Norfolk Health Overview and Scrutiny Committee 7 September 2017 Item No 7
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
The Local Government Boundary Commision for England Electoral Review of South Norfolk
SHEET 1, MAP 1 THE LOCAL GOVERNMENT BOUNDARY COMMISION FOR ENGLAND ELECTORAL REVIEW OF SOUTH NORFOLK E Final recommendations for ward boundaries in the district of South Norfolk March 2017 Sheet 1 of 1 OLD COSTESSEY COSTESSEY CP EASTON CP D C This map is based upon Ordnance Survey material with the permission of the Ordnance Survey on behalf of the Controller of Her Majestry's Stationary Office @ Crown copyright. Unauthorised reproduction infringes Crown copyright and may lead to prosecution or civil preceedings. NEW COSTESSEY The Local Governement Boundary Commision for England GD100049926 2017. B Boundary alignment and names shown on the mapping background may not be up to date. They may differ from the latest Boundary information MARLINGFORD AND COLTON CP applied as part of this review. BAWBURGH CP BRANDON PARVA, COSTON, A RUNHALL AND WELBORNE CP EASTON BARNHAM BROOM CP BARFORD CP COLNEY CP HETHERSETT TROWSE WITH LITTLE MELTON CP NEWTON CP SURLINGHAM CP GREAT MELTON CP KIRBY BEDON CP CRINGLEFORD WRAMPLINGHAM CP CRINGLEFORD CP KIMBERLEY CP HETHERSETT CP BIXLEY CP WICKLEWOOD BRAMERTON CP ROCKLAND ST MARY CP KESWICK AND INTWOOD CP PORINGLAND, ROCKLAND FRAMINGHAM FRAMINGHAMS & TROWSE PIGOT CP H CAISTOR ST EDMUND CP H CLAXTON CP NORTH WYMONDHAM P O P C L C M V A E H R R C S E G T IN P O T ER SWARDESTON CP N HELLINGTON E T FRAMINGHAM YELVERTON P T CP KE EARL CP CP T S N O T E G EAST CARLETON CP L WICKLEWOOD CP F STOKE HOLY CROSS CP ASHBY ST MARY CP R A C ALPINGTON CP HINGHAM CP PORINGLAND CP LANGLEY WITH HARDLEY CP HINGHAM & DEOPHAM CENTRAL -
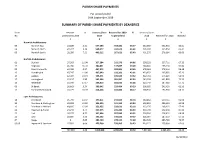
Parish Share Report
PARISH SHARE PAYMENTS For period ended 30th September 2019 SUMMARY OF PARISH SHARE PAYMENTS BY DEANERIES Dean Amount % Deanery Share Received for 2019 % Deanery Share % No Outstanding 2018 2019 to period end 2018 Received for 2018 received £ £ £ £ £ Norwich Archdeaconry 06 Norwich East 23,500 4.41 557,186 354,184 63.57 532,380 322,654 60.61 04 Norwich North 47,317 9.36 508,577 333,671 65.61 505,697 335,854 66.41 05 Norwich South 28,950 7.21 409,212 267,621 65.40 401,270 276,984 69.03 Norfolk Archdeaconry 01 Blofield 37,303 11.04 327,284 212,276 64.86 338,033 227,711 67.36 11 Depwade 46,736 16.20 280,831 137,847 49.09 288,484 155,218 53.80 02 Great Yarmouth 44,786 9.37 467,972 283,804 60.65 478,063 278,114 58.18 13 Humbleyard 47,747 11.00 437,949 192,301 43.91 433,952 205,085 47.26 14 Loddon 62,404 19.34 335,571 165,520 49.32 322,731 174,229 53.99 15 Lothingland 21,237 3.90 562,194 381,997 67.95 545,102 401,890 73.73 16 Redenhall 55,930 17.17 339,813 183,032 53.86 325,740 187,989 57.71 09 St Benet 36,663 9.24 380,642 229,484 60.29 396,955 243,433 61.33 17 Thetford & Rockland 31,271 10.39 314,266 182,806 58.17 300,933 192,966 64.12 Lynn Archdeaconry 18 Breckland 45,799 11.97 397,811 233,505 58.70 382,462 239,714 62.68 20 Burnham & Walsingham 63,028 15.65 396,393 241,163 60.84 402,850 256,123 63.58 12 Dereham in Mitford 43,605 12.03 353,955 223,631 63.18 362,376 208,125 57.43 21 Heacham & Rising 24,243 6.74 377,375 245,242 64.99 359,790 242,156 67.30 22 Holt 28,275 8.55 327,646 207,089 63.21 330,766 214,952 64.99 23 Lynn 10,805 3.30 330,152 196,022 59.37 326,964 187,510 57.35 07 Repps 0 0.00 383,729 278,123 72.48 382,728 285,790 74.67 03 08 Ingworth & Sparham 27,983 6.66 425,260 239,965 56.43 420,215 258,960 61.63 727,583 9.28 7,913,818 4,789,282 60.52 7,837,491 4,895,456 62.46 01/10/2019 NORWICH DIOCESAN BOARD OF FINANCE LTD DEANERY HISTORY REPORT MONTH September YEAR 2019 SUMMARY PARISH 2017 OUTST. -

Norfolk Through a Lens
NORFOLK THROUGH A LENS A guide to the Photographic Collections held by Norfolk Library & Information Service 2 NORFOLK THROUGH A LENS A guide to the Photographic Collections held by Norfolk Library & Information Service History and Background The systematic collecting of photographs of Norfolk really began in 1913 when the Norfolk Photographic Survey was formed, although there are many images in the collection which date from shortly after the invention of photography (during the 1840s) and a great deal which are late Victorian. In less than one year over a thousand photographs were deposited in Norwich Library and by the mid- 1990s the collection had expanded to 30,000 prints and a similar number of negatives. The devastating Norwich library fire of 1994 destroyed around 15,000 Norwich prints, some of which were early images. Fortunately, many of the most important images were copied before the fire and those copies have since been purchased and returned to the library holdings. In 1999 a very successful public appeal was launched to replace parts of the lost archive and expand the collection. Today the collection (which was based upon the survey) contains a huge variety of material from amateur and informal work to commercial pictures. This includes newspaper reportage, portraiture, building and landscape surveys, tourism and advertising. There is work by the pioneers of photography in the region; there are collections by talented and dedicated amateurs as well as professional art photographers and early female practitioners such as Olive Edis, Viola Grimes and Edith Flowerdew. More recent images of Norfolk life are now beginning to filter in, such as a village survey of Ashwellthorpe by Richard Tilbrook from 1977, groups of Norwich punks and Norfolk fairs from the 1980s by Paul Harley and re-development images post 1990s. -
Contents of Volume 14 Norwich Marriages 1813-37 (Are Distinguished by Letter Code, Given Below) Those from 1801-13 Have Also Been Transcribed and Have No Code
Norfolk Family History Society Norfolk Marriages 1801-1837 The contents of Volume 14 Norwich Marriages 1813-37 (are distinguished by letter code, given below) those from 1801-13 have also been transcribed and have no code. ASt All Saints Hel St. Helen’s MyM St. Mary in the S&J St. Simon & St. And St. Andrew’s Jam St. James’ Marsh Jude Aug St. Augustine’s Jma St. John McC St. Michael Coslany Ste St. Stephen’s Ben St. Benedict’s Maddermarket McP St. Michael at Plea Swi St. Swithen’s JSe St. John Sepulchre McT St. Michael at Thorn Cle St. Clement’s Erh Earlham St. Mary’s Edm St. Edmund’s JTi St. John Timberhill Pau St. Paul’s Etn Eaton St. Andrew’s Eth St. Etheldreda’s Jul St. Julian’s PHu St. Peter Hungate GCo St. George Colegate Law St. Lawrence’s PMa St. Peter Mancroft Hei Heigham St. GTo St. George Mgt St. Margaret’s PpM St. Peter per Bartholomew Tombland MtO St. Martin at Oak Mountergate Lak Lakenham St. John Gil St. Giles’ MtP St. Martin at Palace PSo St. Peter Southgate the Baptist and All Grg St. Gregory’s MyC St. Mary Coslany Sav St. Saviour’s Saints The 25 Suffolk parishes Ashby Burgh Castle (Nfk 1974) Gisleham Kessingland Mutford Barnby Carlton Colville Gorleston (Nfk 1889) Kirkley Oulton Belton (Nfk 1974) Corton Gunton Knettishall Pakefield Blundeston Cove, North Herringfleet Lound Rushmere Bradwell (Nfk 1974) Fritton (Nfk 1974) Hopton (Nfk 1974) Lowestoft Somerleyton The Norfolk parishes 1 Acle 36 Barton Bendish St Andrew 71 Bodham 106 Burlingham St Edmond 141 Colney 2 Alburgh 37 Barton Bendish St Mary 72 Bodney 107 Burlingham -

NORTH NORFOLK 2 PCN Pharmacy Lead
North Norfolk PCN Please note this list is subject to change and is provided for Pharmacy Contractors in Norfolk/Suffolk to facilitate the process of organising communication and nomination of PCN Leads. The list is not final and should not be circulated for any purpose other than facilitating the organisation of Pharmacy PCNs/Leads. NORTH NORFOLK 1 PCN Pharmacy Lead: Geoff Ray Clinical Director: Email: [email protected] Contact Details: Pharmacy Details: Kelling Pharmacy, FWK09 GP Practices Pharmacies Holt Medical Practice David Jagger Ltd Sheringham Medical Practice Fakenham Pharmacy Wells Health Centre Kelling Pharmacy The Fakenham Medical Practice Lloyds Pharmacy Sheringham Well Fakenham - Holt Road Your Local Boots Pharmacy Sheringham Your Local Boots Pharmacy Fakenham Your Local Boots Pharmacy Holt NORTH NORFOLK 2 PCN Pharmacy Lead: Carrie Catchpole Clinical Director: Email: [email protected] Contact Details: Pharmacy Details: Boots North Walsham, FK436 GP Practices Pharmacies Cromer Group Practice Coastal Pharmacy Mundesley Medical Centre Cromer Pharmacy Birchwood Surgery Lloyds Pharmacy Cromer Paston Surgery North Walsham Pharmacy Aldborough Surgery Well North Walsham - Market Place Bacton Surgery Your Local Boots Pharmacy Cromer Your Local Boots Pharmacy North Walsham North Norfolk PCN Please note this list is subject to change and is provided for Pharmacy Contractors in Norfolk/Suffolk to facilitate the process of organising communication and nomination of PCN Leads. The list -

North Norfolk District Council (Alby
DEFINITIVE STATEMENT OF PUBLIC RIGHTS OF WAY NORTH NORFOLK DISTRICT VOLUME I PARISH OF ALBY WITH THWAITE Footpath No. 1 (Middle Hill to Aldborough Mill). Starts from Middle Hill and runs north westwards to Aldborough Hill at parish boundary where it joins Footpath No. 12 of Aldborough. Footpath No. 2 (Alby Hill to All Saints' Church). Starts from Alby Hill and runs southwards to enter road opposite All Saints' Church. Footpath No. 3 (Dovehouse Lane to Footpath 13). Starts from Alby Hill and runs northwards, then turning eastwards, crosses Footpath No. 5 then again northwards, and continuing north-eastwards to field gate. Path continues from field gate in a south- easterly direction crossing the end Footpath No. 4 and U14440 continuing until it meets Footpath No.13 at TG 20567/34065. Footpath No. 4 (Park Farm to Sunday School). Starts from Park Farm and runs south westwards to Footpath No. 3 and U14440. Footpath No. 5 (Pack Lane). Starts from the C288 at TG 20237/33581 going in a northerly direction parallel and to the eastern boundary of the cemetery for a distance of approximately 11 metres to TG 20236/33589. Continuing in a westerly direction following the existing path for approximately 34 metres to TG 20201/33589 at the western boundary of the cemetery. Continuing in a generally northerly direction parallel to the western boundary of the cemetery for approximately 23 metres to the field boundary at TG 20206/33611. Continuing in a westerly direction parallel to and to the northern side of the field boundary for a distance of approximately 153 metres to exit onto the U440 road at TG 20054/33633. -

Ludham Character Appraisal Adopted 7 December 2020
Ludham Conservation Area Apprasial August 2020 1 Contents Introduction ............................................................................................................................... 3 Why have conservation areas? ............................................................................................. 3 Aims and Objectives .............................................................................................................. 5 What does designation mean for me? ................................................................................. 5 The Appraisal ............................................................................................................................. 7 Preamble ................................................................................................................................ 7 Summary of Special Interest ................................................................................................. 8 Location and Context ............................................................................................................ 9 General Character and Plan Form ........................................................................................ 9 Geological background ....................................................................................................... 10 Historic Development .............................................................................................................. 12 Archaeology and early development of the Parish .......................................................... -

Parish Registers and Transcripts in the Norfolk Record Office
Parish Registers and Transcripts in the Norfolk Record Office This list summarises the Norfolk Record Office’s (NRO’s) holdings of parish (Church of England) registers and of transcripts and other copies of them. Parish Registers The NRO holds registers of baptisms, marriages, burials and banns of marriage for most parishes in the Diocese of Norwich (including Suffolk parishes in and near Lowestoft in the deanery of Lothingland) and part of the Diocese of Ely in south-west Norfolk (parishes in the deanery of Fincham and Feltwell). Some Norfolk parish records remain in the churches, especially more recent registers, which may be still in use. In the extreme west of the county, records for parishes in the deanery of Wisbech Lynn Marshland are deposited in the Wisbech and Fenland Museum, whilst Welney parish records are at the Cambridgeshire Record Office. The covering dates of registers in the following list do not conceal any gaps of more than ten years; for the populous urban parishes (such as Great Yarmouth) smaller gaps are indicated. Whenever microfiche or microfilm copies are available they must be used in place of the original registers, some of which are unfit for production. A few parish registers have been digitally photographed and the images are available on computers in the NRO's searchroom. The digital images were produced as a result of partnership projects with other groups and organizations, so we are not able to supply copies of whole registers (either as hard copies or on CD or in any other digital format), although in most cases we have permission to provide printout copies of individual entries. -

Georgeloydsophiabanham.Pdf
BULLEN chart (c2) My genealogy index page is: http://cashewnut.me.uk/Genealogy/ George Sophia m. 1835, Aslacton LORD ........................... LOYD ........................... LLOYD ALA CASH - web pages Descendants LOYD Margaret's parents were James SMITH, house painter and plasterer, Eliza'a baptism is recorded on and wife Sarah. Both were born in Bury. According to the 1851 and 1861 The marriage of Caroline's parents was registered in 1856 between home page: http://cashewnut.me.uk of Although the spelling in the 1863 marriage record (GRO) is Elviner, BAHAM See BULLEN chart (c) for (LORD) 11 Mar 1838 as Eliza LORD The ancestral name for this family was LORD according to baptismal censuses William's parents were Robert LISTER & Dinah COLLINGS. George LOYD I have used the more usual spelling. the ancestry of George LOYD daughter of George & Sophia (IGI). records for earlier generations. For some branches, the spelling This couple are possibly to be identified with the marriage recorded Birth entry in GRO (2nd quarter 1851, Benjamin & Ann KALLAWAY b. 1808, Long Stratton St Mary, Norfolk I cannot find a birth registration and b. 1814, Moulton, Norfolk changed during the nineteenth century to LOYD and then LLOYD. in the IGI of James SMITH and Sarah BUCKLEY at St Mary Radcliffe, Depwade reg-district) has the name (various spellings) both born in Caroline's birth was registered (1861 GRO) as Caroline LESTER. I think Elvina cannot have been the daughter of Sophia who would d. 1882, Forncett St Peter in the GRO. Her GRO marriage Sophia BANHAM d. 1898, Forncett St Peter On this chart I have used the surname spelling entered in the GRO Bury, 19 Feb 1837. -

Wicklewood Map Book
Hardingham Kimberley GNLP0525 GNLP0006 GNLP0232 GNLP0535 Hingham Wicklewood Wymondham GNLP0577 GNLP0249 Deopham GNLP0507 GNLP0354 GNLP0032 GNLP0402 Morley GNLP0515 GNLP0403 © Crown copyright and database rights 2017 Ordnance Survey 100019340 GNLP0515 GNLP0320 Date created: Legend 31-03-2017 Greater Norwich Local Plan Wicklewood ParishesBoundary 1:28,392 This map was made by the Norfolk County Council Information Exploitation Team [email protected] ± D OA HACKFORD R Wicklewood GNLP0577 T H E G R E E N © Crown copyright and database rights 2017 Ordnance Survey 100019340 Date created: Wicklewood 31-03-2017 Greater Norwich Local Plan GNLP0577 Legend 1:2,000 This map was made by the Norfolk County Council Information Exploitation Team [email protected] Land to the south of Wicklewood Primary School Parish Boundary ± H IL LS ID E CRESCENT E N A L H C R U H C Wicklewood GNLP0535 © Crown copyright and database rSigChLtsO S2E017 Ordnance Survey 100019340 SAINT ALL Date created: Wicklewood 31-03-2017 Greater Norwich Local Plan GNLP0535 Legend 1:2,000 This map was made by the Norfolk County Council Information Exploitation Team [email protected] Land to the south of Church Lane Parish Boundary ± D LA A DY RO S LAN CAVICK E K DEC YKE Wicklewood D HIGH E OAK D N ROA A L L O S W N P R A RES TON AVENUE O M A D D A E R V B I GNLP0354 R ABBE ROAD D Wymondham Y T U N T S E AD H RO C DON LON AD RO ON D E N N O L A L N O E T N U S A L L L A H E L © Crown copyright and database rights 2017 Ordnance Survey 100019340 IL V N O G GNLP0320 Date created: Wicklewood -

Swan Field, Hardingham Road, Hingham
Vision and Delivery Document Swan Field, Hardingham Road, Hingham CONTENTS |1.0| Introduction 4 |2.0| Planning Context 8 |3.0| The Site in Context 12 |4.0| Development Opportunity 26 |5.0| Opportunities and Constraints 30 |6.0| Masterplan Strategy 34 |7.0| Delivery & Competition 42 |8.0| Conclusion 50 Published February 2020 Swan Field, Hardingham Road, Hingham | 3 View south towards the site and Hingham from FP3 1.0 Introduction Swan Field, Hardingham Road, Hingham | 5 1.0 Introduction Lanpro Services is instructed by Hardingham Farms The document does this through: Limited to assist in the promotion of a development of up to 70 homes at Swan Field, Hardingham Road, • Setting out the planning context within which Hingham through the emerging Local Plan process. these representations are submitted; The site is located within South Norfolk District, • Assessing the site’s capacity to accommodate new and as such, this document is prepared to inform development (against a series of environmental discussions with the local planning authority and the and social criteria); continued promotion of the site through the Greater Norwich Local Plan process. The site has previously • Comparing the site’s deliverability against been submitted through the ‘Call for Sites’ process competing sites in the locality; and is identified as site GNLP0554R. • Setting out the vision and key development The site, comprising 3.9 hectares, lies immediately principles for the site (including the water to the northeast of Hingham, 7km to the north of positive development); -

STATEMENT of PERSONS NOMINATED Election of Parish
STATEMENT OF PERSONS NOMINATED North Norfolk Election of Parish Councillors The following is a statement of the persons nominated for election as a Councillor for Aldborough and Thurgarton Reason why Name of Candidate Home Address Description (if any) Name of Proposer no longer nominated* BAILLIE The Bays, Chapel Murat Anne M Tony Road, Thurgarton, Norwich, NR11 7NP ELLIOTT Sunholme, The Elliott Ruth Paul Martin Green, Aldborough, NR11 7AA GALLANT Spring Cottage, The Elliott Paul M David Peter Green, Aldborough, NR11 7AA WHEELER 4 Pipits Meadow, Grieves John B Jean Elizabeth Aldborough, NR11 7NW WORDINGHAM Two Oaks, Freeman James H J Peter Thurgarton Road, Aldborough, NR11 7NY *Decision of the Returning Officer that the nomination is invalid or other reason why a person nominated no longer stands nominated. The persons above against whose name no entry is made in the last column have been and stand validly nominated. Dated: Friday 10 April 2015 Sheila Oxtoby Returning Officer Printed and published by the Returning Officer, Electoral Services, North Norfolk District Council, Holt Road, Cromer, Norfolk, NR27 9EN STATEMENT OF PERSONS NOMINATED North Norfolk Election of Parish Councillors The following is a statement of the persons nominated for election as a Councillor for Antingham Reason why Name of Candidate Home Address Description (if any) Name of Proposer no longer nominated* EVERSON Margra, Southrepps Long Trevor F Graham Fredrick Road, Antingham, North Walsham, NR28 0NP JONES The Old Coach Independent Bacon Robert H Graham House, Antingham Hall, Cromer Road, Antingham, N. Walsham, NR28 0NJ LONG The Old Forge, Everson Graham F Trevor Francis Elderton Lane, Antingham, North Walsham, NR28 0NR LOVE Holly Cottage, McLeod Lynn W Steven Paul Antingham Hill, North Walsham, Norfolk, NR28 0NH PARAMOR Field View, Long Trevor F Stuart John Southrepps Road, Antingham, North Walsham, NR28 0NP *Decision of the Returning Officer that the nomination is invalid or other reason why a person nominated no longer stands nominated.