Studies on the Prevalence, Knowledge, and Practices Toward Malaria in Owerri West Local Government Area of Imo State, Nigeria
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

CURRICULUM VITAE Name: OSUAGWU, Linus Chukwunenye. Status: Professor & Former Vice Chancellor. Specialization: Business Admi
CURRICULUM VITAE Name: OSUAGWU, Linus Chukwunenye. Status: Professor & Former Vice Chancellor. Specialization: Business Administration/Marketing . Nationality: Nigerian. State of Origin: Imo State of Nigeria (Ihitte-Uboma LGA). Marital status: Married (with two children: 23 years; and 9 years). Contact address: School of Business & Entrepreneurship, American University of Nigeria,Yola, Adamawa State, Nigeria; Tel: +2348033036440; +2349033069657 E-mail: [email protected]; [email protected] Skype ID: linus.osuagwu; Twitter: @LinusOsuagwu Website: www.aun.edu.ng SCHOOLS ATTENDED WITH DATES: 1. Comm. Sec. School, Onicha Uboma, Ihitte/Uboma, Imo State, Nigeria (1975 - 1981). 2. Federal University of Technology Owerri, Nigeria, (1982 - 1987). 3. University of Lagos, Nigeria (1988 - 1989; 1990 - 1997). ACADEMIC QUALIFICATIONS: PhD Business Administration/Marketing (with Distinction), University of Lagos, Nigeria, (1998). M.Sc. Business Administration/Marketing, University of Lagos, Nigeria, (1990). B.Sc. Tech., Second Class Upper Division, in Management Technology (Maritime), Federal University of Technology Owerri (FUTO), Nigeria (1987). 1 WORKING EXPERIENCE: 1. Vice Chancellor, Eastern Palm University, Ogboko, Imo State, Nigeria (2017-2018). 2. Professor of Marketing, School of Business & Entrepreneurship, American University of Nigeria, Yola (May 2008-Date). 3. Professor of Marketing & Chair of Institutional Review Boar (IRB), American University of Nigeria Yola (2008-Date). 4. Professor of Marketing & Dean, School of Business & Entrepreneurship, American University of Nigeria, Yola (May 2013-May 2015). 4. Professor of Marketing & Acting Dean, School of Business & Entrepreneurship, American University of Nigeria (January 2013-May 2013) . 5. Professor of Marketing & Chair of Business Administration, Department of Business Administration, School of Business & Entrepreneurship, American University of Nigeria (2008-2013). 6. -

Imperatives of Entrepreneurship Education Amongst Library And
University of Nebraska - Lincoln DigitalCommons@University of Nebraska - Lincoln Library Philosophy and Practice (e-journal) Libraries at University of Nebraska-Lincoln January 2020 Imperatives of Entrepreneurship Education Amongst Library and Information Science Undergraduate in Nigeria: The Case Study of LIS Undergraduates in South-East and South-South Geopolitical Zones of Nigeria Nneka C. Agim Federal University of Technology, Owerri, [email protected] Follow this and additional works at: https://digitalcommons.unl.edu/libphilprac Part of the Library and Information Science Commons Agim, Nneka C., "Imperatives of Entrepreneurship Education Amongst Library and Information Science Undergraduate in Nigeria: The Case Study of LIS Undergraduates in South-East and South-South Geopolitical Zones of Nigeria" (2020). Library Philosophy and Practice (e-journal). 3907. https://digitalcommons.unl.edu/libphilprac/3907 Imperatives of Entrepreneurship Education Amongst Library and Information Science Undergraduate in Nigeria: The Case Study of LIS Undergraduates in South-East and South-South Geopolitical Zones of Nigeria Agim, Nneka Chinaemerem University Library Federal University of Technology, Owerri, Nigeria Email: [email protected] ABSTRACT Entrepreneurship education and its training is an important skill oriented education with prospects of creating self employment amongst students upon graduation and national development. Specifically, to be examined in this study are the available entrepreneurial courses in the curricular of library and information schools in both South-East and South-South Geopolitical zones of Nigeria, to determine the benefit of entrepreneurial courses for undergrad uates in library schools in South- East and South-South Geopolitical zones of Nigeria and to examine the factors affecting entrepreneurship education in library schools in South-East and South-South Geopolitical zone of Nigeria. -

Assessment of Physicochemical and Microbial Load of Nworie River Owerri, Imo State, South-Eastern Nigeria
IOSR Journal of Environmental Science, Toxicology and Food Technology (IOSR-JESTFT) e-ISSN: 2319-2402,p- ISSN: 2319-2399.Volume 10, Issue 6 Ver. I (Jun. 2016), PP 67-75 www.iosrjournals.org Assessment of Physicochemical and Microbial Load of Nworie River Owerri, Imo State, South-Eastern Nigeria Njoku –Tony, R.F1, Ebe, T.E2, Ihejirika, C.E3, Ejiogu, C.C4 Uyo, C.N5 Department of Environmental Technology Federal University of Technology, P.M.B 1526, Owerri. Nigeria Abstract: Investigations on the physicochemical properties and microbial load of Nworie River in Owerri Imo state, Nigeria was carried out between January and July, 2014. Water samples from 3 locations namely (Upstream Akwakuma), (Discharge pointFederal Medical Center) and (Downstream Holy Ghost College) were collected and taken to the laboratory for analysis. Temperature, Conductivity, pH, TDS, and DO were determined in-situ using Jenway (Model type HANNA 1910) Multipurpose tester. Microbial quality was determined using standard methods. Results showed that temperature, pH, dissolved solids, DO, BOD were all within the WHO standard. Analysis on microbial quality however revealed heavy presence of microbial contamination in the midstream (Discharge point). The total coliform count was highest at the midstream (FMC) and ranged from 80x105cfu/cm3 to 172x105cfu/cm3, and total faecal coliform count ranged from 8x105cfu/cm3 to 31x105cfu/cm3 while the least was recorded at the upstream (Akwakuma) with a total coliform range of 12x105 to 80x 105cfu/cm3 and total faecal coliform count that ranged from 4x105 to 22x105cfu/cm3. The results obtained showed the presence of Escherichia coli (8.18%), Staphylococcus spp(18.18%), Bacillus spp (21.09%), Klebsiellaspp (10.91%), Salmonella spp (1.82%), Proteus spp (8.18%), Pseudomonas spp (2.72%), Mucorspp(4.54%),Tricophytonspp (3.63%), Aspergillus fumigates (4.54%), Candida spp (2.72%), and Rhizopusspp (5.45%). -

River Basins of Imo State for Sustainable Water Resources
nvironm E en l & ta i l iv E C n g Okoro et al., J Civil Environ Eng 2014, 4:1 f o i n l Journal of Civil & Environmental e a e n r r i DOI: 10.4172/2165-784X.1000134 n u g o J ISSN: 2165-784X Engineering Review Article Open Access River Basins of Imo State for Sustainable Water Resources Management BC Okoro1*, RA Uzoukwu2 and NM Chimezie2 1Department of Civil Engineering, Federal University of Technology, Owerri, Imo State, Nigeria 2Department of Civil Engineering Technology, Federal Polytechnic Nekede, Owerri, Imo State, Nigeria Abstract The river basins of Imo state, Nigeria are presented as a natural vital resource for sustainable water resources management in the area. The study identified most of all the known rivers in Imo State and provided information like relief, topography and other geographical features of the major rivers which are crucial to aid water management for a sustainable water infrastructure in the communities of the watershed. The rivers and lakes are classified into five watersheds (river basins) such as Okigwe watershed, Mbaise / Mbano watershed, Orlu watershed, Oguta watershed and finally, Owerri watershed. The knowledge of the river basins in Imo State will help analyze the problems involved in water resources allocation and to provide guidance for the planning and management of water resources in the state for sustainable development. Keywords: Rivers; Basins/Watersheds; Water allocation; • What minimum reservoir capacity will be sufficient to assure Sustainability adequate water for irrigation or municipal water supply, during droughts? Introduction • How much quantity of water will become available at a reservoir An understanding of the hydrology of a region or state is paramount site, and when will it become available? In other words, what in the development of such region (state). -

Quantification of Heavy Metals Using Contamination and Pollution Index in Selected Refuse Dumpsites in Owerri, Imo State Southeast Nigeria Onwudike, S
International Journal of Environment, Agriculture and Biotechnology (IJEAB) Vol-2, Issue-3, May -Jun- 2017 http://dx.doi.org/10.22161/ijeab/2.3.25 ISSN: 2456-1878 Quantification of Heavy Metals using Contamination and Pollution Index in Selected Refuse Dumpsites in Owerri, Imo State Southeast Nigeria Onwudike, S. U1, Igbozurike, C. I2, Ihem, E. E1., Osisi F. A.1, Ukah, C. I1 1Department of Soil Science and Technology, Federal University of Technology Owerri, Imo State Nigeria 2Department of Soil Science and Environment, Imo State University Owerri, Nigeria Corresponding author: Dr. S. U. Onwudike, Department of Soil Science and Technology, Federal University of Technology Owerri, Imo State Nigeria. Running title: Contamination and pollution level of heavy metals at dumpsites. Abstract— Many sites in urban cities are used for resulted to generation of large agricultural and municipal dumping of domestic, industrial and municipal wastes wastes [1]. Most often, people deposit these wastes on or because of high human population density in the area. along the road sides, unapproved areas, open dumpsites in Most often, people use these dumpsites for growing of the markets or in water ways [2] and management of these crops without knowing the level of heavy metal wastes has been an environmental challenge to Nigerian contamination in soils of these areas. This study governmental [3]. Inappropriate disposal of these wastes evaluated the quantification and contamination level of causes environmental pollution and contamination of heavy metals in some refuse dumpsites in communities of underground and surface water bodies [4]. Research the State Nigeria. Three replicate soil samples were works have shown that heavy metals such as lead, collected from the dumpsites and at 20 m away from the cadmium, nickel, manganese and chromium amongst non - dumpsite which do not receive sewage water within others are responsible for certain diseases in man [5]. -

NIGERIA, JAHR 2020: Kurzübersicht Über Vorfälle Aus Dem Armed Conflict Location & Event Data Project (ACLED) Zusammengestellt Von ACCORD, 25
NIGERIA, JAHR 2020: Kurzübersicht über Vorfälle aus dem Armed Conflict Location & Event Data Project (ACLED) zusammengestellt von ACCORD, 25. März 2021 Anzahl der berichteten Vorfälle mit mindestens einem Anzahl der berichteten Todesopfer Todesopfer Staatsgrenzen: GADM, 6. Mai 2018a; Verwaltungsgliederung: GADM, 6. Mai 2018b; Vorfallsda- ten: ACLED, 12. März 2021; Küstenlinien und Binnengewässer: Smith und Wessel, 1. Mai 2015 NIGERIA, JAHR 2020: KURZÜBERSICHT ÜBER VORFÄLLE AUS DEM ARMED CONFLICT LOCATION & EVENT DATA PROJECT (ACLED) ZUSAMMENGESTELLT VON ACCORD, 25. MÄRZ 2021 Inhaltsverzeichnis Konfliktvorfälle nach Kategorie Anzahl der berichteten Todesopfer 1 Anzahl der Vorfälle mit Anzahl der Anzahl der Anzahl der berichteten Vorfälle mit mindestens einem Todesopfer 1 Kategorie mindestens Vorfälle Todesopfer einem Konfliktvorfälle nach Kategorie 2 Todesopfer Entwicklung von Konfliktvorfällen von 2012 bis 2020 2 Gewalt gegen Zivilpersonen 1045 605 2280 Proteste 858 16 40 Methodologie 3 Kämpfe 844 627 3336 Berichtete Konfliktvorfälle nach Provinz 4 Ausschreitungen 297 112 204 Explosionen / Fernangriffe 220 188 1900 Lokalisierung der Konfliktvorfälle 4 strategische Entwicklungen 80 0 0 Hinweis 9 Gesamt 3344 1548 7760 Die Tabelle basiert auf Daten von ACLED (verwendete Datensätze: ACLED, 12. März 2021). Entwicklung von Konfliktvorfällen von 2012 bis 2020 Das Diagramm basiert auf Daten von ACLED (verwendete Datensätze: ACLED, 12. März 2021). 2 NIGERIA, JAHR 2020: KURZÜBERSICHT ÜBER VORFÄLLE AUS DEM ARMED CONFLICT LOCATION & EVENT DATA PROJECT (ACLED) ZUSAMMENGESTELLT VON ACCORD, 25. MÄRZ 2021 Methodologie Die geographischen Kartendaten basieren hauptsächlich auf GADM, fallweise ergänzt durch weitere Quellen. Die Vorfälle werden den von ACLED genannten Die Daten, die in diesem Bericht verwendet werden, stammen vom Armed Conflict Provinzen zugeordnet (Provinznamen und -grenzen können sich zwischen ACLED Location & Event Data Project (ACLED). -

Characteristics of Leachate at Ihiagwa Dumpsite, Imo State Nigeria and Their Implications for Surface Water Pollution
International Journal of Advanced Academic Research | ISSN: 2488-9849 Vol. 7, Issue 3 (March, 2021) | www.ijaar.org Journal DOI: www.doi.org/10.46654/ij.24889849 Article DOI: www.doi.org/10.46654/ij.24889849.e7223 CHARACTERISTICS OF LEACHATE AT IHIAGWA DUMPSITE, IMO STATE NIGERIA AND THEIR IMPLICATIONS FOR SURFACE WATER POLLUTION Nelson-Kalu, C.T1; Amangabara, G.T1; Owuama, C.O.1, Nzeh, C.N and Uyo, C.N Department of Environmental Management, Federal University of Technology, Owerri. [email protected], [email protected] ABSTRACT Open dumpsite is the most common way to eliminate solid urban wastes in this part of the world. An important problem associated to landfills and open dumpsite is the production of leachates. The leachates from these dumpsites have many toxic substances, which may adversely affect the environmental health. Thus in order to have a better management of characteristics of Ihiagwa-Nekede waste dump leachates, representative leachate samples were collected and analyzed for Physico-chemical properties and levels of heavy metals in them. Results indicate pH7.38, temperature 28.30 ℃ - 28.40℃, total dissolved solid 124.01mg/l-125.45mg/l, magnesium hardness 4.40mg/l-7.32mg/l, sulphate 3.60mg/l- 3.70mg/l, and nitrate 27.00mg/l-27.60mg/l. Other parameters indicated as follows Conductivity1910휇푠/푐푚-1930.00 휇푠/푐푚, total chloride 891.72mg/l-891.74mg/l, carbonate 1708.00mg/l-1904.00mg/l, Ammonia 9.39mg/l-9.40mg/l, calcium hardness 373.17mg/l- 375.61mg/l, total solid 2423.00mg/l-2454.00mg/l, phosphate 13.52mg/l-13.54mg/l. -

Coverage of Llin Among Expectant Mothers in Nwangele, Imo State, Nigeria
OPEN ACCESS International Journal of Applied Biology International Journal of Applied Biology is licensed under a ISSN : 2580-2410 Creative Commons Attribution 4.0 International License, which permits unrestricted use, distribution, and reproduction in any eISSN : 2580-2119 medium, provided the original work is properly cited. Coverage of Llin Among Expectant Mothers in Nwangele, Imo State, Nigeria Chiagoziem Ogazirilem Emerole1*, Dr. Salome Ibe1, Dr. Uchechukwu Madukaku Chukwuocha1, Prof. Eunice Nwoke1, Prof. Ikechukwu Dozie1, Prof. Okwuoma Abanobi1 1Department of Public Health, School of Health Technology, Federal University of Technology, Owerri, Imo State, Nigeria. PMB 1526 Abstract Background: long-lasting insecticide-treated nets (LLINs) is one of the major interventions for the control and elimination of malaria, especially among Article History pregnant women. Received 12 April 2021 Aim: This study aimed to evaluate the knowledge, occurrence of malaria, Accepted 03 July 2021 utilisation and acquisition of long lasting insecticide treated net (LLINs) among pregnant women in Nwangele L.G.A. Imo State. Method: This was a cross-sectional study among women attending antenatal Keyword care in a primary health facility in Nwangele LGA, Imo State, Nigeria. A total of LLIN, Malaria, Nigeria, 150 women were interviewed using structured questionnaire to obtain Maternal health, Public information on their knowledge and the coverage of LLINs. Data analysis was Health done using SPSS version 20. Results: The mean age of the women was 29years. Most (81.3%) of the respondents had at least a secondary education. 92% used the LLINs at night time. Cost of acquiring these nets were free and in good condition (97.3%). -

Determination of Aquifer Potentials of Abia State University Uturu (ABSU
Journal of Geology and Mining Research Vol. 3(10), pp. 251-264, October 2011 Available online at http://www.academicjournals.org/JGMR ISSN 2006-9766 ©2011 Academic Journals Full Length Research Paper Determination of aquifer potentials of Abia State University, Uturu (ABSU) and its environs using vertical electrical sounding (VES) M. U. Igboekwe* and Akpan, C. B. Department of Physics, Micheal Okpara University of Agriculture, Umudike, P. M.B. 7267 Umuahia, Nigeria. Accepted 23 October, 2010 Resistivity soundings have been carried out around the Abia State University, Uturu (ABSU) and its environs, using the Schlumberger configuration. The major aim is to delineate potential aquifer zones for regional groundwater harvesting and further development. The geologic formations in the study area consist of a sequence of underlying Lower Coal Measures (Mamu), the Ajali formation and the upper coal measures (Nsukka formation). The Ajali formation, which is the most predominant in the sequence, consists of false-bedded poorly sorted sandstones. Twenty (20) vertical electrical soundings (VES) are taken with AB/2 = 500 m. The geoelectrical data analysis indicates the heterogenous nature of the aquifer with resistivity range between 2291.8 to 100,000 m. Assuming a homogeneous sandy aquifer, the average hydraulic conductivity (k) and transmissivity (Tr) distribution within the study area, are found to be 8.12 m/day and 1154.2 m2/day respectively. Based on these results, potential aquifer zones have been identified between Ugba junction (Uturu) and 200 m southeastward along Isukwuato- ABSU road. Key words: Abia State University Uturu (ABSU), aquifer, Schlumberger, VES, resistivity, transmissivity. INTRODUCTION Unlike surface water resources, the evaluation of population. -

4.Leonard Nwosu and Doris Ndubueze
Human Journals Research Article February 2017 Vol.:5, Issue:4 © All rights are reserved by Leonard Nwosu et al. Geoelectric Investigation of Water Table Variation with Surface Elevation for Mapping Drill Depths for Groundwater Exploitation in Owerri Metropolis, Imo State, Nigeria. Keywords: Water table, surface elevation, drill depth, resistivity, groundwater. ABSTRACT A total of 20 Vertical Electrical Soundings (VES) were *1Leonard Nwosu and 2Doris Ndubueze carried out in different locations in Owerri Metropolis, Imo state of Nigeria in order to investigate water table variation 1. Department of Physics University of Port with surface elevation for assessment of groundwater Harcourt, Nigeria. potential. Field data were acquired using the OHMEGA-500 resistivity meter and accessories. The Schlumberger electrode 2. Department of Physics Michael Okpara University configuration with maximum electrode spread of 700m was adopted. At each VES point, coordinates and elevations were of Agriculture Umudike, Nigeria. measured using the Global Positioning System (GPS). The field data were interpreted using the Advanced Geosciences Submission: 2 February 2017 Incorporation (AGI) 1D software and the Schlumberger automatic analysis version. The results revealed that the area Accepted: 7 February 2017 is underlain by multi geoelectric layers with about 6 to 9 Published: 25 February 2017 lithological units identified. The aquiferous layer is composed mainly of fine sand and sandstone units with low resistivity values recorded in Owerri West Area. The resistivity values ranged from 0.6Ωm to 1100.8Ωm. The depth to the water table varied across the area with surface elevation and ranged from 16.80m to 85.6m. Similarly, the aquifer thickness www.ijsrm.humanjournals.com ranged from 13.23m to 111.56m. -
History Doctrine
BY DANIEL AKA & OKEKE CHIKA JERRY ALL CHRISTIAN PRACTICAL PRAYING BAND (ACPPB) INTERNATIONAL HistoryAND DoctrinBY DANIEL AKA & OKEKE CHIKA JERReY ACPPB LOS ANGELES MAIN - OVERSEAS ZONAL HEADQUARTERS A U.S. NON-PROFIT RELIGIOUS ORGANZATION 9115 S VERMONT AVENUE, LOS ANGELES, CA 90044 P: 323 777 7507 | 323 753 3333 F: 323 778 5717 E: [email protected] www.acppb.cc MADAM SOPHIA O. NWOKOLO ELDER DANIEL CHUKA NWOKOLO CO-FOUNDER/SPIRITUAL DIRECTOR LEADER-GENERAL of ACPPB PART HistoryTABLE OF CONTENTS Introduction . 6 CHAPTER 1: Brief History of the Praying Band . 8 The Origin of Ekpere Ufuma . 9 Prophecy . 10 A Creation of Branches . 11 Visits of Various Dignitaries to Ufuma . 11 The Life in Nwokolos’s House . 12 Temptations . 14 The Death of Pa Nwokolo . 15 Pa Ofejebe’s Administration . 15 Elder Dan Nwokolo’s Aministration . 16 CHAPTER 2: Some Facts About ACPPB . 17 CHAPTER 3: History of the Bible Quiz Competition . 18 CHAPTER 4: Notable Dates in ACPPB . 19 CHAPTER 5: Some of the Key Officers in ACPPB . 24 CHAPTER 6: List of Zones, Zonal Headquarters & Zonal Leaders . 27 CHAPTER 7: Branches and their Leaders . 28 CHAPTER 8: Branches and Years of Establishment . 31 CHAPTER 9: Various Committees in ACPPB . 33 CHAPTER 10: Themes of Various Retreats in ACPPB . 37 CHAPTER 11: Part of the Constitution of ACPPB . 38 CHAPTER 12: Chapels and their Current Addresses . 44 of ACPPB PART DoctrinesTABLE OF CONTENTS CHAPTER 1: The Name Prayer House or “Ulo Ekepere” . 52 CHAPTER 2: How to Conduct Prayer Services . 52 The Chain of Conduction of Prayer Services . 55 CHAPTER 3: Admission of New Members . -
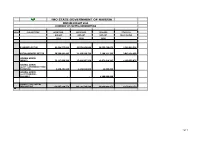
Imo State Government of Nigeria Revised Budget 2020 Summary of Capital Expenditure
IMO STATE GOVERNMENT OF NIGERIA REVISED BUDGET 2020 SUMMARY OF CAPITAL EXPENDITURE HEAD SUB-SECTORS APPROVED APPROVED REVISED COVID-19 BUDGET BUDGET BUDGET RESPONSIVE 2019 2020 2020 ECONOMIC SECTOR 82,439,555,839 63,576,043,808 20,555,468,871 2,186,094,528 SOCIAL SERVICES SECTOR 50,399,991,403 21,139,598,734 7,190,211,793 3,043,134,650 GENERAL ADMIN: (MDA'S) 72,117,999,396 17,421,907,270 12,971,619,207 1,150,599,075 GENERAL ADMIN: (GOVT COUNTERPART FUND PAYMENTS) 9,690,401,940 4,146,034,868 48,800,000 - GENERAL ADMIN: (GOVT TRANSFER - ISOPADEC) - - 4,200,000,000 - GRAND TOTAL CAPITAL EXPENDITURE 214,647,948,578 106,283,584,680 44,966,099,871 6,379,828,253 1of 1 IMO STATE GOVERNMENT OF NIGERIA IMO STATE GOVERNMENT OF NIGERIA REVISED BUDGET 2020 MINISTERIAL SUMMARY OF CAPITAL EXPENDITURE ECONOMIC SECTOR APPROVED 2019 APPROVED 2020 REVISED 2020 COVID-19 RESPONSIVE O414 MINISTRY OF AGRICULTURE AND FOOD SECURITY 1,499,486,000 2,939,000,000 1,150,450,000 - 0 AGRIC & FOOD SECURITY 1,499,486,000 0414-2 MINISTRY OF LIVESTOCK DEVELOPMENT 1,147,000,000 367,000,000 367,000,000 - 0 LIVESTOCK 1,147,000,000 697000000 1147000000 0414-1 MINISTRY OF ENVIRONMENT AND NATURAL RESOURCES 13,951,093,273 1,746,000,000 620,000,000 - 0 MINISTRY OF ENVIRONMENT 13951093273 450000000 O415 MINISTRY OF COMMERCE AND INDUSTRY 7,070,700,000 2,650,625,077 1,063,000,000 - -5,541,800,000 MINISTRY OF COMMERCE, INDUSTRY AND ENTREPRENEURSHIP1528900000 0419-2 MINISTRY OF WATER RESOURCES 2,880,754,957 2,657,000,000 636,869,000 - 1,261,745,492 MINISTRY OF PUBLIC UTILITIES 4,142,500,449