spinal cord, the neck supporting muscles, and associated tissues (skin, OFcon- l Scapula: part of the pectoral girdle that sup- nective tissues, vasculature, and nerves). A hallmark of ports the upper limb; note its spine, inferior human anatomy is the concept of “segmentation,” and angle, and medial border the back is a prime example. Segmentation and bilat l Iliac crests: felt best when you place your eral symmetry of the back will be obvious as you hands “on your hips”; an imaginary horizontal study the vertebral column, the distribution of the line connecting the crests passes through the spinal nerves, the muscles of th back, and its vascular spinous process of the L4 vertebra and the supply. intervertebral disc of L4-L5, a useful landmark Functionally, the back is involved in three primary for a lumbar puncture or epidural block tasks: l Posterior superior iliac spines: an imaginary CONTENThorizontal line connecting these two points l Support: the vertebral column forms the axis of passes through the spinous process of S2 (second the body and is critical for our upright posture sacral segment) (standing or si ting), as a support for our head, as an PROPERTYattachment point and brace for move- 3. -

Successful Treatment of Supraspinous and Interspinous Ligament Injury with Ultrasound-Guided Platelet-Rich Plasma Injection
HSSXXX10.1177/1556331621992312HSS Journal®: The Musculoskeletal Journal of Hospital for Special SurgeryCreighton et al 992312case-report2021 Case Report HSS Journal®: The Musculoskeletal Journal of Hospital for Special Surgery Successful Treatment of Supraspinous 1 –4 © The Author(s) 2021 Article reuse guidelines: and Interspinous Ligament Injury sagepub.com/journals-permissions DOI:https://doi.org/10.1177/1556331621992312 10.1177/1556331621992312 With Ultrasound-Guided Platelet-Rich journals.sagepub.com/home/hss Plasma Injection: Case Series Andrew Creighton, DO1, Roger A. Sanguino, MS1, Jennifer Cheng, PhD1, and James F. Wyss, MD, PT1 Keywords supraspinous ligament, interspinous ligament, platelet-rich plasma, ultrasound, nonoperative treatments, lumbar spine Received October 18, 2020. Accepted October 21, 2020. Introduction running volume. The LBP intensity ranged from 3 to 9/10 and was worse with prolonged standing, sitting, or running. Low back pain (LBP) is a very common complaint and is He reported no improvement with 3 prior courses of PT, now the number one cause of disability across the globe NSAIDs, and use of a seat cushion. Physical examination [5,13]. Both the supraspinous ligament (SSL) and interspi- revealed mild right thoracolumbar curvature. Tenderness nous ligament (ISL) form part of the posterior ligamentous was appreciated over the L5 spinous process and interspi- complex, which is believed to play an integral role in the nous region above and below L5. Strength, sensation, and stability of the thoracolumbar spine [8]. The SSL begins at reflexes were normal. the C7 spinous process and extends to L3 and L4 in 22% Radiographs were unremarkable. Magnetic resonance and 74% of adults, respectively [11]. -

Supraspinous Ligament Sprains
Unraveling the Mystery of Low Back Pain #5: Supraspinous Ligament Sprains Instructor: Ben Benjamin, Ph.D. Instructor: Ben Benjamin, Ph.D. [email protected] 1 SPONSOREDSPONSORED BY:BY: Over 30 years of experience building the finest portable treatment tables and accessories. Products that are visually stimulating, ergonomically supportive, and incredibly comfortable. The superior design and engineering capabilities merge to create the ultimate experience for you and your clients. www.oakworks.com 717.235.6807 SPONSOREDSPONSORED BY:BY: Mattes chair Side-lying position system Webinar Goal Explore the assessment and treatment of supraspinous ligament injuries: • Supraspinous ligaments L1-L5 • Suprasacral ligaments 2 Pretest 1. The supraspinous ligament is also known as the supraspinal ligament. True or False? 2. The suprasacral ligament connects the sacrum to the ilium. True or False? 3. The interspinous ligament is not continuous from vertebra to vertebra; it only connects two spinous processes to each other. True or False? 4. The supraspinous ligament in the low back limits lumbar flexion. True or False? 5. The posterior layer of thoracolumbar fascia and multifidus muscles combine to form the lumbar supraspinous ligaments. True or False? 6. The suprasacral ligament holds the sacrum to the pelvis. True or False? Anatomy Anatomy of the Supraspinous Ligaments • Connect all five lumbar vertebrae • Connect L5 to the sacrum • Sometimes called the supraspinal ligaments 3 Anatomy of the Supraspinous Ligaments • Run between the tips of the spinous -

The Lumbosacral Dorsal Rami of the Cat
J. Anat. (1976), 122, 3, pp. 653-662 653 With 1O figures Printed in Great Britain The lumbosacral dorsal rami of the cat NIKOLAI BOGDUK Department ofAnatomy, University ofSydney, Sydney, Australia (Accepted 2 December 1975) INTRODUCTION Several reflexes involving dorsal rami have been demonstrated in the cat (Pedersen, Blunck & Gardner, 1956; Bogduk & Munro, 1973). However, there is no adequate description in the literature of the anatomy of lumbosacral dorsal rami in this animal. The present study was therefore undertaken to provide such a description, hoping thereby to facilitate the design and interpretation of our own (Bogduk & Munro, 1973) and future research on reflexes involving lumbosacral dorsal rami, including reflexes possibly relevant to the understanding of back pain in man. These nerves are described in the present study in relation to a revised nomen- clature of the muscles in the dorsal lumbar region. Such a revision (Bogduk, 1975) was necessary because of the different nomenclatures and varied interpretations in the literature. METHODS Six laboratory cats (Felis domesticus) were embalmed with 10° formalin and studied by gross dissection. In addition, confirmatory observations were made on another 16 cats in the course of surgical procedures. Lateral branches of dorsal rami were first identified during reflexion of the skin and then during the resection of iliocostalis and longissimus lumborum. These branches were subsequently traced back to their origins from the dorsal rami, a dissecting microscope being used. The medial branches of the dorsal rami were then traced through the intertransversarii mediales into multifidus. Sinuvertebral nerves were also sought. Nerve roots were detached from the spinal cord before removing it from the vertebral canal. -
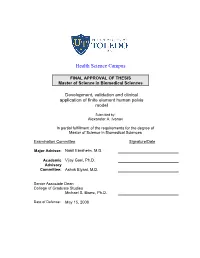
Development, Validation and Clinical Application of Finite Element Human Pelvis Model
Health Science Campus FINAL APPROVAL OF THESIS Master of Science in Biomedical Sciences Development, validation and clinical application of finite element human pelvis model Submitted by: Alexander A. Ivanov In partial fulfillment of the requirements for the degree of Master of Science in Biomedical Sciences Examination Committee Signature/Date Major Advisor: Nabil Ebraheim, M.D. Academic Vijay Goel, Ph.D. Advisory Committee: Ashok Biyani, M.D. Senior Associate Dean College of Graduate Studies Michael S. Bisesi, Ph.D. Date of Defense: May 15, 2008 A Thesis Entitled Development, Validation and Clinical Application of the Finite Element Model of Human Pelvis. By Alexander A. Ivanov, M.D. Submitted as partial fulfillment of the requirements for the Master of Science in Orthopaedic Science ______________________________ Advisor: Dr. Nabil A. Ebraheim, M.D. ______________________________ Co-Advisor: Dr. Vijay K. Goel, Ph.D. ______________________________ Graduate School The University of Toledo 2008 1 © 2008, Alexander A. Ivanov 2 College of Health Science I HEREBY RECOMMEND THAT THE THESIS PREPARED UNDER MY SUPERVISION BY: Alexander A Ivanov, M.D. ENTITLED: Development, validation and clinical application of finite element human pelvis model BE ACCEPTED IN PARTIAL FULFILLMENT OF THE REQUIREMENTS FOR THE DEGREE OF: Master of Science in Orthopaedic Science ______________________________________________________________ Thesis Advisor: Dr. Nabil A. Ebraheim, M.D. _______________________________________________________________ Thesis Co-Advisor: Dr. Vijay K. Goel, Ph.D. Recommendation concurred by: ___________________________________ Committee Dr.Ashok Biyani, M.D. Of Final Examination ________________________________________________________________ Dean, College of Health Science 3 Acknowledgment I would like to extend my gratitude to my advisors Dr. Nabil Ebraheim and Dr. Vijay Goel for their incredible support of this work. -

Effects of Different Angles of the Traction Table on Lumbar Spine Ligaments: a Finite Element Study Hekmat Farajpour, MS, Nima Jamshidi, Phd
Original Article Clinics in Orthopedic Surgery 2017;9:480-488 • https://doi.org/10.4055/cios.2017.9.4.480 Effects of Different Angles of the Traction Table on Lumbar Spine Ligaments: A Finite Element Study Hekmat Farajpour, MS, Nima Jamshidi, PhD Department of Biomedical Engineering, Faculty of Engineering, University of Isfahan, Isfahan, Iran Background: The traction bed is a noninvasive device for treating lower back pain caused by herniated intervertebral discs. In this study, we investigated the impact of the traction bed on the lower back as a means of increasing the disc height and creating a gap between facet joints. Methods: Computed tomography (CT) images were obtained from a female volunteer and a three-dimensional (3D) model was cre- ated using software package MIMICs 17.0. Afterwards, the 3D model was analyzed in an analytical software (Abaqus 6.14). The study was conducted under the following traction loads: 25%, 45%, 55%, and 85% of the whole body weight in different angles. Results: Results indicated that the loading angle in the L3–4 area had 36.8%, 57.4%, 55.32%, 49.8%, and 52.15% effect on the anterior longitudinal ligament, posterior longitudinal ligament, intertransverse ligament, interspinous ligament, and supraspinous ligament, respectively. The respective values for the L4–5 area were 32.3%, 10.6%, 53.4%, 56.58%, and 57.35%. Also, the body weight had 63.2%, 42.6%, 44.68%, 50.2%, and 47.85% effect on the anterior longitudinal ligament, posterior longitudinal liga- ment, intertransverse ligament, interspinous ligament, and supraspinous ligament, respectively. The respective values for the L4–5 area were 67.7%, 89.4%, 46.6%, 43.42% and 42.65%. -

Anatomy of the Spine
Anatomy of the Spine Musculoskeletal block- Anatomy-lecture 4 Editing file Color guide : Objectives Only in boys slides in Blue Only in girls slides in Purple By the end of this lecture you should be able to: important in Red Doctor note in Green ✓ Distinguish and describe the cervical, thoracic, lumbar, sacral and Extra information in Grey coccygeal vertebrae. ✓ Describe the vertebral curvatures. ✓ Describe the movement which occur in each region of the vertebral column. ✓ List the structures which connect 2 adjacent vertebrae together. ✓ List and identify the ligaments of the intervertebral joints. Spine or Vertebral Column ● The vertebral column extends from the skull to the pelvis. ● It surrounds and protects the spinal cord and supports the whole body. ● It is formed from 33 irregular vertebrae. It consists of 24 single vertebrae and 2 bones: •Sacrum, (5 fused vertebrae).(Convex) •Coccyx, (4 fused vertebrae). Of the 24 single bones, •7 Cervical vertebrae (concave) •12 Thoracic vertebrae(convex) •5 Lumbar vertebrae.(concave) The single vertebrae are separated by pads of flexible fibrocartilage called the intervertebral disc. • The intervertebral discs cushion the vertebrae and absorb shocks. • The spinal curvature and discs make the body trunk flexible and prevent shock to head while walking or running. • We have 2 spinal curvatures: 1) Primary curvature (present at birth): Concave forward - Thoracic - Sacral regions 2) Secondary curvature (present after birth): Convex forward - Cervical (after the baby holds his head 6th month) - Lumbar (after walking around one year) 3 Typical Vertebra ● Any vertebra is made up of: 1) Body or Centrum: - disc-like weight bearing part that lies anteriorly 2) Vertebral Arch: - Formed from fusion of 2 pedicles and 2 laminae ● Vertebral foramen lies between the body and the vertebral foramen. -

Acoustic Emission Signals from Injuries of Three Vertebra Specimens
IRC-14-25 IRCOBI Conference 2014 Acoustic Emission Signals from Injuries of Three‐Vertebra Specimens Carolyn Van Toen, John Street, Thomas R. Oxland, Peter A. Cripton Abstract Although acoustic emission (AE) signals from isolated spinal ligament failures have lower amplitudes and frequencies than those from vertebral body fractures, it is not known if AE signals could be used to differentiate between injured structures in spine segment testing. The objectives of this study were to evaluate differences in AE signal amplitudes and frequencies resulting from injuries of various tissue types, tested as part of a spine segment, during dynamic loading. Three‐vertebra specimens from the human cadaver cervical spine were tested in dynamic eccentric axial compression with lateral eccentricities. Specimens were tested with low (n=6) and high (n=5) initial eccentricities of 5 and 150% of the lateral diameter of the vertebral body, respectively. AE signals were recorded using two sensors. The time of injury initiation was identified for seven vertebral body and/or endplate fractures and five intertransverse and/or facet capsule ruptures. Hard tissue injuries resulted in higher peak amplitude AE signals than soft tissue injuries. Characteristic frequencies of AE signals from the sensor on the concave side of the lateral bend from failures of hard tissues were greater than those from failure of soft tissues. These findings suggest that AE signals can assist in delineating injured structures of the spine. Keywords acoustic emission, experimental, ligament, spine, vertebra I. INTRODUCTION Cervical spine injuries are associated with substantial personal, social and economic costs [1‐5]. In order to reduce the risk of these injuries occurring, injury prevention devices, such as airbags and helmets, are designed and evaluated using spine injury tolerances [6‐8].